Introduction
One-lung ventilation (OLV) is a commonly used technique in thoracic surgeries. In thoracic surgeries performed with OLV, there may be changes in cerebral tissue oxygenation depending on both patient position and anesthetic technique. The effect of cerebral hypoxia on post-operative cognitive functions is controversially. Despite the ISPOCD1 study in which concluded that, there was no relationship between the cerebral hypoxy and post-operative cognitive dysfunction (POCD) regional cerebral oxygen saturation decrements during surgery which is listed among the POCD1-4. Therefore, anesthetic techniques affecting lung mechanics and cerebral tissue oxygenation may affect cognitive functions as well.
When OLV begins, alveolar hypoxia and arteriovenous shunt of deoxygenated blood occur in the dependent lung. And then, hypoxic pulmonary vasoconstriction (HPV) in non-ventilated lung segments occurs with increased mechanical stress. This event leads to significant physiological changes in cardiac output and pulmonary and systemic pressures5.
In OLV, the propofol-based total intravenous anesthesia (TIVA) and inhalation general anesthesia techniques are frequently used. Recent studies have shown that unlike inhalational anesthetics, propofol does not suppress HPV, indeed increases it6,7. Inhalational anesthetic agents reduce cardiac output more than oxygen consumption, causing a decrease in mixed venous partial pressure of oxygen, which stimulates HPV. In this way, especially dose of more than 1 MAC, HPV is inhibited8.
Hypoxemia underlies many mechanisms that cause a disruption in cerebral tissue oxygenation. Moreover, hemodynamic changes that affect the perfusion of the brain and other organs are also important9. Studies have shown significant reductions in cerebral oxygen saturation in thoracic surgery as a result of severe oxidative stress due to prolonged OLV and hypoxemia due to decreased functional residual capacity of the ventilated lung in the lateral decubitus position10,11. It is also likely that decreased oxygen saturation affects post-operative cognitive functions.
Cerebral oximetry is a method used to monitor the cerebral oxygen distribution-consumption balance and regional oxygen saturation (rSO2) in a limited area of the frontal cortex by noninvasively and continuously combining arterial and venous oxygen saturation signals of near-infrared spectroscopy (NIRS), which is a technique developed in the 1970s. Thanks to this method, perioperative physiological conditions, optimal tissue oxygenation, and end-organ functions can be interpreted9,12.
The aim of this prospective study was to compare the potential effects of TIVA and inhalation general anesthesia techniques on cerebral tissue oxygenation and post-operative cognitive functions in patients receiving one-lung ventilation in thoracic surgery.
Materials and methods
The study was approved by the regional or institutional review boards according to national guidelines for approval of registry studies and was registered at http://www.clinicaltrials.gov (NCT04760262). This study was prospectively conducted on a total of 60 patients aged 18-80 years in the ASA I-III risk group who would undergo thoracic surgery with one-lung ventilation (OLV) for more than 45 min by obtaining Local Ethics Committee Approval and informed consent. The exclusion criteria were determined as severe metabolic, renal, hepatic, central nervous system diseases, alcohol or drug addiction, multiple trauma, coagulopathy, cerebral disease, dementia, hearing impairment and imperception, and severe obesity (a body mass index (BMI) of ≥ 35). It was also planned to exclude patients with a peripheral oxygen saturation below 90 during OLV. Mini-mental state examination (MMSE) was used to evaluate the cognitive functions of the patients. The maximum MMSE score was determined as 30, and a score below 23 was considered abnormal. The MMSE of all patients was repeated at the latest 1 day before the surgery and at the post-operative 3rd and 24th h to evaluate cognitive functions. It was also planned to exclude patients with a pre-operative MMSE score below 23. New patients were recruited in place of patients who were excluded for any reason to reach the planned sample size.
The patients, who were transferred to the operating room and whose electrocardiography, non-invasive blood pressure, and peripheral oxygen saturation (spO2) were monitored, were inhaled 3 l/min of oxygen with a face mask. After the sedation with 1-2 mg intravenous midazolam, an epidural catheter was placed in the patients at the level of T4-5 or T5-6. Bispectral index (BIS) monitoring was performed on the patients whose invasive blood pressure was monitored by the radial artery catheter to follow-up the depth of anesthesia. To measure the cerebral oxygen saturation values of both hemispheres, the fiberoptic sensors of the INVOS 1500C (Covidien, CO, USA) cerebral oximetry device were placed on the right and left sides of the foreheads of the patients.
The first rSO2 values of the patients were measured during spontaneous breathing while breathing 3 l/min of oxygen with a face mask and recorded as basal value. According to this basal value measured, a decrease of more than 20% in rSO2 was considered cerebral oxygen desaturation and recorded.
All patients' age, gender, and ASA score were recorded. Surgery time, duration of OLV and performed surgical procedure was also noted. The hemodynamic values (mean arterial pressure and heart rate), spO2, and rSO2 values (both hemispheres of patients) were recorded before anesthesia induction (basal), at 5 min intervals throughout the surgical procedure, and after extubation.
The solution prepared as 2 mg/ml bupivacaine was initiated at a constant rate of 4mL/h through the epidural catheter before anesthesia induction and the infusion was maintained until the post-operative 48th h. During the anesthesia induction, the patients were intravenously administered 2-3 mg/kg propofol, 1-2 mg/kg fentanyl, and 0.6 mg/kg rocuronium and the endotracheal intubation procedure was performed using a left double-lumen endobronchial tube and the location of the tube was confirmed by a fiberoptic bronchoscope. The patients were randomly divided into two groups as Group T (n = 30) whose anesthesia was maintained with TIVA (intravenous 125-250 mg/kg/min propofol + 0.1-0.25 mg/kg/min remifentanil infusion) and Group I (n = 30) whose anesthesia was maintained with inhalation (a sevoflurane concentration of 1-2% in 50-50% O2-air mixture). Randomization was performed before group assignment using computer-assisted random numbers from www.randomization.com. The doses of anesthetic drugs used in the patients were adjusted to maintain the depth of anesthesia at BIS values between 40 and 60.
The ventilation of all patients was provided in volume-controlled ventilation mode by adjusting the respiratory rate that would maintain a tidal volume of 6-8 ml/kg and an EtCO2 value of 30-35 mmHg so that the peak airway pressure did not exceed 30 cmH2O. During OLV, low tidal volume (4-5 ml/kg) and PEEP (6-8 cmH2O) were performed with 14-18/min ventilator frequency as a strategy of lung protection. The maintenance of the muscle relaxant was provided with additional doses of 0.25 mg/kg rocuronium depending on neuromuscular monitoring response.
Considering the surgical site, the patient was placed in the right or left lateral decubitus position. During the one-lung ventilation, spO2 was tried to be kept above 90%. When SpO2 decreased below 90%, a continuous oxygen insufflation of 1-2 l/min was administered to the non-ventilated lung. However, when there was no improvement despite that, it was planned to terminate one-lung ventilation and switch to two-lung ventilation and exclude these patients from the study. The EtCO2 and paCO2 values of the patients were regulated by respiratory frequency. Although post-operative analgesia was maintained with constant infusion through the epidural catheter, in the case of a numeric rating scale of >3 in the pain assessment, it was planned to administer bolus doses of 4 ml through the epidural catheter by closely monitoring the hemodynamic parameters.
The Statistical Package for the Social Sciences (SPSS Inc., Chicago, IL, USA) v21.0 was used for the statistical analysis of the data obtained in the study. The SPSS Statistics software package was used for the statistical analyses of the results obtained in the study. In addition to the descriptive statistics (frequency, percentage, mean, and standard deviation), the Kolmogorov–Smirnov test was used to test for normality distribution when evaluating the study data.
The Pearson Chi-square test and the Fisher's exact test were used to compare the nominal data. The Mann–Whitney U-test was used for the intergroup comparison of the quantitative parameters in the case of two groups. The Wilcoxon signed-rank test was used for the intragroup comparison of the parameters. Spearman's correlation analysis was used to analyze the correlation between the presence of desaturation and MMSE measurements and age. The power of a sample size of 60 cases, 30 in each group, was calculated to be 90.5%. The results were evaluated at 95% confidence interval and the level of significance of p < 0.05.
Results
The study included a total of 66 patients. Since the MMSEs of two patients could not be evaluated postoperatively and four patients required conversion to two-lung ventilation due to impaired intraoperative oxygenation, they were excluded from the study. The patients excluded from the study were equal in both groups. The data were analyzed through 60 patients. There was no significant difference between the groups in terms of the data of the patients and surgical procedures (p > 0.05) (Table 1). There was no significant difference between the groups in terms of heart rate, mean arterial pressure, peripheral oxygen saturation, and BIS scores (p > 0.05).
Table 1 Patients' general characteristics and intraoperative data
| Parameter | Group T (n = 30) | Group I (n = 30) |
|---|---|---|
| Age | 57.3 ± 12.3 | 57.6 ± 12.6 |
| Gender (F/M) | 9/21 | 13/17 |
| BMI (kg/m2) | 26.5 ± 3.2 | 26.1 ± 2.9 |
| ASA I/II/III (n) | 12/10/8 | 10/12/8 |
| Operation time (min) | 137.25 ± 45.2 | 139.56 ± 35.4 |
| OLV time (min) | 89.7 ± 35.1 | 90.9 ± 26.6 |
| Type of surgery | ||
| Lobectomy (n) | 21 | 22 |
| Chest wall resection (n) | 5 | 4 |
| Pneumonectomy (n) | 4 | 4 |
| Thoracotomy (n) | ||
| Right | 18 | 16 |
| Left | 12 | 14 |
Data of patients are expressed as numbers, mean ± standard deviation. BMI; body mass index. ASA; American Society of Anesthesiologists, OLV; One-Lung Ventilation, M; Male, F; Female.
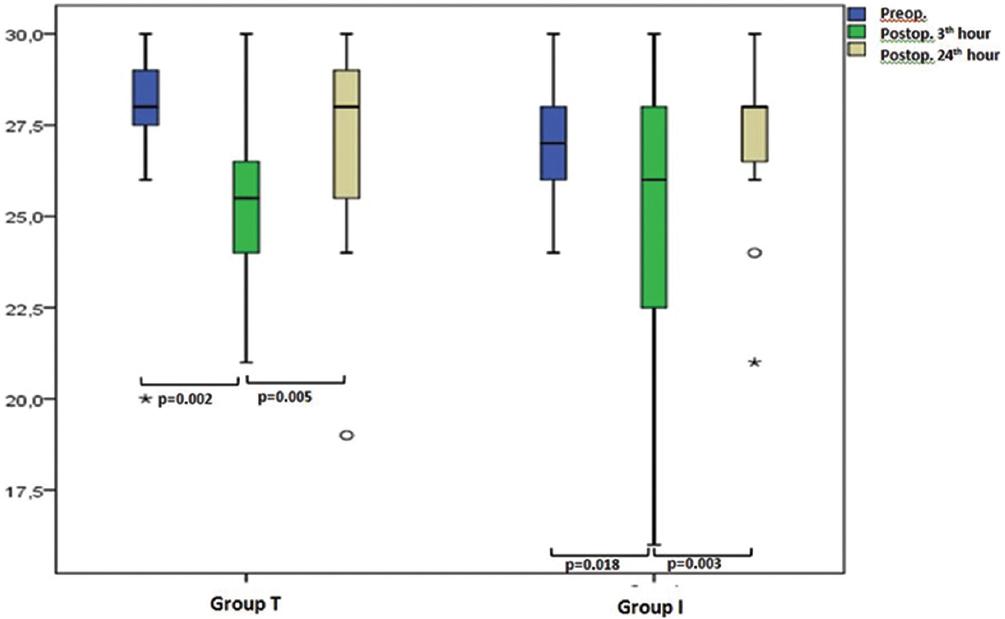
The number of patients in the groups who exhibited a decrease in rSO2 compared to the basal values and the rates of decrease are shown in figure 1. As is seen in figure, there were certain reductions in rSO2 in all patients received OLV. In Group T, the rate of patients (15 patients, 50%) who exhibited a decrease of more than 20% in rSO2 compared to the basal values, in which we considered clinically significant, was higher than Group I (ten patients, 33.3%), (p < 0.05) (Fig. 1).
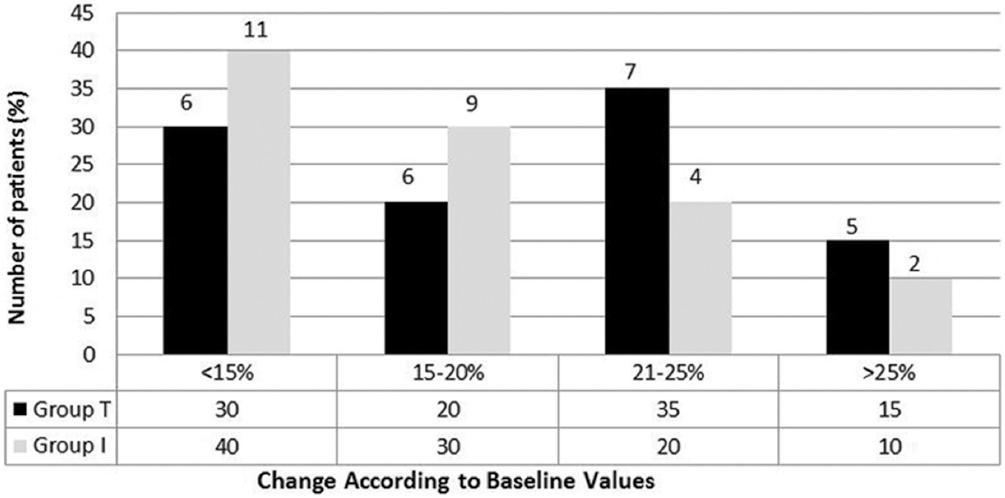
Figure 1 The rate of decrease in rSO2compared to baseline values and the change in number of patients
Of the patients who underwent right thoracotomy, 10 (33%) had desaturation in the left hemisphere of the brain, while 4 (13%) of the patients who underwent left thoracotomy had desaturation. This difference was statistically significant (p = 0.044) (Table 2). When the left cerebral oxygenation values of the groups in the follow-up periods were compared, the left cerebral oxygenation values of Group I were significantly higher than that of Group T at 10 min, 15 min, 20 min, 25 min, 30 min, 35 min, 40 min, 45 min, and 50 min of OLV (p < 0.05), (Fig. 2). There was no significant difference between the right cerebral oxygenation values of the groups.
Table 2 The correlation between the presence of desaturation and the right-left thoracotomized lung segments
| Right thoracotomy (n = 34) | Left thoracotomy (n = 26) | p | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Presence of desaturation left rSO2 | 10 | 35 | 4 | 5 | 0.044 |
| Presence of desaturation right rSO2 | 6 | 25 | 4 | 15 | 0.472 |
Data of patients are expressed as numbers and rate.
There was no significant difference between the groups in the comparison of pre-operative, post-operative 3-h and 24-h MMSE scores (p > 0.05) (Table 3). There was a significant decrease in the post-operative 3-h MMSE scores of the patients in Group T and Group I compared to the pre-operative period (p = 0.002, p = 0.018, respectively). The change in the post-operative 24-h scores was not statistically significant compared to the pre-operative scores. In addition, the increase in the post-operative 24-h MMSE values of the groups compared to the post-operative 3-h MMSE values was statistically significant (p = 0.005, p = 0.003, respectively) (Fig. 3).
Table 3 MMSE changes of the groups
| Group T (n = 30) | Group I (n = 30) | p | |
|---|---|---|---|
| Pre operative | 27.90 ± 2.12 | 27.46 ± 1.46 | 0.53 |
| Post operative 3th h | 25.32 ± 2.43 | 25.22 ± 3.72 | 0.95 |
| Post operative 24th h | 26.25 ± 0.85 | 27.55 ± 1.43 | 0.73 |
Data of patients are expressed as mean ± standard deviation.
There was no significant correlation between the presence of desaturation and MMSE scores and age (p > 0.05).
Discussion
This study demonstrated that inhalation general anesthesia provided better cerebral tissue oxygenation in thoracic surgeries with one-lung ventilation. TIVA, on the other hand, showed a statistically significant decrease compared to the baseline values in the same patient groups and had a negative effect on oxygenation. Decreases in cerebral oxygenation were observed especially in the left cerebral hemisphere of the patients who underwent right thoracotomy. However, decreases in intraoperative cerebral oxygenation were not reflected on the post-operative clinical condition and there was no difference between the groups in terms of MMSE.
Hypoxemia, which was much more common in OLV in previous years, has considerably decreased with the use of fiberoptic bronchoscopy in intubation and ventilation and the development of new airway devices13. However, tissue oxygenation impairments that may negatively affect post-operative cognitive functions still remain. In thoracic surgeries performed with OLV, alveolar hypoxia cause HPV and pulmonary vascular resistance increase in the non-ventilated lung. With the shunt of deoxygenated blood, an increase occurs in alveolar-arterial oxygen gradient. As a result of reduced functional residual capacity and intraoperative pulmonary ischemia reperfusion, various cytokines are released and a systemic inflammatory response develops14. In consequence of all these, hypoxemia and associated clinical pathologies may be seen. The brain is one of the organs very sensitive to hypoxia and most affected by these changes.
The anesthetic technique and anesthetic drugs used in thoracic surgeries with OLV can also effect cerebral tissue oxygenation. They have different effects on potential hypoxemia in OLV. While inhalational anesthetics have the ability to inhibit HPV, intravenous anesthetics do not have a reducing effect on HPV. Contrary to the results of our study, this leads to the expectation of better tissue oxygenation in patients receiving TIVA. However, it is known that the concentration of alveolar pro-inflammatory cytokines increases in surgeries performed with OLV, especially in the ventilated lung. This inflammatory response developed negatively affects tissue oxygenation. Despite the study conducted by Akyol et al.15, in which propofol seem to be effective in protecting against lung injury caused by increased oxidative stress, some studies have shown that inhalational anesthetics exhibit a cytoprotective effect, inhibiting this inflammatory response more than intravenous anesthetics, which reduces post-operative complications16-19. The study by Erturk et al. investigating the effects of inhalational and intravenous anesthetic agents on oxidative stress in thoracic surgeries performed with OLV found that inhalation anesthesia using sevoflurane produced more positive results by suppressing oxidative stress20. Cytoprotective effect of sevoflurane may contribute to get better cerebral tissue oxygenation in our study.
Cardiac output (CO), along with cerebral blood flow (CBF) and cerebral metabolic rate of oxygen (CMRO2), are some of the important factors that affect brain tissue oxygenation. Increased CBF/CMRO2 ratio allows for better cerebral tissue oxygenation. Both sevoflurane and propofol significantly decrease CMRO2, while propofol tends to reduce CBF more than sevoflurane. The study by Guclu et al. investigating the effects of sevoflurane and TIVA on cerebral tissue oxygenation with NIRS measurement showed that sevoflurane reduced global cerebral blood flow and more significantly CMRO2 with its dose-dependent vasodilator effect, thereby providing higher NIRS values compared to TIVA21. Guo et al. who similarly investigated the effects of propofol and sevoflurane on abdominal surgery patients showed that high-dose propofol further reduced CBF, while sevoflurane increased CBF/CMRO2 ratio and increased cerebral oxygenation22. In our study, a decrease of more than 20% in rSO2, in which we considered a statistically significant value, was observed in 30% of the patients in the inhalation group, while this decrease reached up to 50% in the TIVA group. These positive effects of sevoflurane on CBF and CMRO2 might have contributed to achieve better rSO2 values in the inhalation group.
The study by Erol et al. investigating the effect of lateral decubitus position and OLV on CBF in thoracic surgery with carotid blood flow measurement found that there was no significant difference before or after OLV and between supine and lateral decubitus positions23. However, it has been reported that there is no more than 10% decrease in rSO2 in thoracic surgery, but desaturation is higher when OLV is performed11. In their study, Slinger et al. reported that hypoxemia was more common in patients undergoing right thoracotomy, and that right thoracotomy could be considered as a predicting factor in thoracic surgery24. The study by Hummerling et al. investigating the oxygenation difference between both cerebral hemispheres in the lateral decubitus position in thoracic surgery found that the oxygenation of the upper hemisphere was higher in 56% of patients25. This difference was explained by deoxygenation in the lateral decubitus position and changes in venous pressure. In our study, the patients who underwent right thoracotomy showed a higher decrease in rSO2 and the intraoperative tissue oxygenation of the upper, in other words the right hemisphere, was better than that of the lower left hemisphere, which supports these two studies.
However, the reason for decreases in rSO2 during OLV could not be fully understood. In their studies on cardiac surgery patients, Paquet et al. showed a correlation between mean pulmonary artery pressure and mean rSO2 values and stated that the increase in pulmonary pressure caused by OLV could reduce rSO2 by decreasing CO26. In our study, we found reductions in rSO2 in both groups. We can also explain the lower decrease in rSO2 and better cerebral tissue oxygenation in the inhalation group by the fact that sevoflurane partially prevented the increase in pulmonary artery pressure by inhibiting HPV and positively contributing to CO.
Monitoring of peripheral oxygen saturation and partial oxygen pressure in blood gas is not sufficient to assess the adequacy of cerebral perfusion and tissue oxygenation27. NIRS is a method used for the monitoring of tissue oxygenation, as well as the detection of cerebral desaturation in recent years as it measures rSO2 values as accurately as invasive techniques28. The incidence of cerebral desaturation can vary between 28-70% in the studies conducted on thoracic surgery, because the baseline control values compared are very different27,29,30. In the light of recent studies, we took the pre-operative rSO2 values obtained while spontaneous breathing with 3 l/min of oxygen with a face mask before anesthesia induction as the control value in this study. We considered a decrease of more than 20% in rSO2 compared to the control value as desaturation.
The development of POCD due to intraoperative cerebral hypoperfusion after general anesthesia is always possible, particularly in elderly patients. It has been reported that this risk can rise up to 25% in patients over 60 years of age 1 week after surgery31,32. MMSE is an easy-to-apply test that is commonly used to evaluate cognitive functions. We also used this test to evaluate the post-operative cognitive functions of our patients.
In their study, Tang et al. investigated the correlation between cerebral oxygenation and POCD in thoracic surgeries performed with OLV on patients 60 years and older and found that rSO2 was decreased by more than 25% compared to control values in one third of patients29. They also found that approximately one-third of the patients included in the study developed POCD at the 3rd post-operative h, but 90% of these patients achieved their normal cognitive functions 24 h after surgery. In our study, although more significantly in the TIVA group, the rSO2 values decreased during OLV in both groups. As a result, we found significant reductions in the MMSE scores of both groups at the 3rd post-operative h compared to the pre-operative values. However, the cognitive dysfunctions of the patients in both groups returned to normal at the post-operative 24th h.
In their study investigating the effect of rSO2 on POCD development, Lin et al. indicated increased age and significant decreases in rSO2 as an important risk factor3. They also stated that a decrease of more than 11% in rSO2 was effective in predicting cognitive impairment. In a multicenter study of 1218 patients over 60 years of age who underwent non-cardiac surgery, the incidence of POCD was 25.8% in the early period and decreased over time. In the same study, it was reported that there was a significant correlation between advanced age and POCD.1 In another study, De Tourney Jette et al. investigated the correlation between the decrease in intraoperative rSO2 and early and late POCD development in patients over 65 years of age who underwent CABG surgery33. They found in their study that the risk of developing POCD in the early period was increased by 7.69 in patients with up to 50% decreases in rSO2, and in decreases up to 30%, POCD occurred as late as 1 month and 3.32 times more likely. Despite the difference in rSO2 values between the groups in our study, there was no significant difference in terms of MMSE scores. This may be due to the fact that the mean age of the patients included in the study was not very high and they were relatively younger so that it was not clinically reflected on the MMSE scores.
Patients undergoing thoracic surgeries tend to stay in PACU longer than other patients due to the requirement for recovery and pain control. High-dose opioids may be needed to control the severe pain of these patients. High-dose opioid can negatively affect both patients' recovery and ability to cooperate in the early period. To obtain more reliable results in our study, we preoperatively placed an epidural catheter in all of our patients and eliminated the misleading effect of opioid use by providing pain control with a local anesthetic.
In conclusion, inhalation general anesthesia provided better cerebral tissue oxygenation in thoracic surgeries performed with OLV compared to TIVA. Further studies are needed to more clearly demonstrate the effects of this positive effect on POCD development and another clinical course.
Study limitations
Our study has some limitations. First, to get an actual conclusion in such a study, the number of patient were small, and patients were relatively young. POCD occurs especially in elderly patient groups. The mean age of our patients was 57 years. If we had studied in older patient groups, we could have achieved different MMSE levels. Second, it may be concluded that the NIRS monitors a small portion of the brain, and may has a high negative predictive value. Since rSO2 was used in many studies in the literature, we also used NIRS to evaluate cerebral oxygenization. Tertiary, we only evaluated POCD using MMSE at the post-operative 24th h at the latest. This may be accepted as an early period for such a study. We could have achieved more reliable results if we had evaluated the patients in the later periods, such as after a week and a month. Finally, the results of MMSE may slightly differ depending on the educational levels of the patients since the same questions were frequently repeated and could be remembered in the early period. We did not analyze the educational levels of our patients.











 nova página do texto(beta)
nova página do texto(beta)