Introduction
Laparoscopic Roux-en-Y gastric bypass (RYGB) has been the most common bariatric surgical procedure for many years, but it is less preferred after the definition of sleeve gastrectomy (SG)1. Despite the successful results of bariatric surgery in the treatment of weight loss and obesity-related comorbidities, recurrence of some comorbidities such as weight gain, type 2 diabetes, and surgery-related complications can be seen2. There is more than one opinion about defining the success of bariatric surgery. Although one of these “Reinhold criteria” defines perfect post-operative weight loss as BMI <30 kg/m2, many centers accept “more than 50% weight loss (EWL)” as a success criterion3,4.
With the reporting of long-term results of bariatric procedures, the inability to lose enough weight after RYGB is a difficult problem to answer. Indications for revision of RYGB to another procedure or normal anatomy are extremely rare; persistent nausea, severe dumping syndrome, cachexia, psychological problems, chronic pain, recurrent anastomotic ulcers, and resistant neuroglycopenia are some of them5. Surgical treatment options in this regard; forming a smaller gastric pouch, narrowing the gastrojejunal anastomosis, placing an adjustable band in the gastric pouch, and transforming it into a different bariatric procedure6.
Little is known about the long-term consequences of RYGB revisions. In this study, we aimed to present the results of our patients who switched from RYGB to SG due to inadequate weight loss and to present the summary of the literature.
Case presentation
Pre-operative preparation
All patients were evaluated preoperatively by a team of dieticians, psychiatrists, endocrinologists, and surgeons. Emotional and behavioral reasons for the failure of the first surgery were excluded from the study. All patients were examined with the upper gastrointestinal endoscopy and IV contrast-enhanced abdominal CT to exclude reasons for technical failure. All aspects of the surgery were explained to the patients, and the consent form was signed by all patients. Compression stockings were worn preoperatively in all patients.
Surgical technique
Each patient was placed in the supine position, with the surgeon on the right, and the assistant and camera on the left. The abdomen was inflated with a Veress needle from the left upper quadrant (palmer point). The camera port was placed at different points in three patients whose first surgery was open surgery. Four standard ports for RYGB and one port for liver retraction were placed. The left liver lobe was retracted from the epigastric port with a Nethenson retractor. The adhesions between the gastric pouch and liver and between the gall bladder and the remnant stomach were dissected. Gastrojejunostomy was found and the gastric sac was separated with a green cartridge just above the anastomosis. Afterward, anastomosis was performed with a linear stapler between the gastric pouch and the remnant stomach. The gastrocolic and gastrosplenic omentum was separated from the great curvature of the stomach, starting 6 cm proximal to the pylorus, up to the left diaphragmatic crus. The 34 Fr bougie was passed into the stomach through the gastrogastric anastomosis. The stomach was shaped into a tube with green and then blue cartridges. The entire fundus and part of the stomach corpus were resected through the bougie. The entire staple line was sutured with a 3-0 prolene suture. Methylene blue leak test was done. A drain was placed in all patients. The jejunal part of the gastrojejunostomy anastomosis created in the previous surgery was not resected in any patient.
Follow-up data of patients
The demographic, RYGB, and revision surgery data of our patients are summarized in tables 1 and 2. None of our patients developed surgical complications after RYGB. Revision surgery was decided on due to insufficient weight loss at the end of follow-up. Feeding jejunostomy, etc., was not added to the revision surgery, oral intake was started on the 2nd post-operative day.
Table 1 Demographic data
| Patient no | Sex | Age (y) | Pre RYGB BMI (kg/m²) | RYGB Lap/Open | Post RYGB min BMI | Follow-up (m) | Pre Revision BMI | Pre Rev EWL |
|---|---|---|---|---|---|---|---|---|
| 1 | F | 55 | 52.8 | Open | 32.5 | 123 | 44.7 | 29 |
| 2 | F | 54 | 55.5 | Lap | 29 | 118 | 40.2 | 50 |
| 3 | F | 47 | 58.3 | Open | 34.5 | 105 | 48.75 | 29 |
| 4 | F | 33 | 43.5 | Open | 13.6 | 80 | 40 | 17.6 |
| Average | 47.25 ± 10.14 | 52.52 ± 6.42 | 27.4 ± 9.47 | 106.5 ± 19.22 | 43.41 ± 4.16 | 31.4 ± 13.51 |
Table 2 Revision operation data and post-revision follow-up results
| Patient no | Lap/Open | Op Time (min) | Bleeding (ml) | Per-operative Complication | Post-operative Complication | LOS (day) | Follow up (m) | Last BMI | EWL | Mortality |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Lap | 300 | 50 | N | Leakage | 25 | 7 | 32.4 | 72.4 | Y |
| 2 | Lap | 300 | 230 | N | N | 6 | 20 | 34.1 | 70 | N |
| 3 | Lap | 385 | 100 | N | Leakage, Bleeding | 10 | 20 | 35.4 | 68.7 | N |
| 4 | Lap | 500 | 50 | N | N | 5 | 22 | 28.7 | 88 | N |
| Average | 371.25 ± 94 | 107.5 ± 85 | 11.5 ± 9.25 | 17.25 ± 6.89 | 32.65 ± 2.9 | 74.77 ± 8.94 |
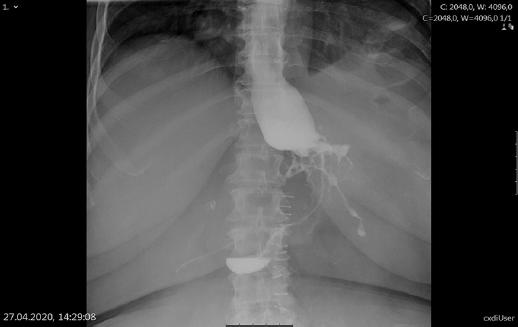
After revision surgery, the patient number 1 developed a gastric fistula, and she needed repeat surgery on the 3rd post-operative day. The openings in the stapler line were sutured, gastrostomy and feeding jejunostomy were placed. Gastric fistula persisted (Fig. 1). During follow-up, stenosis developed in the gastrogastric anastomosis, and no response was obtained for endoscopic dilatation sessions and stent placement (Figs. 2 and 3). After subtotal gastrectomy in the 6th post-operative month after SG, the patient who developed a leak from the gastroenterostomy anastomosis died on the post-operative 44th day due to viral pneumonia (COVID 19).
The patient number 3 presented again on the 12th day after revision surgery with gastrointestinal system bleeding and gastric fistula (non-operative managed).
Discussion
Revision surgery is needed due to inability to lose weight, regain weight, or complications. 15-35% of the patients fail to lose weight and the revision rate is 4.5%7,8. In addition to inadequate weight loss, some RYGB complications such as persistent nausea, severe dumping syndrome, cachexia, psychological problems, chronic pain, recurrent anastomotic ulcers, and refractory neuroglycopenia require revision.
Various revision options after unsuccessful RYGB have been presented in the literature. Mechanism of revision surgery; It is based on return to normal anatomy and restructuring of restrictive or non-absorbent components. Return to normal anatomy is frequently preferred in patients undergoing revision surgery due to complications. There is not enough data in the literature regarding weight status after reversal of RYGB, but it has been reported that patients in need of revision after jejunoileal bypass or gastric band regain their weight in long-term follow-up9,10. Restriction can be increased surgically or by endoscopic approach, which is a minimally invasive method. Reducing the gastrojejunal anastomosis or gastric pouch size by endoscopy did not yield successful results in the long term. At 2-month results of endoscopic sclerotherapy, only 7-9% showed EWL and the rate of regain weight was 25%11. Endoscopic plication of the anastomosis resulted in 25% EWL in 5 months, although promising in the short term, most patients started to regain weight at the end of the 1st year12. Surgical revision of gastrojejunostomy and reduction of gastric pouch size did not yield desired weight loss results in the long term. Up to 69% of EWL has been reported in the literature after increasing the malabsorptive component of RYGB by converting it to a distal RYGB or duodenal switch13,14. In this study, we aimed to present the results of four patients who underwent a revision from RYGB to SG due to insufficient weight loss. In the literature, there are patients who underwent revision from RYGB to SG due to inadequate weight loss or weight gain again (Table 3).
Table 3 Literature of RYGB revision to Sleeve Gastrectomy for inadequate weight loss treatment
| Author | Patient | Age (y) | Pre RYGB BMI (kg/m²) | Time to revision (m) | Post RYGB min BMI | Pre Revision BMI | Post revision follow-up (m) | Current BMI | Complication |
|---|---|---|---|---|---|---|---|---|---|
| Parikh et al. | 14 | 43 | 46.8 | 41 | 30.5 | 35.5 | 12.2 | 32.9 | No |
| Dapri et al. | 4 | 42 ± 14.7 | 43.2 ± 8 | 36.7 ± 15.6 | 33.2 ± 7 | 37.3 ± 6.6 | 11 | 30.3 ± 5.1 | 1 patient (Gastrogastric fistula) |
| Carter et al. | 1 | 61 | Na | Na | Na | 47.9 | 12 | 34 | No |
| Lakdawala et al. | 5 | 38.8 ± 9.1 | 57.9 ± 8.1 | 74 ± 13 | 13.6 | 46.6 ± 11.5 | 12 | Na | No |
In our group, the mean EWL after conversion from RYGB to SG was 74.77 ± 8.94%, Lakdawala et al. in the study of five patients, the mean EWL at 1 year was 35.8 ± 8.8%, Dapri et al. reported 59.3 ± 31.5% EWL in 1 year in four patients15,16. Continuous weight loss after revision; we attribute it to the functioning of the pylorus, which increases the restriction, and resection of the entire ghrelin-producing fundus of the stomach.
There are studies in the literature emphasizing that pre-operative BMI can be a predictor of weight loss after bariatric procedures. In our patient group, the mean BMI before RYGB was 52.52 ± 6.42 kg/m². It was 57.9 ± 8.1 kg/m² in the Lakdawala et al study group and 43 ± 8 kg/m² in Dapri et al's series 15,16. Dixon et al.17 evaluated the first-year results of 440 patients who underwent gastric banding and demonstrated a significant relationship between increased BMI and low EWL%17.
We think that surgical techniques are associated with morbidity in the revision of RYGB to SG. Anastomosis of the gastric pouch to the remnant stomach has a risk of fistula. The gastric pouch, gastrojejunostomy, and remnant stomach need to be exposed for a tension-free anastomosis. For successful SG, the fundus and corpus should be adequately resected. We prefer to perform gastrogastrostomy with the linear stapler, but anastomosis using circular stapler has also been reported in the literature in addition to the manual method16. There are also studies indicating that gastrogastrostomy with circular stapler has a high risk in terms of stenosis18. Surgeons have no consensus on the gastrogastric anastomosis technique. Dapri and Vilallonga did not have stenosis in any of the patients who were hand stitched, but Simper et al. reported a 50% stenosis as a result of a similar suture technique16,19,20.
The distal and proximal parts of the gastrogastric anastomosis are susceptible to ischemia, so there is a risk of fistula and stenosis. Fistula developed in two of our patients, probably due to ischemia in the gastric pouch. To reduce this risk, it is necessary to avoid unnecessary dissection that will impair blood supply during both primary and revision operations. A low-flow fistula developed in one of our patients, and he was discharged with a conservative approach on the 21st day. In another patient, primary repair was performed on fistulized areas due to fistula-related sepsis. Feeding jejunostomy was placed, oral intake was closed. Later, a stenosis developed in the anastomosis due to the increased granulation tissue. Surgery was decided due to re-controlled fistula development. Subtotal gastrectomy was performed 6 months after revision surgery due to failure of stent placement. Endoscopic stent placement is one of the methods preferred in the literature in the treatment of high-flow fistulas21. However, lavage and drainage are required in unstable and septic patients.
The high risk of fistula after revision may bring to mind the use of additional enteral feeding routes. While our patients did not routinely use this method during SG, feeding jejunostomy was performed in one of our patients during the complication surgery. It was used in the 6-month period until subtotal gastrectomy in our patient, who could not take oral intake for a long time. Carter et al. applied nasojejunal enteral nutrition in four of their 12 patients for anastomosis safety during revision surgery, and in the other four patients due to insufficient oral intake due to post-operative persistent vomiting22.
Simper et al. reported that five of eight patients developed complications after RYGB revision to SG. They observed complications such as gastric fistula, superior mesenteric vein thrombosis, ileus, gastrogastrotomy stricture, and splenic bleeding19. In a series of ten patients, Vilallonga et al. reported anastomotic leakage in three patients and gastric ulcer in one patient20. Revision surgery has higher morbidity (21.8-23%) and mortality (1.3%) rates compared to primary surgery23. One of the most serious complications is fistula development in the gastrogastric anastomosis (4.2-11%)4. The alternative of RYGB to SG revision is to convert to normal anatomy. However, since it is a rarely preferred operation, its morbidity rates are not known.
The average lenght of hospital stay of our patients is longer compared to other studies13. We attribute this to the long hospitalization due to gastric fistula in our two patients.
One of the limitations of our study is that it is retrospective. It has also been studied in a small group of patients, but RYGB to SG revision is a rare procedure and the number of cases reported in the literature is low. To better understand the procedure, it will be possible by sharing the articles, in which large-scale evaluations are made, although the number is small.
Laparoscopic conversion of RYGB to SG is feasible operation. Gastric fistula is a serious risk. This procedure is successful in solving certain complications of RYGB, but has a high rate of major complications, as well as a need for re-hospitalization and additional nutrition. Larger series are needed to better understand the success of this procedure.











 nova página do texto(beta)
nova página do texto(beta)