Casos Clínicos
Embolización de cuerpo extraño por la raíz aórtica por lesión por
arma de fuego: caso clínico de una paciente asintomática de diez
años
Foreign body embolization by the aortic root due to a fire gun
injury: A case report of a 10-year-old asymptomatic patient
Sefer Kaya1
Dilan Oruç1
Ekin Anil-Ünal2
İbrahim Demir3
*
Metin Onur-Beyaz1
1Department of Cardiovascular Surgery, Tayfur
Ata Sökmen Faculty of Medicine, Hatay Mustafa Kemal University,
Hatay
2Department of Anesthesia and Reanimation,
Tayfur Ata Sökmen Faculty of Medicine, Hatay Mustafa Kemal University,
Hatay
3Department of Cardiovascular Surgery, Faculty
of Medicine, Istanbul University, Istanbul. Turkey
Resumen
Las embolias de cuerpo extraño que tienen origen en el sistema arterial se han
presentado en su mayoría sintomáticas y por eso requieren cirugía de emergencia.
Sin embargo, los casos asintomáticos se siguen de manera conservadora, pueden
causar patologías vasculares relacionadas con los órganos diana a medida que
pasa el tiempo. La migración de cuerpos extraños desde la aorta ascendente hasta
la arteria del órgano blanco es muy rara en la literatura después de una lesión
por arma de fuego. Casos sintomáticos, la cirugía de emergencia debe
planificarse de inmediato. En casos asintomáticos, primero se deben considerar
los riesgos y beneficios antes de cualquier abordaje quirúrgico.
Palabras clave Lesión por arma de fuego; Embolización por cuerpo extraño; Raíz aórtica
Abstract
Foreign body embolies that origin arterial system have mostly seen symptomatic
and that’s why they require emergency surgery. However, asymptomatic cases are
followed conservatively, they can cause vascular-related end-organ pathologies
as time passes. Foreign body migration from the ascending aorta to the end-organ
artery is a very rare in literature after a fire gun injury. In symptomatic
cases, emergency surgery should be planned immediately. In asymptomatic cases,
the risks and benefits should first be considered before any surgical
approach.
Keywords Fire gun injury; Foreign body embolization; Aortic root
Introduction
Foreign bodies in the heart or major arteries can be seen due to fire gun injuries.
Increased use of illegal drugs in recent years can cause migrating needles1,2.
Furthermore, the catheters used for intravascular treatment can sometimes break off
and they can go to distal arteries or can migrate to the heart if they in veins3,4.
The sources of intravascular foreign bodies are different in every age group. The
most common cause in children is iatrogenic, while in adults, it is due to illegal
drug use or war injuries5.
Foreign body embolies that origin arterial system have mostly seen symptomatic and
that’s why they require emergency surgery. However, asymptomatic cases are followed
conservatively, they can cause vascular related end-organ pathologies as time
passes6.
In this paper, we present the case of a 10-year-old male patient who got injured by a
fire gun and underwent emergency surgery. The bullet was not founded in the
intrathoracic region, the bullet had migrated into the segmental artery of the
liver.
Case report
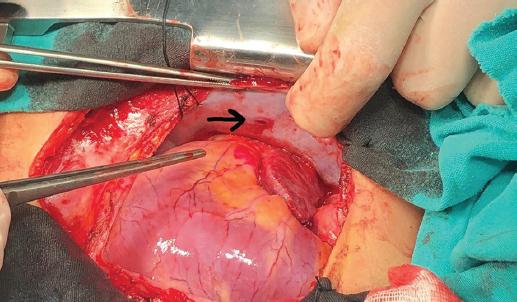
A 10-year-old male patient applied to the emergency service. The first physical
examination shown the entrance of the bullet was just below the right nipple,
however, there were no evidence of an exit of the bullet (Fig. 1). His heart rate was 138 beats/min, blood pressure was
65/38 mmHg. Echocardiography was performed in the emergency room.
The right ventricular dilatation, dilatation of the inferior vena cava, and signs of
cardiac tamponade supported by more than 2.8 cm of fluid at the thinnest point
around the heart were observed. He underwent emergency operation immediately. After
the pericardium was opened, his vital functions immediately returned to normal.
However, no major bleeding was found. No signs or traces of the bullet were found.
During intraoperative exploration, a bullet entrance was found on the right pleural
area (Fig. 2).
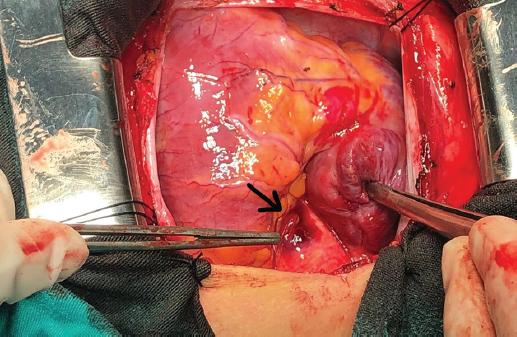
When explored in detail, adventitial hematoma was detected on the right anteromedial
surface of the aortic root (Fig. 3). No
additional bleeding was detected despite physical manipulations and washing with
warm water. After the procedure, chest and abdomen computed tomography were applied
in addition to the chest X-ray. A foreign body forming a metallic structure was
detected in the segmental branch of the hepatic artery (Fig. 4). With the recommendations of the pediatric surgery
department, no additional surgeries should be planned, and the patient was decided
to be followed. After the 5th day postoperatively, no pathologies were
seen in the patient’s liver functions tests, so the patient got discharged without
any problem.
Discussion
Foreign body embolization was first introduced in literature in 1834, after that,
only a few cases have been added to literature7. If the foreign body is not found at the site of surgery, foreign body
embolization should always be kept in mind8.
Gunshot wounds manifesting in the intravascular space affect the arterial system 4/1
more frequently. When a foreign body enters the arterial lumen, the probability of
causing ischemic damage is 80%8,9.
In symptomatic cases and if the diameter of the foreign body is more than 5 mm,
emergency surgery should be planned to prevent ischemic event2. The treatment of asymptomatic foreign body penetrations is
still not very clear. Foreign body excision or conservative treatment options should
be considered according to the risk of surgery and complications10.
Conclusion
Foreign body migration from the ascending aorta to the end-organ artery is a very
rare in literature after a fire gun injury. Symptomatic cases, emergency surgery
should be planned immediately. In asymptomatic cases, the risks and benefits should
first be considered before any surgical approach.
References
1. Michelassi F, Pietrabissa A, Ferrari M, Mosca F, Vargish T, Moosa
HH. Bullet emboli to the systemic and venous circulation. Surgery.
1990;107:239-45.
[ Links ]
2. Actis Dato GM, Arslanian A, Di Marzio P, Filosso PL, Ruffini E.
Posttraumatic and iatrogenic foreign bodies in the heart:report of fourteen
cases and review of the literature. J Thorac Cardiovasc Surg.
2003;126:408-14.
[ Links ]
3. Stolt V, Cook S, Räber L, Wani S, Garachamani A, Vogel R, et al.
Amplatzer septal occluder to treat iatrogenic cardiac perforations. Catheter
Cardiovasc İnterv. 2012;79:263-70.
[ Links ]
4. Witzke CF, Martin-Herrero F, Clarke SC, Pomerantzev E, Palacios
IF. The changing pattern of coronary perforation during percutaneous coronary
intervention in the new device era. J İnvasive Cardiol.
2004;16:257-301.
[ Links ]
5. Kumar R, Rana SS, Kumar S, Das D, Datta M. Management of
accidental and ıatrogenic foreign body ınjuries to heart-case Series. J Clin
Diagn Res. 2017;11:PE01-4.
[ Links ]
6. Khurana A, Jain V, Gupta SC, Malik K, Gupta S. A potentially
dangerous ındustrial projectile lodged in the leg of a steel factory worker.
Cureus. 2021;13:e17870.
[ Links ]
7. Pan GZ, Bastidas JG, Hasaniya NW, Floridia R Jr. Bullet
embolization from an aorto-caval fistula to the heart. Interact Cardiovasc
Thorac Surg. 2013;16:710-11.
[ Links ]
8. Greaves N. Gunshot bullet embolus with pellet migration from the
left brachiocephalic vein to the right ventricle:a case report. Scand J Trauma
Resusc Emerg Med. 2010;18:367.
[ Links ]
9. Colquhoun IW, Jamieson MP, Pollock JC. Venous bullet embolism:a
complication of airgun pellet injuries. Scott Med J.
1991;36:16-7.
[ Links ]
10. Schroeder MF, Pryor HI 2nd, Chun AK, Rahbar R, Arora
S, Vaziri K. Retrograde migration and endovascular retrieval of a venous bullet
embolus. J Vasc Surg. 2011;53:1113-5.
[ Links ]











 nueva página del texto (beta)
nueva página del texto (beta)