Introduction
Well-differentiated thyroid carcinoma (WTC) is the most frequent endocrine malignant neoplasia. Its incidence has been rising over the past two decades, at least in part due to the widespread use of neck ultrasound1. According to Globocan, thyroid cancer in Mexico is the 4th most common malignant tumor with 12,000 new cases diagnosed in 20182.
Total thyroidectomy is the treatment of choice in most cases of WTC (3). When this procedure is carried out by a high-volume surgeon, the morbidity and mortality are almost negligible3. However, thyroidectomy is not only performed by expert surgeons and in this setting the complication rate of the procedure increases considerably3. Transient post-operative hypocalcemia is perhaps the most frequent complication, occurring in 15-30% of cases, although in some series the reported incidence is over 60%4. Permanent hypocalcemia is considerably less frequent and its incidence ranges between 0.2% and 10%4,5. The risk factors that have been associated with the development of post-operative hypocalcemia include female gender, extrathyroidal tumor invasion, parathyroid injury, central compartment lymph node dissection, and obesity4. We here describe and analyze the occurrence of postoperative hypocalcemia in our center, seeking to find clinical and biochemical features that could serve as prognostic markers.
Material and methods
The electronic charts of patients undergoing a total thyroidectomy between January 2016 and December 2020 at the American British Cowdray Medical Center in Mexico City were retrospectively reviewed. The study protocol was approved by our Local Scientific and Ethics Committees. Patients younger than 16 years and patients with preoperative hypocalcemia or hypoparathyroidism as well as patients with scheduled concomitant parathyroid surgery were excluded from the study. The corresponding pathology reports were also assessed looking for the presence of parathyroid tissue. Hypocalcemia was defined as a total serum calcium < 8 mg/dL or an ionized calcium < 4.0 mg/dL. In those patients with discrepant results, the normal measurement was favored.
Variables were categorized into the following three groups:
a) Baseline variables: Gender, age, pre-operative hyper/hypothyroidism, history of neck surgery, and comorbidities.
b) Surgical variables: Indication for surgery, operating room (OR) time, a > 200 mL intraoperative bleeding, lymph node dissection, drain placement, surgeon’s yearly volume, and parathyroid identification, parathyroid gland incidental injury, and reimplantation when detected.
c) Tumor variables: Size, histological type, stage, lymph node invasion, capsular, and vascular lymphatic or neural invasion as well as locoregional and/or distant metastasis.
Statistical analysis
Nominal and ordinal variables were described as absolute numbers and percentages; numeric variables depending on their type of distribution were expressed as means with standard deviations medians with interquartile ranges. Continuous variables were analyzed with the T student test for independent variables when a normal distribution was present and with the U of Mann–Whitney when it was not. Nominal and ordinal variables were analyzed with a χ2 test. All the losses from baseline variables were smaller than 15% so they were all substituted. The ordinal and nominal variables were substituted by mode and the continuous variables by means or medians, depending on their distribution. Finally, the association values like odds ratio and confidence intervals and the statistical significance were obtained with χ2, as well as with linear and logistic regressions. p < 0.05 was considered statistically significant. All the information was consolidated on an unidentified spread sheet on Microsoft Excel version 2010 and the statistical analysis was done using IBM SPSS Statistics version 25.
Results
A total of 337 patients underwent a total thyroidectomy at our center over the study period. Median age was 47 years (interquartile range [IQR] = 37-69), 262 (77.7%) were women and 75 (22.2%) were men (Table 1). Preoperatively, the majority of patients had normal thyroid function tests; 43 (12.8%) had a prior diagnosis of hypothyroidism and were under levothyroxine replacement and 29 (8.6%) had evidence of hyperthyroidism (Table 1). In the majority of patients (253, 75.1%), the underlying diagnosis was WTC (Table 1). Other indications for surgery included goiter (38, 11.3%) and thyroiditis (15, 4.5%) (Table 1). Complete outcome information was available in 290 patients. Post-operative hypocalcemia was diagnosed in 38 (13.1%). Symptoms and signs of hypocalcemia ranged from perioral numbness to frankly positive Trusseau and Chvostek signs.
Table 1 Baseline characteristics of the cohort
| n | % | |
|---|---|---|
| Median age (IQR) | 47 | (37-69) |
| Female gender | 262 | 77.7 |
| Hypothyroidism | 43 | 12.8 |
| Hyperthyroidism | 29 | 8.6 |
| Underlying diagnosis | ||
| – Thyroid cancer | 253 | 75.1 |
| – Goiter | 38 | 11.3 |
| – Thyroiditis | 15 | 4.5 |
| – Other | 31 | 9.2 |
IQR: interquartile range.
Table 2 compares the characteristics of the patients who developed post-operative hypocalcemia with those who remained normocalcemic. A pre-operative diagnosis of hypothyroidism was more commonly present among patients who did not develop post-operative hypocalcemia (13.4% vs. 0%, p = 0.018). Post-operative hypocalcemia developed in 32 of the 219 patients with a diagnosis of thyroid cancer (14.6%), in two of the 31 patients with multinodular goiter (6.4%), and in two of the 15 patients with thyroiditis (13.3%); the difference in the rates of hypocalcemia among patients with these three different diagnostic categories did not reach statistical significance. Lymph node invasion and dissection as well as surgical time > 2.5 h were significantly more common among patients who became hypocalcemic after surgery. Parathyroid gland injury was significantly more frequent in patients who developed hypocalcemia than in those who remained normocalcemic, as was the need to leave a drain after surgery.
Table 2 Univariate analysis of clinical and surgical features of patients who developed post-operative hypocalcemia and those who did not
| n (%) | Hypocalcemia 37 (12.7%) | Normocalcemia 253 (87.3%) | p |
|---|---|---|---|
| Age > 60 | 8 (21.6) | 60 (23.7) | 0.770 |
| Female gender | 24 (64.8) | 199 (78.6) | 0.063 |
| Pre-operative hypothyroidism | 0 | 34 (13.4) | 0.018 |
| Pre-operative hyperthyroidism | 4 (10.8) | 21 (8.3) | 0.611 |
| Underlying diagnosis | |||
| – Thyroid carcinoma | 32 (86.4) | 187 (74) | 0.33 |
| – Goiter | 2 (5.4) | 29 (11.4) | 0.33 |
| Lymph node invasion | 15 (40.5) | 54 (21.3) | 0.01 |
| Lymph node dissection | 16 (43.2) | 60 (23.7) | 0.01 |
| Surgical time > 2.5 h | 18 (48.6) | 79 (31.2) | 0.03 |
| Estimated blood loss > 200 mL | 2 (5.4) | 12 (4.7) | 0.861 |
| Parathyroid gland identification | 35 (94.6) | 238 (94) | 0.891 |
| Parathyroid gland reimplantation | 1 (2.7) | 18 (7.1) | 0.311 |
| Parathyroid gland injury | 16 (43.2) | 58 (23) | 0.008 |
| Drain placement | 17 (46) | 66 (26) | 0.008 |
In bold: p statistically significant
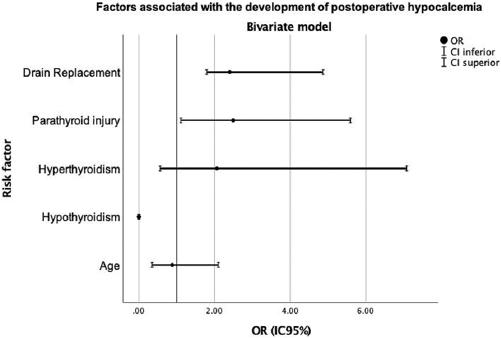
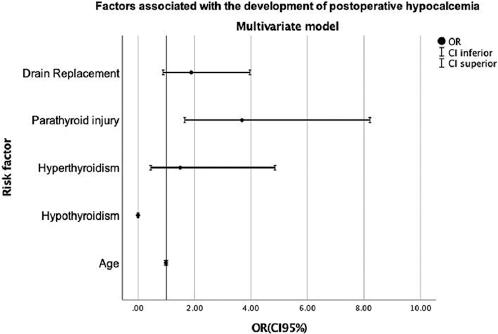
On bivariate analysis, pre-operative hypothyroidism, intraoperative parathyroid gland injury, and the need to leave a drain were all significantly associated with the development of post-operative hypocalcemia (Fig. 1). However, on multivariate analysis, only documented parathyroid injury remained significantly associated with the development of post-operative hypocalcemia (OR = 3.68, 95% CI = 1.65-8.21, p = 0.001) (Fig. 2). Table 3 shows a side-by-side comparison between the bivariate and the multivariate analysis.
Table 3 Bivariate and multivariate analysis of factors associated with the development of postoperative hypocalcemia
| Bivariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Age | 0.88 | 0.35-2.10 | 0.779 | 0.99 | 0.97-1.02 | 0.692 |
| Hypothyroidism | 0 | 0 | 0.018 | 0 | 0 | 0.008 |
| Hyperthyroidism | 2.06 | 0.56-7.08 | 0.611 | 1.49 | 0.45-4.85 | 0.507 |
| Parathyroid injury | 2.49 | 1.11-5.59 | 0.008 | 3.68 | 1.65-8.21 | 0.001 |
| Drain placement | 2.4 | 1.79-4.87 | 0.008 | 1.88 | 0.89-3.96 | 0.097 |
CI: confidence interval
Discussion
Parathyroid gland injury with the consequent post-operative hypocalcemia due to primary hypoparathyroidism (PHPT) is without a doubt, one of the most frequent complications of thyroid surgery, particularly of total thyroidectomy3,4. In a recently published meta-analysis, comprising 115 observational studies, the median rates of transient and permanent hypocalcemia were 27% (IQR = 19-38) and 1% (IQR = 0-3), respectively6. Post-operative hypocalcemia even when transient could hamper an appropriate surgical recovery and may prolong hospitalization4. Several risk factors have been variably associated with the occurrence of this complication, including concomitant central neck dissection specially when performed by a low volume surgeon, an underlying diagnosis of thyroid cancer or Graves’ disease, a lengthy surgical procedure particularly when accompanied by a > 200 mL intraoperative bleeding, as well as the lack of identification and/or inadvertent injury of parathyroid glands6.
The incidence of post-operative hypocalcemia in our cohort was unexpectedly low (12.7%) despite the fact that over 75% of our patients had an underlying diagnosis of thyroid cancer and that more than 25% had also been subjected to the central neck dissection. Although post-operative hypocalcemia tended to be more frequent among our patients with a thyroid malignancy, this did not reach statistical significance, likely because of the relatively small number of patients with a non-malignant underlying diagnosis included in the study. In contrast to other series whereby over half of the patients who develop post-operative hypocalcemia do so asymptomatically7,8, all of the hypocalcemic patients in our cohort had at least paresthesias appearing 8-12 h after the surgical event. Female gender and old age have both been associated with an increased risk of post-operative hypocalcemia6. Almost 80% of the patients in our cohort were women, and post-operative hypocalcemia tended to be more frequent in women than in men; however, this did not reach statistical significance.
It is controversial to what extent does the identification (and preservation?) of parathyroid glands during surgery impacts the probability of developing post-operative hypocalcemia. Some authors claim that the lack of identification of parathyroid glands is associated with transient9,10 as well as with permanent11 hypocalcemia, irrespective of the underlying diagnosis, and the extent of thyroidectomy. Conversely, other studies have found that identifying the parathyroid glands during surgery is by itself associated with a greater likelihood of post-operative hypocalcemia12. In our study, neither the identification nor the reimplantation of parathyroid glands was significantly associated with the development of hypocalcemia. Yet, we did find that parathyroid gland injury, be it inadvertent (i.e., parathyroid glands found in the pathology specimen) or advertent, significantly predicted the development of postoperative hypocalcemia in both, bivariate and multivariate analyses. Intuitively, thyroidectomies performed by large volume surgeons should have a lower rate of complications, including the development of post-operative hypocalcemia6,13. Our study was not designed to address this issue, since the majority of our patients were operated by large volume surgeons.
Patients undergoing thyroidectomy for diffuse toxic goiter or Graves’ disease appear to have an elevated risk of post-operative hypocalcemia11. More recently, one of the few prospective studies evaluating post-operative hypocalcemia after thyroidectomy found that thyrotoxicosis diagnosed < 10 years before surgery was significantly associated with hypocalcemia8. Of the 29 hyperthyroid patients included in our cohort, only four developed post-operative hypocalcemia. Interestingly, however, none of the 43 patients with hypothyroidism became hypocalcemic after surgery and in the multivariate analysis, hypothyroidism was negatively associated with post-operative hypocalcemia.
Our study has several limitations such as its retrospective nature, the lack of a uniform surgical procedure due to the fact that it reflects the combined experience of several low volume and a few large volume surgeons, and perhaps more importantly, the lack of long-term follow-up. Despite these weaknesses, the present report takes place in a real-life setting and thus, our data are undoubtedly representative of what occurs in day-to-day life.











 nueva página del texto (beta)
nueva página del texto (beta)