Introduction
In December 2019, several cases of atypical pneumonia emerged in China. A novel coronavirus was identified and named Severe Acute Respiratory Syndrome Coronavirus-21,2. As a consequence of this pandemic healthcare workers (HCWs) were forced to use personal protective equipment (PPE). The prolonged use of PPE has been associated with skin lesions3, head and facial discomfort due to heat and humidity, pressure, pain, itching4,5, difficulty breathing, fatigue, exertion,6 and de novo headaches7-11. These may negatively impact HCWs’ performance and tolerance to long-term use of PPE12,13.
De novo PPE-associated headaches may have a multifactorial origin. The main proposed mechanism is external compression headache (ECH).7 ECH is a primary headache coded in the 3rd edition of the International Classification of Headache Disorders14,15. The diagnostic criteria are (A) at least two episodes that meet criteria B-D, (B) it is caused by and occurs within, 1 h of constant external compression of the forehead or scalp, (C) the intensity is maximum at the point where external compression occurs, (D) subsides within 1 h after the release of external compression, and (E) not attributable to any other diagnosis15.
As far as we know, this phenomenon has not yet been studied in our population. Hence, we set out to investigate the prevalence of PPE-associated headache in Mexican HCWs and the conditional probability of developing it based on specific factors.
Methods
We conducted a cross-sectional study at ABC Medical Center from July 8 to August 11, 2020, during phase III of our country’s coronavirus disease 2019 (COVID-19) pandemic. Our institution made mandatory for HCWs to wear at least a surgical mask in any hospital area. However, we observed a generalized use of the N95 face mask plus any eye protection device (EPD) among healthcare workers of non-COVID wards (HCWs-NCW).
Based on the hospital census, we invited all the physicians and nurses registered on both campuses to participate in the study. We enrolled front-line healthcare workers (FL-HCWs) and HCWs-NCW of any hospital area (emergency rooms, hospitalization, intensive care unit, and outpatient areas) who agreed to participate and gave written consent. The Institutional Research and Ethics Committee approved the study.
We applied a digital survey, which was developed by the two neurologists conducting the study on Google Forms and was shared through WhatsApp to HCWs registered in the hospital census. The questionnaire included five sections: (1) information about the study’s objective, a consent part approved by all participants before answering the survey, and instructions for completing it, (2) asked about demographic data, (3) inquired about PPE-usage patterns in the last month before inclusion, (4) asked if the participant had suffered a primary headache disorder (PHD) before the pandemic, the type of headache, the use of preventive or acute treatment, and each participant’s perception of the behavior of their PHD during the COVID-19 pandemic, and (5) asked about PPE-associated headache phenotypic characteristics. We defined PPE-associated headaches as those in close temporal relationship to the use of PPE, and we categorized them as de novo headaches (never experienced before) and PHD present before the pandemic that worsened in frequency or intensity due to PPE wearing.
Statistical analysis
Data analysis was performed using SPSS V.25.0 statistical package program for Windows. We calculated descriptive analyses, percentage distributions of the different categories of the analyzed variables and, in the case of quantitative variables average, standard deviation, variance, asymmetry index, and kurtosis. The Chi-square test was used for 2 × 2 contingency tables and for proportional contrast to stipulate the association or dependency relationship between qualitative variables. We used t-test for independent samples to compare means between groups.
We performed multivariate histograms with the qualitative and quantitative variables to examine the possible probabilistic intersections (A∩B∩C∩ ) and, based on that, describe the statistical dependence between the analyzed variables and their probability of occurrence. To establish whether there was a correlation between the variables, the Pearson Correlation Coefficient test was employed. The statistical significance was set at the level of p < 0.05.
Results
We surveyed 305 HCWs, 153 females (50.16%) and 152 males (49.83%), with an average
age of 37.86 ± 9.57 years (mean, SD), range of 47 years (interval 21-68 years), 273
(89.50%) physicians, and 32 (10.49%) nurses. Of respondents, 141 (45.90%) were
FL-HCWs and 165 (54.09%) HCWs-NCW. The N95 face-mask was the most used device by 286
(93.77%) participants, 143 (46.88%) used face shield, 125 (40.98%) safety glasses,
121 (39.67%) goggles/visor, and 76 (24.91%) surgical masks. For calculating these
frequencies, we used replacement sampling due to the possible use of multiple
protective devices. The average use of the different devices was 18.73 ± 9.07
days/month for the N95 face mask, 15.05 ± 9.22 days/month for EPD (googles/visor,
face shield) and 12.93 ± 9.28 days/month for the combined used of the N95 face mask
+ EPD. The average daily use of the N95 face mask was 8.50 ± 5.43 h/day, 5.96 ± 4.35
h/day for safety glasses/goggles/face shield and 5.27 ± 4.49 h/day for the combined
use of the N95 face mask + any EPD. Of the total studied population, 36.06% suffered
a PHD before the pandemic onset. Tension-type headache was the most frequent
disorder reported by  or 62.72%, followed by migraine
with aura in
or 62.72%, followed by migraine
with aura in  or 24.54% and migraine without
aura
or 24.54% and migraine without
aura  or 22.72%. At least
or 22.72%. At least
 or 69.09% of the participants with
PHD occasionally used abortive treatment; only
or 69.09% of the participants with
PHD occasionally used abortive treatment; only  or 5.45% took preventive treatment
and topiramate was the most used. At least
or 5.45% took preventive treatment
and topiramate was the most used. At least  (62.72%) considered that their PHD
worsened with the regular use of PPE (Table
1).
(62.72%) considered that their PHD
worsened with the regular use of PPE (Table
1).
Table 1 Demographic Characteristics of 305 Healthcare Workers Who used PPE During COVID-19 pandemic
| Characteristics | Healthcare Workers n = 305 (%) |
|---|---|
| Age (years) | 37.86 ± 9.57 |
| Gender | |
| Female | 153 (50.16) |
| Male | 152 (49.83) |
| Occupation | |
| Doctor | 273 (89.50) |
| Nurse | 32 (10.49) |
| N95 face mask | 286 (93.77) |
| Days per month worn (days) (mean ± SD) | 18.73 ± 9.07 |
| Hours per day worn (h) (mean ± SD) | 8.50 ± 5.43 |
| Eye protection devices (EPD) | |
| Face shield | 143 (46.88) |
| Safety glasses | 125 (40.98) |
| Goggles/visor | 121 (39.67) |
| Days per month worn EPD (days) (mean ± SD) | 15.05 ± 9.22 |
| Hours per day worn EPD (h) (mean ± SD) | 5.96 ± 4.35 |
| Combination N95 face mask and EPD | |
| Days per month worn (days) (mean ± SD) | 12.93 ± 9.28 |
| Hours per day worn (h) (mean ± SD) | 5.27 ± 4.49 |
| Pre-existing primary headache disorder (PHD) | 110 (36.06) |
| Tension type headache | 69 (62.72) |
| Migraine with aura | 27 (24.54) |
| Migraine without aura | 25 (22.72) |
| Preventive treatment for PHD | 6 (5.45) |
| Worsening of PHD with frequent PPE use | 69 (62.72) |
EPD: eye protection devices; PHD: pre-existing primary headache disorder; PPE: personal protective equipment; SD: standard deviation.
Of the 305 persons surveyed, 206 (67.54%) reported PPE-associated headaches, 119
(39.01%) had de novo headaches while 87 (28.52%) had a worsening of
a PHD. The majority,  or 76.21% reported headache of
tightening quality,
or 76.21% reported headache of
tightening quality,  or 20.38% reported pulsatile pain
and
or 20.38% reported pulsatile pain
and  or 16.99% stabbing pain. We
calculated these frequencies with replacement sampling (Table 2).
or 16.99% stabbing pain. We
calculated these frequencies with replacement sampling (Table 2).
Table 2 Characteristics of PPE-associated headaches in healthcare workers
| Characteristics | Healthcare Workers n = 206 (%) |
|---|---|
| PPE- associated headache | 206 (67.5) |
| De novo headache | 119 (39.01) |
| Aggravated pre-existing PHD | 87 (28.52) |
| Headache attacks per month | 5.75 ± 6.52 |
| Headache Type | |
| Oppressive | 157 (76.21) |
| Pulsatile | 42 (20.38) |
| Stabbing | 35 (16.99) |
| Headache intensity | |
| Mild | 96 (46.60) |
| Moderate | 106 (51.45) |
| Maximum intensity at contact sites of PPE | 110 (53.39) |
| Associated symptoms | |
| Neck pain | 88 (42.71) |
| Dizziness | 58 (28.15) |
| Nausea | 31 (15.04) |
| Need for acute analgesic requirement | 157 (76.21) |
| Paracetamol | 95 (46.11) |
| NSAIDs | 78 (37.86) |
| Number of days participants took analgesic medication (days) (mean ± SD) | 2.53 ± 3.76 |
NSAIDs: non-steroidal anti-inflammatory drugs; PHD: Pre-existing primary headache disorder; PPE: personal protective equipment.
The time interval between donning PPE to the onset of headache was > 60 min in
 or 64.07% of HCWs, while it was
< 60 min in
or 64.07% of HCWs, while it was
< 60 min in  or 35.92%. After removal of PPE,
headache resolved within 60 min in
or 35.92%. After removal of PPE,
headache resolved within 60 min in  or 70.87% of the cases (Table 3).
or 70.87% of the cases (Table 3).
Table 3 Time interval between wearing or removal of PPE and the onset or resolution of PPE- Associated headaches (n = 206).
| Variable | Value |
|---|---|
| Time interval between wearing PPE to onset of headache (min), n (%) | |
| < 15 | 6 (2.91) |
| 15-30 | 19 (9.2) |
| 31-45 | 23 (11.17) |
| 46-60 | 26 (12.62) |
| >60 | 132 (64.1) |
| Time interval from removal of PPE to resolution of headache (min), n (%) | |
| < 15 | 39 (18.93) |
| 15-30 | 46 (22.33) |
| 31-45 | 38 (18.44) |
| 46-60 | 23 (11.17) |
| >60 | 60 (29.13) |
PPE: personal protective equipment.
Headache intensity was considered mild by  or 46.60% HCWs, moderate by
or 46.60% HCWs, moderate by
 or 51.45%, and severe by
or 51.45%, and severe by
 or 4.85%. Associated symptoms
were neck pain in or
or 4.85%. Associated symptoms
were neck pain in or  42.71% HCWs, dizziness in
42.71% HCWs, dizziness in
 or 28.15%, and nausea in
or 28.15%, and nausea in
 , or 15.04%. Of the 206
respondents with PPE-associated headaches, 110 (53.39%) reported maximum pain at
contact sites of the devices with the craniofacial structures. Only
, or 15.04%. Of the 206
respondents with PPE-associated headaches, 110 (53.39%) reported maximum pain at
contact sites of the devices with the craniofacial structures. Only  or 16.99% of the cases met the
diagnostic criteria for ECH. HCWs with PPE-associated headaches reported an average
of 5.75 ± 6.52 attacks per month. During an attack
or 16.99% of the cases met the
diagnostic criteria for ECH. HCWs with PPE-associated headaches reported an average
of 5.75 ± 6.52 attacks per month. During an attack  or 76.21% required analgesic
treatment. The mean number of days participants took analgesic medication to relieve
that the pain was 2.53 ± 3.76 days/month. Paracetamol was the most used analgesic by
or 76.21% required analgesic
treatment. The mean number of days participants took analgesic medication to relieve
that the pain was 2.53 ± 3.76 days/month. Paracetamol was the most used analgesic by
 or 46.11%, followed by
non-steroidal anti-inflammatory drugs in
or 46.11%, followed by
non-steroidal anti-inflammatory drugs in  or 37.86% (Table 2).
or 37.86% (Table 2).
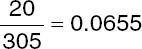
We made a multivariate histogram to analyze the conditional probability of the study
variables from the probabilistic intersections between PPE-associated headaches,
type of HCW, gender, and age. Thus  or 23. 60% had PPE-associated
headache, which were female HCWs-NCW between 30 and 40 years old;
or 23. 60% had PPE-associated
headache, which were female HCWs-NCW between 30 and 40 years old;  or 13.11% had PPE-associated
headache, which were male HCWs-NCW between 40 and 45 years old, while
or 13.11% had PPE-associated
headache, which were male HCWs-NCW between 40 and 45 years old, while
 or 15.73% had PPE-associated
headache, which were female FL-HCWs between 25 and 30 years old. Lastly,
or 15.73% had PPE-associated
headache, which were female FL-HCWs between 25 and 30 years old. Lastly,
 or 17.04% who experienced
PPE-associated headaches were male FL-HCWs between 35 to 42 years old. Therefore, we
can infer that caring for COVID-19 patients, gender and age are not independent
factors for PPE-associated headaches (Fig.
1).
or 17.04% who experienced
PPE-associated headaches were male FL-HCWs between 35 to 42 years old. Therefore, we
can infer that caring for COVID-19 patients, gender and age are not independent
factors for PPE-associated headaches (Fig.
1).
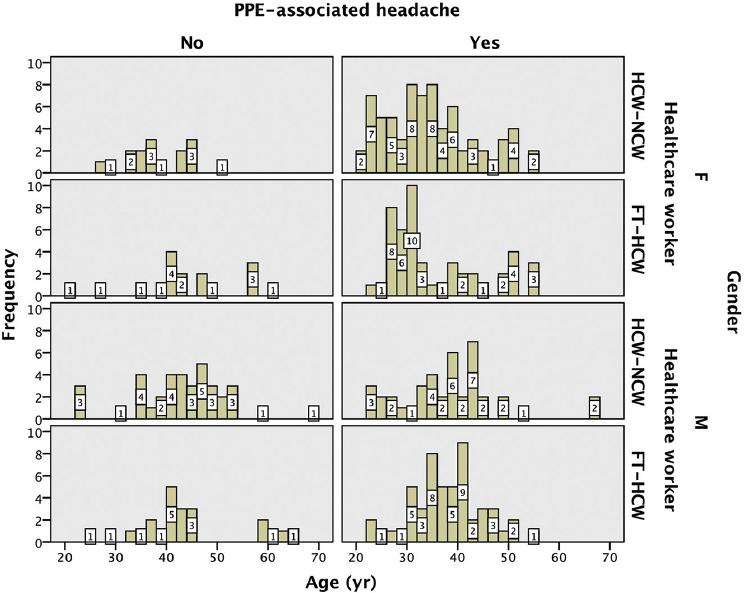
Figure 1 Tetra-variable histogram, PPE-associated headache, gender, age, and type of healthcare worker. We observed no relationship between age, gender, and type of healthcare worker with PPE-associated headaches.F: female; FT-HCW: front-line healthcare worker; HCW-NCW: healthcare worker of a non-COVID ward; M: male; PPE: personal protective equipment; yr: years.
We performed a multivariable histogram to analyze the statistical dependence between
the variables time interval between wearing PPE to the onset of headache, type of
HCW, gender, and age. The development of headache after wearing PPE for more than 60
min was the modal column in the analyzed variables. We can infer from the studied
sample that the probability of female HCW-NCW referring headache due to PPE use for
more than 60 min regardless of age  is 12.78%. The probability that a
male HCW-NCW refer headache from PPE use for more than 60 min, regardless of age,
which is
is 12.78%. The probability that a
male HCW-NCW refer headache from PPE use for more than 60 min, regardless of age,
which is  or 8.85%. A female FT-HCW’s
probability to refer headache due to PPE use for more than 60 min no matter the age
is
or 8.85%. A female FT-HCW’s
probability to refer headache due to PPE use for more than 60 min no matter the age
is 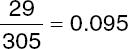 9.5%. Finally, the probability
that a male FT-HCW has a headache due to PPE use for more than 60 min irrespective
of age
9.5%. Finally, the probability
that a male FT-HCW has a headache due to PPE use for more than 60 min irrespective
of age  is or 9.83%. (Fig. 2) These results show that none of the
variables studied are independent factors for PPE-associated headaches, but headache
frequency increased as the longer HCWs wore the PPE (Table 3).
is or 9.83%. (Fig. 2) These results show that none of the
variables studied are independent factors for PPE-associated headaches, but headache
frequency increased as the longer HCWs wore the PPE (Table 3).
Figure 2 Tetra-variable histogram, time interval from donning PPE to the onset of headache, gender, age, and type of healthcare worker. The modal column was the onset of headache more than 60 min after wearing PPE. None of the variables studied are independent factors for PPE-associated headaches, but headache frequency increased as the longer HCWs wore the PPE.F: female; FT-HCW: front-line healthcare worker; HCW-NCW: healthcare worker of a non-COVID ward; M: male; min: minutes; NHG: non-headache group; PPE: personal protective equipment; yr: years.
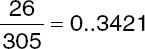
We analyzed the statistical dependence between the variables, headache intensity,
gender, age, and type of healthcare worker using multivariable histogram. The
highest frequency reported was a moderate headache in female FL-HCWs regardless of
age  , or 9.83% and in
, or 9.83% and in  8.52% male FL-HCWs. We observed
the opposite in the modal column for HCWs-NCW, who presented with a mild headache
8.52% male FL-HCWs. We observed
the opposite in the modal column for HCWs-NCW, who presented with a mild headache
 or 10.49% in women and
or 10.49% in women and
 or 6.55% in men; thus, we can
infer that providing COVID-19 care is determinant for headache intensity (Fig. 3).
or 6.55% in men; thus, we can
infer that providing COVID-19 care is determinant for headache intensity (Fig. 3).
Figure 3 Tetra-variable histogram, intensity of PPE-associated headache, gender, age, and type of healthcare worker. We observed a higher intensity of PPE-associated headaches among FT-HCW compared to HCW-NCW.F: female; FT-HCW: front-line healthcare worker; HCW-NCW: healthcare worker of a non-COVID ward; M: male; NHG: non-headache group; PPE: personal protective equipment; yr: years.
To determine the statistical dependence between the variables, PPE-associated
headache, history of PHD, and gender, we elaborated a trivariate histogram and a
contingency table to determine the probabilistic intersections between these
variables. Thus, the probability that a HCW without a history of PHD does not
manifest PPE-associated headache is  or 24.91%, of which or
or 24.91%, of which or
 34.21% were women and
34.21% were women and
 or 65.78% were men. The
probability that a participant without a history of PHD manifests PPE-associated
headache is
or 65.78% were men. The
probability that a participant without a history of PHD manifests PPE-associated
headache is  or 39.01%, of which
or 39.01%, of which
 or 49.57% were women and
or 49.57% were women and
 or 50.42% were men. The
probability that a participant with a history of PHD does not manifest
PPE-associated headache is
or 50.42% were men. The
probability that a participant with a history of PHD does not manifest
PPE-associated headache is  or 5.57%,
or 5.57%,  or 41.17% were women and
or 41.17% were women and
 or 58.82% were men. Finally, the
combined probability of having a history of PHD and manifesting PPE-associated
headache is
or 58.82% were men. Finally, the
combined probability of having a history of PHD and manifesting PPE-associated
headache is  or 30.49%, of which
or 30.49%, of which
 or 65.59% were women and
or 65.59% were women and
 or 34.40% were men. In the sample
studied,
or 34.40% were men. In the sample
studied,  or 39.01% denied a history of PHD
and experienced PPE-associated headache; this combination has the highest
probability of occurrence (p = 0.3901), followed by the combined probability of
having a history of PHD and experiencing PPE-associated headache in
or 39.01% denied a history of PHD
and experienced PPE-associated headache; this combination has the highest
probability of occurrence (p = 0.3901), followed by the combined probability of
having a history of PHD and experiencing PPE-associated headache in  or 30.49% (p = 0.3049). In the
latter intersection,
or 30.49% (p = 0.3049). In the
latter intersection, 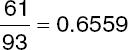 or 65.59% were women, while in
men, the highest combined probability is not having experienced PPE-associated
headaches nor a history of PHD in
or 65.59% were women, while in
men, the highest combined probability is not having experienced PPE-associated
headaches nor a history of PHD in  or 65.78% (Fig. 4).
or 65.78% (Fig. 4).
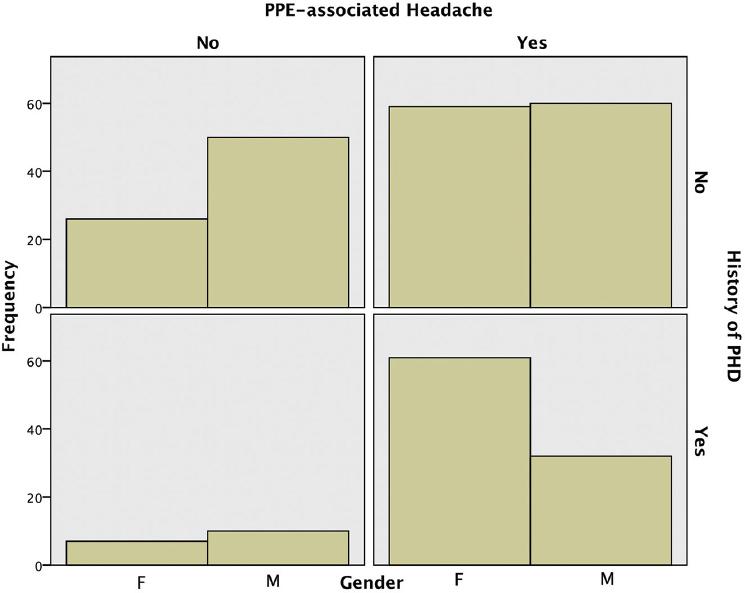
Figure 4 Tri-variable histogram, PPE-associated headache, history of primary headache disorder and gender. The highest frequency was for the intersection PPE-associated headache and absent history of PHD followed by having a history of PHD and experiencing PPE-associated headache.F: female; PHD: primary headache disorder; PPE: personal protective equipment; M: male; yr: years.
We made error bars to compare the mean and confidence intervals for the mean at 95% confidence limit of the days per month the N95 face mask and the EPD were used alone and combined, and we found a significant difference in both p ≤ 0.001, demonstrating a greater use of the N95 face mask (Fig. 5).When we compared means difference between the average hours per day, the N95 face mask and the EPD were used alone and combined, we also found a significant difference p ≤ 0.001, meaning the daily average use of the N95 face mask is higher.

Figure 5 Comparative error between days per month use of N95 face mask, eye protection devices, and the combination N95 facemask + eye protection devices. The N95 face mask was used significantly more days per month compared to the other devices. d.p.m: days per month.
We made an error bar to compare time intervals from donning the PPE to headache onset according to the number of days per month that the PPE was used. We observed that the more days per month HCWs worn PPE, the shorter was the time interval between donning PPE and headache onset (Fig. 6).

Figure 6 Error graph of the time interval between donning PPE to Headache Onset. The error graph shows that the more days per month HCWs worn PPE, the shorter was the time interval between donning PPE and headache onset.Min: minutes; NHG: non-headache group; PPE, personal protective equipment.
Finally, we calculated the correlation coefficient between the time interval from donning PPE to headache onset and headache intensity (r = 0.728), showing a high correlation between these variables. Inversely, we found a correlation between the time interval between doffing PPE to headache resolution and headache intensity (r = 0.662).
Discussion
We surveyed 305 Mexican HCWs to investigate the association between PPE use and de novo headaches. The prevalence of de novo PPE-associated headaches in our study was 39.01%, quite similar to the reported prevalence in another studies7-11.
Unlike studies published so far, we included HCWs-NCW in addition to FL-HCWs. The most used device was the N95 face mask, but as expected, FL-HCWs used more frequently the N95 face mask plus any EPD. Both types of HCWs worn the PPE for the same time. There was no difference in PPE-associated headaches prevalence between both groups, but headache intensity was higher in FL-HCWs (moderate vs. mild).
The most frequent phenotype of PPE-associated headache in our study was moderate intensity headache, oppressive quality accompanied by neck pain and dizziness, which is consistent to what has been published in other studies. We identified as predisposing factors for this type of headache wearing PPE for more than 60 min, wearing PPE more days per month, and having a pre-existing PHD.
A third of our participants reported having had a PHD before the pandemic. Surprisingly, few HCWs (only 5.45%) used preventive treatment for their PHD. Tension-type headache was the most reported disorder and at least 62.72% of HCWs considered, their PHD worsened during the current pandemic. Most of the participants (84.54%) with a history of a PHD reported having headaches while using PPE. However, cases of de novo PPE-associated headache were higher than cases of PHD worsening.
We observed an inversely proportional relationship between the number of days HCWs wore PPE and the time period, in which headache developed. Therefore, we can infer that frequent (several days per month) and prolonged (several hours per day) exposure to PPE could trigger headaches in a shorter period with each exposure. A possible explanation for this phenomenon could be that chronic exposure to a nociceptive stimulus (in this case, the compressive mechanical or traction effect exerted by the different devices and their elastic bands on the pericranial soft tissues) would induce sensitization of the craniofacial nociceptive system and the cervical trigeminal complex favoring a decrease in the threshold for presenting headache each time the exposure to the stimulus occurs. This mechanism is the pathophysiological basis of ECH, which results from the continuous activation of the superficial sensory nerves of the face, head, and neck (branches of the trigeminal or occipital nerve), caused by sustained pressure on the pericranial soft tissues14,15. Although only 17% of the participants in our study met the diagnostic criteria for ECH, we observed that in the majority of participants, headache occurred in close temporal relation to PPE wearing.
ECH is not the only probable mechanism involved in PPE-associated headaches. Several authors have found physiological alterations in users while wearing an N95 face mask associated with symptoms such as discomfort, fatigue, dyspnea, dizziness, and headache. In addition, increased serum CO2 levels (re-inhalation of exhaled air)16, decreased oxygen saturation (SpO2)17-19, increased heart rate, and blood pressure compared to baseline have been observed after wearing PPE for 4 h19,20. An increase in heart rate may be due to several conditions: a high respiratory resistance caused by an N95 face mask moist on the inside (as a consequence of the local rise in temperature and sweating), the level of user’s physical activity, baseline physical condition, an increase in CO2 retention, and anxiety associated with face mask use19,21.
The adverse effects of prolonged use of PPE lies could limit adherence when using protective devices and put the staff at risk of infection. We believe that further research and the development of new technologies and devices that guarantee proper protection without the related side effects should be carried out.
The strengths of our investigation are that we included FL-HCWs and HCWs-NCW; thus, we obtained a representative sample of the staff in our institution at risk of developing headaches due to PPE use; also, we included a gender-balanced group. The weaknesses of our study are that we conducted a cross-sectional study, we did not objectively measure the pressure exerted by the devices and their elastic bands on the craniofacial structures. Other physiological (hypoxemia, hypercapnia, dehydration, increased local temperature), and psychological (stress, anxiety) factors that may trigger PPE-associated headaches were not considered or analyzed in our study.
Conclusions
Like other symptoms brought on by PPE use, headaches have a multifactorial origin and, although external compression is a relevant factor, it is not the only one. Therefore, future research should consider the different pathophysiological mechanisms that seem to be involved in developing symptoms in individuals wearing PPE. Studies published so far, including ours, have analyzed the individual factors proposed to be causal. However, as far as we know, no study has covered all the proposed triggering factors for de novo PPE-associated headaches in their analyses. Based on current published data of predisposing conditions that lead HCWs to develop PPE-associated headaches, we believe that future research should focus on the development of novel protective devices less harmful than current ones.











 nueva página del texto (beta)
nueva página del texto (beta)


