Introduction
Arterioenteric fistulas (AEFs) are a rare condition. They are defined as the communication between a major artery and a loop of the digestive tract, the most frequent communication site being at the level of the duodenum1,2. They are classified into two types according to their etiology: primary and secondary. The primary fistulas are caused by aneurysms, trauma, radiation therapy, atherosclerotic disease, and inflammatory bowel disease, while the secondary fistulas are usually caused by previous aortic surgery with the use of synthetic prosthetic material3.
In this clinical case, we present a male patient who, after suffering a gunshot wound to the abdomen, underwent an exploratory laparotomy with damage control surgery. After discharge, he presented a picture of hematemesis and melena. Imaging and endoscopy studies were performed showing a pseudoaneursyma of the right renal artery and gastrointestinal bleeding due to the primary AEF, which is successfully treated by angioembolization.
Clinical case
A 27-year-old male was referred to our emergency department after suffering a gunshot wound to the epigastrium, a downward and right pathway was observed with an exit orifice in the right paravertebral lumbar region at the L3 level. Hemodynamically stable, tachycardic patient with pain on abdominal palpation and paralysis of both lower extremities was evaluated.
He went to the operating room where an exploratory laparotomy was performed, in which it was evidenced that the projectile lacerated the free edge of liver segment IV b, perforated the fundus of the gallbladder; the anterior face of the second portion of the duodenum was found to be blunt with a 0.5 mm defect, as well as complete perforation of the hepatic flexure of the colon; the route went to the pararenal fascia, where no injury was found in the right renal parenchyma or its vascular structures, ending the journey in the lumbar spine.
Given these findings, a right hemicolectomy was performed with terminal ileostomy, cholecystectomy with intraoperative cholangiography, in which the integrity of the biliary tree without leaks or lesions in the distal common bile duct was observed; the edges of the thermal lesion in the duodenum were debrided, a two-plane defect was repaired, and a closed drain was placed in the surgical bed.
During his post-operative period, the patient had a good clinical evolution; however, on post-operative day 5, bile fluid leakage was observed through the drain, a volume of 100 cc in 24 h, suspecting dehiscence of the duodenal repair, he went to the operating room for abdominal examination.
In this second intervention, 200 cc of bile fluid were found when entering the cavity, it was dissected to expose the duodenum in its entirety, observing the complete repair without evidence of leakage at the site or in any other duodenal portion. It was decided to proceed to endoscopic retrograde cholangiopancreatography to reassess the integrity of the bile duct. When performing the cholangiography, leakage of contrast material was observed at the level of the distal common bile duct at the level of the insertion at the level of the ampulla. It was decided to perform a sphincterotomy and biliary stent placement as treatment. The patient had an adequate clinical evolution, for which he was discharged.
Fourteen days after his medical discharge, the patient came after referring three episodes of hematemesis and melena through the ileostomy, he was found hemodynamically stable, with initial hemoglobin of 9 g/dL; a contrasted computed tomography (CT) was performed, where the presence of a saccular pseudoaneurysm in the right renal artery was observed in the arterial phase, which is in the proximity of the duodenum, in contact with the biliary diversion probe. Contact with the second portion of the duodenum shows an image suggestive of an AEF which conditioned the patient’s hematemesis episodes (Fig. 1).
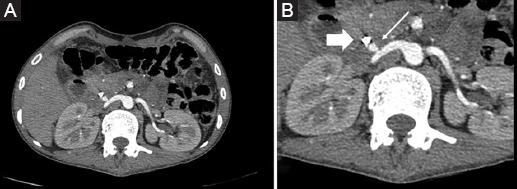
Figure 1 Contrast abdominal CT scan in arterial phase. A: The right renal artery with saccular aneurysm, which is in contact with the biliary diversion tube. B: Zoom in on the area, thin arrow: pseudoaneurysm of the renal artery. Thick arrow: biliary diversion probe.
With these findings, it was decided to carry out the management of the AEF by endovascular media, obtaining an access through the right common femoral artery, selective catheterization of the right renal artery was performed for angiography, observing pseudoaneurysm in its proximal third; it was catheterized at the neck of the pseudoaneurysm; and embolization was performed with a Terumo® controlled release 6 mm × 10 mm coil. Subsequently, a control angiography was performed at 3 min at the level of the right renal artery, where adequate occlusion of the pseudoaneurysm was evidenced (Fig. 2).
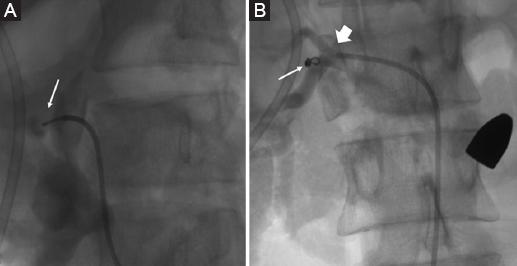
Figure 2 A: Arteriography with selective catheterization of the pseudoaneurysm of the right renal artery. Arrow: Pseudoaneurysm of the renal artery. B: Arteriography after coil placement in pseudoaneurysm, showing adequate occlusion of the vascular lesion. The image shows a firearm projectile at the left paravertebral level. Thin arrow: coil in topography of the pseudoaneurysm in the proper position. Thick arrow: right renal artery.
The patient is monitored clinically, without presenting a new episode of hematemesis, with a hemoglobin of 11.5 g/dL after transfusing 2 blood packets. Due to the good clinical resolution, the patient is discharged, and his follow-up is continued in the outpatient clinic, where 3 weeks after this last hospitalization, the patient remained asymptomatic, so he was discharged from the clinic.
Discussion
Aneurysmal lesions are abnormal dilations of the lumen of the vessels secondary to disease or damage to the vessel wall4,5. These lesions are classified into two types according to the composition of their wall: true aneurysms and pseudoaneurysms. True aneurysms are dilations of the arterial lumen with preservation of the three layers of the vessel (intima, media, and adventitia)6. However, pseudoaneurysms occur as a result of injury to one or more layers of the arterial wall. Compression of the periarterial tissue slows bleeding and forms a hematoma around the arteriotomy. Next, a fibrous reaction occurs that encapsulates the hemorrhage, forming a structure that resembles an aneurysmal sac. There is a theory that when this pseudoaneurysm bleeds, a hematoma is formed that is accompanied by a fibrous reaction, which if it persists is capable of eroding the intestinal wall, which until that moment served as containment, forming a fistulous path from the pseudoaneurysm toward the intestinal lumen7.
AEFs are a rare condition and are classified into the primary and secondary according to their etiology1,4,7. The primary fistulas are caused by aneurysms, trauma, radiotherapy, and atherosclerotic disease, their incidence ranges between 0.04% and 0.07% at the time of performing an autopsy. The secondary fistulas are usually caused by previous aortic surgery with the placement of synthetic prosthetic grafts, with a post-operative incidence ranging from 0.5% to 2.3%8.
The common symptoms of AEFs are hematemesis, melena, and abdominal pain. Bleeding is initially scanty and often intermittent (“sentinel hemorrhage”) but eventually leads to severe bleeding and hypovolemic shock5. Some patients before bleeding experience fever, fatigue, malaise, or weight loss, which often go unnoticed. The natural history of arterioenteric fistulas is the progression of hemorrhage and/or sepsis, it can even lead to death in cases with massive hemorrhages, unless a rapid, correct, and exact diagnosis associated with an adequate surgical treatment avoids the fatal outcome9. In the case of our patient, he was admitted to the emergency department after referring generalized weakness, hematemesis, and melena through the ileostomy; on admission, he was hemodynamically stable, so an approach for upper gastrointestinal bleeding was initiated and studies of image.
CT with intravenous contrast is considered the test of choice in hemodynamically stable patients, with a sensitivity of 50-94% and specificity of 85-100% for the diagnosis of arterioenteric fistulas10-12. Renal artery aneurysms are rare, and most of them are asymptomatic when detected by imaging. The CT scan of our patient was able to identify a saccular aneurysmal dilation of the right renal artery with a neck of 3 mm and a dome of 4 × 6 mm, which was found adjacent to the bile duct diversion and the second portion of the duodenum, for what existed the possibility of the existence of a fistulous path.
Endoscopy plays an important role in determining the main causes of gastrointestinal bleeding to rule out, such as esophageal variceal bleeding, peptic ulcers, among others. In some patients, it is not possible to identify the exact site of bleeding; however, in many cases, a clot associated with the site of the injury or even the presence of the fistula can be demonstrated with the presence of prosthetic material in cases, where it has already been placed a graft9. In our case, during the endoscopy for the approach to upper gastrointestinal bleeding, the presence of prosthetic material in contact with the duodenal lumen or any active bleeding site was not evidenced.
AEFs can have a fatal course if left untreated. Open surgery where enteric fistula repair is performed as well as artery repair by means of an in situ prosthetic graft or extra-anatomical reconstruction is widely accepted as the management today. However, despite successful surgery, there are mortality rates that have been reported from 21 to 90%, as well as a high rate of morbidity associated with these procedures. Due to this, the use of endovascular therapy has been presented as a promising technique for its management both definitively and in its use as bridging therapy, creating better conditions for later definitive surgery13-15. In the case presented, due to the previous interventions and the general conditions of the patient, it was decided to perform an angiography in renal arteries with selective catheterization of the right renal artery as therapeutic management; the contrast was introduced observing a pseudoaneurysm in the proximal third of the artery. A first attempt at coil embolization was made, observing the coil inside the pseudoaneurysm; however, on immediate angiographic control, migration of the coil was identified toward the lower third of the kidney. A second attempt was made with placement of coils in the pseudoaneurysm, with a post-embolization control angiography observing the coil within the pseudoaneurysm and without contrast passage within the pseudoaneurysm.
Caution must be exercised when making the initial evaluation of the patient, in whom gastrointestinal bleeding is suspected due to an arterioenteric fistula, due to the bleeding so important that it can be triggered from one moment to the next, with a fatal outcome. Therefore, a patient with evidence of AEF with data of hemodynamic instability, in cases where the necessary equipment is not available to perform endovascular therapy quickly, an emergency exploratory laparotomy is indicated for vascular control and vascular repair as enteric in a definitive way.
Conclusion
The purpose of this case report is to present an infrequent pathology that must be taken into account to rule out in patients who present with gastrointestinal bleeding. It is very important to quickly diagnose and intervene in these patients due to their high mortality rate. Endovascular management as a therapeutic alternative to open surgery in the initial approach of these patients has demonstrated its short-term efficacy, from stabilizing the patient to definitive therapy, as in this patient.











 nueva página del texto (beta)
nueva página del texto (beta)


