Introduction
Minimally invasive cardiac surgery is a reality in almost all surgical services, and even in many represents the standard approach for isolated aortic valve replacement (AVR) for the replacement and repair/replacement of the mitral valve. This is due to the fact that, in recent years, the minimally invasive approach has managed to produce results at least no worse than conventional surgery, and better in some respects, such as shorter hospital stays, but above all, it has been possible to establish that it is a safe technique, with a low-associated mortality rate1,2.
However, there are still centers reluctant to use it, or in which interventions of this type are carried out depending on the surgeon assigned. For this reason, the main aim of this study is to present the results of our minimally invasive program for isolated AVR in comparison with those presented by patients with the same pathology operated on using conventional surgery, focusing on post-operative (PO) mortality and also their PO course, to show that it is a safe surgical procedure in our environment. Furthermore, with the greater ageing of the population and the boom in percutaneous techniques, we intend to call for the minimally invasive approach as one of the treatment options to be borne in mind in the decision making of the Heart Team3.
Methods
Design
Retrospective observational study of patients undergoing isolated AVR using minimum access surgery or conventional surgery, between January 2016 and December 2019, at the cardiovascular service of our hospital, with a total number of 114 patients, 57 in each of the two groups. All the subjects undergoing AVR were over 65 years of age, since it was decided to initiate the minimally invasive program in patients deemed most fragile, implanting a biological prosthesis without sutures, and a supported prosthesis to those belonging to the conventional surgery group.
The study met with the provisions of the Helsinki Declaration and was approved by the Ethical Committee of Cadiz University Hospital.
Variables analyzed
Demographic data, personal background, and risk factors for each patient were collected. Furthermore, intraoperative (total ischemia time) and PO data (intubation time, duration of stay in the critical care unit, need for reoperation, among others) were collected, especially the mortality variable in the first 30 days after surgery, by means of the electronic medical history. These variables are divided into two large types:
-
- Independent variables, which are, in turn, subdivided into three subgroups:
Sociodemographic: comprising, age, sex, and body surface
Smoking and comorbidities, which are arterial hypertension, chronic obstructive pulmonary disease, dyslipidemia, and diabetes mellitus
Surgical technique or treatment, New York Heart Association (NYHA) scale, ischemia time, heart rate, left ventricular ejection fraction (LVEF), and type of valve lesion
-
- Dependent variables:
Mortality
Hospital stay in intensive care unit (ICU)
Total hospital stays
Bleeding in the first 24 h of the PO period
Mediastinitis
Reoperation due to bleeding
Reoperation due to other causes
Intubation time: more or <24 h
Respiratory complications: pleural effusion, pneumonia, respiratory infection, atelectasis, and respiratory.
Data analysis
All data obtained have been entered and processed in an Excel® anonymized and encrypted database. Then, they were exported to a Statgraphics data file, where they were statistically processed. Subsequently, the data obtained were analyzed using SPSS statistical programs and applications. Furthermore, to describe the qualitative variables, overall frequencies and percentages were calculated and the ones for each group individually, as well as the 95% confidence index (CI95). However, to describe the quantitative variables, the means and typical deviations together with their 95% confidence interval were calculated, checking first normality with the Kolmogorov-Smirnov test, using the Student’s t-test for variables that met the normality criteria and the Mann–Whitney U-test for variables which did not follow normality criteria. Subsequently, pre-operative variables for both groups were analyzed to evaluate whether there were significant differences in said characteristics. Finally, the dependent and independent variables of both groups were compared to find statistical differences, using regression and bivariate correlation analysis.
Regarding regressions, depending on the variables to be compared, two types were used:
- Logistic regression, if the dependent variable is qualitative
- Multiple linear regressions when the dependent variable is quantitative.
In multiple linear regressions, to evaluate the results, five prior requirements were checked: normality of errors, homoscedasticity, independence of errors, and non-multicollinearity. In respect of the bivariate correlations, whose aim is not causality, but whether one variable is significantly related to another. Thus, if a nominal qualitative variable was correlated with another qualitative one, Cramer’s V test was employed (with a value > 0.6 to be a fairly acceptable correlation and > 1 to be perfect), while if a qualitative variable correlated with another qualitative one the Eta Coefficient was employed (with the same values), with a statistical significance (Sig.) lower or equal to 0.05.
Results
In the analysis of the pre-operative characteristics of both groups in this study, no statistically significant differences were found, except in the sex and LVEF variables. This latter was conserved in the entire conventional surgery group and mainly conserved in the minimum access one. For the rest, both groups may be deemed equivalent, as shown in table 1.
Table 1 Analysis of the pre-operative characteristics
| Mini-sternotomy (n = 57) (%) | Sternotomy (n = 57) (%) | p-value (p < 0.05) | |
|---|---|---|---|
| Age | 73.98 (72.75-75.21) | 72.23 (70.84-73.62) | 0.107 |
| Body surface | 1.78 (1.73-1.82) | 1.79 (1.74-1.83) | 0.689 |
| Female sex | 38 (66.7) | 22 (38.6) | 0.005 |
| Smoking | 14 (24.6) | 19 (33.3) | 0.409 |
| BP | 45 (78.9) | 40 (70.2) | 0.390 |
| DM | 19 (33.3) | 15 (26.3) | 0.539 |
| DLP | 38 (66.7) | 32 (56.1) | 0.248 |
| COPD | 2 (3.5) | 1 (1.8) | 1 |
| NYHA | |||
| I | 0 (0) | 1 (1.8) | 0.531 |
| II | 32 (56.1) | 33 (57.9) | |
| III | 25 (43.9) | 22 (38.6) | |
| IV | 0 (0) | 1 (1.8) | |
| LVEF | |||
| Preserved | 51 (89.5) | 57 (100) | 0.012 |
| Diminished | 6 (10.5) | 0 (0) | |
| Sinus | |||
| Rhythm | 52 (91.2) | 47 (82.5) | 0.355 |
| AF | 4 (7) | 7 (12.3) | |
| Pacemakers | 1 (1.8) | 3 (5.3) | |
| Type of valve lesion | |||
| Stenosis | 45 (78.9) | 43 (75.4) | 0.680 |
| Regurgitation | 2 (3.5) | 1 (1.8) | |
| Mixed | 10 (17.5) | 13 (22.8) |
COPD: chronic obstructive pulmonary disease; DLP: dyslipidemia; DM: diabetes mellitus, LVEF: left ventricular ejection fraction; BP: blood pressure.
Regarding determination of normality of the quantitative variable using the Kolmogorov–Smirnov test; it was found that only the body surface variable had a normal distribution, as shown in table 2:
Table 2 Determination of normality of the quantitative variables using the Kolmogorov–Smirnov test
| Statistics | DF* | Sig. | |
|---|---|---|---|
| Age | 0.092 | 114 | 0.019 |
| Body surface | 0.083 | 114 | 0.052 |
| Clamping time | 0.118 | 114 | 0.000 |
| Bleeding in first 24 h | 0.164 | 114 | 0.000 |
| Stay in ICU | 0.286 | 114 | 0.000 |
| Hospital stay | 0.240 | 114 | 0.000 |
*Degree of freedom
ICU: intensive care unit.
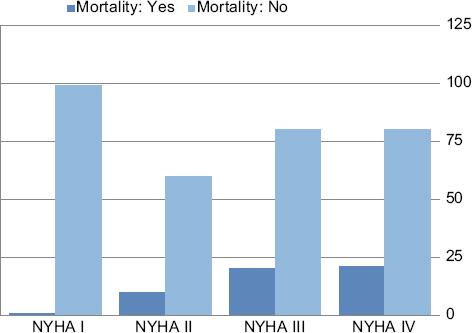
Concerning the results of the logistic regression of the main variable in this study, PO mortality, no statistical differences were observed when they were compared with the sociodemographic variables, smoking and comorbidities, nor with the third group of independent variables. However, in the bivariate correlations, when comparing the mortality variable with each of the variables individually, statistical significance was found in their analysis both with the surgical technique variable and the NYHA variable. Thus, the minimally invasive technique is correlated with the lower mortality compared to the conventional technique, with a low-power Cramer’s V, but with statistical significance, as shown in tables 3 and 4. On the other hand, the greater the NYHA scale of patients the more it correlates with mortality, with a more acceptable Cramer’s V (above 0.6) and statistical significance, as shown in figure 1.
Table 3 Bivariate correlation mortality versus technique or surgical treatment
| Technique | Total | ||
|---|---|---|---|
| Mini | Sternotomy | ||
| Mortality | |||
| Yes | 0 | 5 | 5 |
| No | 54 | 50 | 104 |
| Total | 54 | 55 | 109 |
Table 4 Cramer’s V bivariate correlation versus technique or surgical treatment
| Value | Approximate significance | |
|---|---|---|
| Nominal by Nominal | ||
| Phi | - 0.217 | 0.023 |
| Cramer’s V | 0.217 | 0.023 |
| No. of valid cases | 109 |
With regard to the results obtained with logistic regression for the reoperation variable due to bleeding, no statistical significance was found, only in the 3rd group was it encountered with the surgical technique variable. However, there was no statistical significance in the correlations of this variable with the rest of the variables in this study, except, once again, in the surgical technique, with a low Cramer’s V.
The results obtained in the logistic regressions of the intubation time and respiratory complications variables showed no statistical significance, not even in the correlations, only in minor variables such as body surface or type of lesion. Concluding with the logistic regression results, in the reoperation due to other causes variable, there was no statistical significance, and not with the bivariate correlations either.
However, the results of the multiple linear regressions, in which the quantitative variables were analyzed (total hospital stay, admission to ICU, and bleeding in the first 24 h), in the total hospital stay and time in the ICU, statistical significance was found in favor of the conventional surgery group, regarding three variables: surgical technique, NYHA, and ischemia time. In this way, these results show that the conventional technique is related to lower admission times, both in the ICU and total, probably influenced by the first cases of the learning curve for mini-sternotomy, which had more incidents in its early development and admission time. As regard the NYHA scale and ischemia time, these results show that the greater the NYHA scale and the longer the ischemia time, the longer the admission time, are shown in table 5. These results analyzed with the corresponding analysis of variance (ANOVA) showed that said regression presented acceptable results and with statistical significance.
Table 5 Linear regression hospitalization ICU versus 3rd group of variables
| ICU | Technique | NYHA | Ejection | Rate | Lesion | Ischemia | |
|---|---|---|---|---|---|---|---|
| Pearson correlation | |||||||
| ICU | 1.000 | - 0.225 | 0.213 | - 0.059 | - 0.035 | - 0.048 | 0.168 |
| Technique | - 0.225 | 1.000 | - 0.073 | - 0.189 | 0.191 | 0.103 | 0.199 |
| NYHA | 0.213 | - 0.073 | 1.000 | 0.066 | 0.006 | - 0.142 | - 0.174 |
| Ejection | - 0.059 | - 0.189 | 0.066 | 1.000 | 0.025 | - 0.101 | 0.003 |
| Rate | - 0.035 | 0.191 | 0.006 | 0.025 | 1.000 | 0.027 | 0.103 |
| Lesion | - 0.048 | 0.103 | - 0.142 | - 0.101 | 0.027 | 1.000 | 0.013 |
| Ischemia | 0.168 | 0.199 | - 0.174 | 0.003 | 0.103 | 0.013 | 1.000 |
| Sig. (unilateral) | |||||||
| ICU | 0.020 | 0.026 | 0.297 | 0.376 | 0.333 | 0.063 | |
| Technique | 0.020 | 0.255 | 0.043 | 0.041 | 0.175 | 0.035 | |
| NYHA | 0.026 | 0.255 | 0.276 | 0.480 | 0.099 | 0.057 | |
| Ejection | 0.297 | 0.043 | 0.276 | 0.410 | 0.180 | 0.490 | |
| Rate | 0.376 | 0.041 | 0.480 | 0.410 | 0.404 | 0.176 | |
| Lesion | 0.333 | 0.175 | 0.099 | 0.180 | 0.404 | 0.454 | |
| Ischemia | 0.033 | 0.035 | 0.057 | 0.490 | 0.176 | 0.454 | |
| N | |||||||
| ICU | 84 | 84 | 84 | 84 | 84 | 84 | 84 |
| Technique | 84 | 84 | 84 | 84 | 84 | 84 | 84 |
| NYHA | 84 | 84 | 84 | 84 | 84 | 84 | 84 |
| Ejection | 84 | 84 | 84 | 84 | 84 | 84 | 84 |
| Rate | 84 | 84 | 84 | 84 | 84 | 84 | 84 |
| Lesion | 84 | 84 | 84 | 84 | 84 | 84 | 84 |
| Ischemia | 84 | 84 | 84 | 84 | 84 | 84 | 84 |
ICU: intensive care unit; NYHA: New York Heart Association.
However, no statistically significant results were found in the correlations or variables for ICU admission or total hospital stay.
Finally, in respect of the linear regression results for the bleeding in the first 24 PO h variable, these only showed statistical significance in the 3rd group of independent variables, specifically in these two: technique and type of lesion. These results are probably due to the greater need for reintervention due to bleeding in the 1st h in the first cases of the mini-sternotomy group. However, in the corresponding ANOVA, it can be seen that these results are not very adequate or significant. As regard the correlations of the bleeding in first 24 h variable, no statistical significance was found with any of the variables analyzed individually.
Discussion
Minimal access surgery has shown numerous advantages, such as shorter stay in the ICU, less bleeding, fewer respiratory complications, and among others. It has also been established that it is a safe approach in terms of mortality, especially for AVR4. Concerning safety of the technique, and hence related mortality, in our study, despite the small sample size, we have been able to establish that minimally invasive surgery correlates with a lower mortality rate compared to the conventional technique, with a low but statistically significant Cramer’s V, it being implanted furthermore in patients over 65 years of age with aortic disease. In the study by Paredes et al., mortality in the mini-sternotomy group was practically 0%, while that of the sternotomy group was 5%, with an evaluation of comorbidity in each group using the EUROSCORE risk scale, the most used in cardiac surgery, presenting no statistically significant differences between both techniques. In the Mihaljevic et al. study, it was not statistically significant, but the early mortality rate was lower in the minimum access group compared to the conventional one, 2% as against 2.7%, respectively4,5.
With regard to total hospital stay and PO stay in the ICU, according to the literature, in our study, the results did not show in favor of said technique; moreover, they favored the conventional surgery group in the regressions analyses. This is probably due to the first cases of the minimally invasive approach which returned a larger number of incidents in the early PO period and which, for this reason, lengthened stay times. Furthermore, it highlights that in the results of the bivariate correlations, no statistical significance was obtained; therefore, the surgical technique variable does not correlate significantly with the total hospital stay and ICU stay time. Likewise, being a small sample, these first cases probably had a greater effect on the results.
However, in published studies, such as the one by Khoshbin et al., a meta-analysis, they obtained statistical significance in the lower average stay in the ICU variable of the mini-sternotomy group, and in the study by Mihaljevic et al., patients in the AVR group undergoing the minimum access technique had a lower mean total hospital time, a higher percentage being discharged in < 4 days, resulting statistically significant4,5.
In the published literature concerning intubation time and the emergence of respiratory complications, we can find, by way of example, that in the study by Filip et al., the mean intubation time in the mini-sternotomy group was 8 h, while the mean of the sternotomy group was 10 h, with a (p = 0.045), and that in the study by Young et al., a difference of 2 h was obtained in the mean intubation time across both techniques, in favor of mini-sternotomy. For its part, the study by Paredes et al. a retrospective study of 615 patients undergoing AVR, of whom 83 were operated on using minimum access surgery, it was encountered that the minimally invasive group presented a lower proportion of cases of pleural effusion, respiratory failure, and respiratory infection2,6,7. The results of our study do not show the aforementioned, given that no statistical significance in favor of minimum access surgery in either the regressions or in the corresponding correlations, probably due to the following:
- A huge advance in the PO handling of mechanical ventilation, with an ever increasing tendency, whatever the surgical approach employed, toward fast track and ultrafast track8.
- The learning curve associated with a new technique, with more precise incisions, and more unstable sternal closures in comparison to when it is an internalized technique such as conventional sternotomy.
Another advantage associated with minimum access surgery is lower emergence of PO bleeding, since lesser surgical aggression produces less bleeding, as well as the need to reoperate for this reason. In our study, average bleeding was lower in the mini-sternotomy group compared to the sternotomy one, with a mean of 247.02 ml compared to an average of 285.79 ml, without being statistically significant. While, in the results of the linear regression analysis, the bleeding in the first 24 h variable was statistically significant compared to technique and type of valve lesion variables, consequently despite presenting a lower bleeding average, the mini-sternotomy group showed greater need for reoperation due to bleeding in the immediate PO period. This is probably due to the first cases of the learning curve, where the basics of this new technique were being established.
Notwithstanding, it is to be highlighted that the ANOVA analysis of this regression shows that these results are not very adequate or significant. This variable is difficult to evaluate due to the fact that a multitude of factors affect it, such as prior antiaggregant/anticoagulant drugs taken by the patient, among others. Besides, in our center, it coincided with the implantation of the system of assessment of the state of coagulation, thromboelastography, or ROTEM, which enables patient coagulation to be evaluated, as well as guide the transfusion strategy, which helped management of PO bleeding. In the literature, the meta-analysis by Phan et al. did not find any difference in the need to reoperate, whether for bleeding or for any other cause, between groups, and in the study by Filip et al., the need for further intervention caused by bleeding in the sternotomy group was greater6,9.
As far as the need for further intervention for other causes is concerned, in the results of our study, a greater need for further intervention due to incidents with the drainage tube (entrapment of the tube or absence of/poor drainage) was found in the mini-sternotomy group, due especially to the early cases, in which learning was taking place about where best to place said tube and more incidents occurred with this. Once the learning curve had been overcome no further incidents took place. This is reflected in the results of the regressions for this variable, in which no statistical differences were found between each group.
Furthermore, minimum access surgery has been called into question, because it is related to longer ischemia times, especially in the learning curve. However, the advent of sutureless prostheses has enabled prosthesis implantation time to be reduced, as was demonstrated in the study by Young et al., where the combination of mini-sternotomy and sutureless prosthesis achieved a reduction in clamping time, with a mean of 41 min compared to a mean of 54 min in the sternotomy group, with p < 0.00017. In our study, no statistical significance was reached in the ischemia time in the minimum access group and the conventional surgery one, with means of 60 min and 64 min, respectively, which is probably due to the learning curve associated with a new surgical technique, as well as the curve associated with implantation of a new prosthesis.
In the rest of the variables in our study, mediastinitis, heart rate, and type of valve lesion, no statistically significant differences were obtained between both groups. What we would like to highlight is that LVEF did obtain a statistically significant difference in favor of the sternotomy group, since it could explain the more insidious PO period, in which some patients in the minimum access group presented, due to interventions being performed with greater deterioration of contractility.
Study limitations
- Because it was retrospective, it prevents correct planning as well as randomization of patients
- Being a recently implanted technique with certain inclusion criteria, the resulting sample is small. It is also affected by the fact that many patients over 65 years of age with aortic disease are referred for percutaneous treatment
- The lack of data for some patients made it impossible to calculate the EuroSCORE scale.
Conclusions
Minimum access cardiac surgery for AVR is a safe technique in our environment, correlating with lower PO mortality compared to the conventional technique. For this reason, it is an alternative that should be considered by the Heart Team, both to conventional surgery, and other treatment techniques, such as percutaneous routes, in patients over 65 years of age with aortic disease. Furthermore, it is an increasingly mainstream approach; in which PO management is very important for favoring more rapid recovery.
However, our study has not been able to show any other advantages associated with minimally invasive surgery, above all regarding hospital stay and in the stay in ICU, probably due to the sample size and due to the inevitable learning curve linked to every new surgical technique and new valve prosthesis.











 nueva página del texto (beta)
nueva página del texto (beta)