Introduction
Approximately 7% of men present fertility problems during their lives, resulting in a public health issue1,2. Male infertility is a complex pathology defined by the failure to achieve a clinical pregnancy after 12 months of regular unprotected sexual intercourse, according to international consensus3. Male contribution to infertility represents 45%–50% in childless couples4,5. Diagnosis is made based on abnormal semen analysis according to the WHO criteria. Based on sperm count, patients can be classified as azoospermic, defined as the absence of sperm in at least two different ejaculate samples (including the centrifuged sediment), or oligozoospermic when sperm account is <15 million/mL. In addition, severe oligozoospermia is considered with sperm concentration <5 million/mL and criptozoospermia when sperm is only visualized after centrifugation6. Azoospermia is classified into two groups: 1) obstructive, caused by obstructive factors along the seminal pathways, and 2) secretory or non-obstructive azoospermia (NOA), which is commonly related to gonadal dysfunction. NOA is explained by genetic factors in 21%–29% of cases, whereas in 12%–41% of cases, the cause is idiopathic and probably related to unknown genetic factors7-9. The main genetic cause involved in male infertility are abnormalities of the Y chromosome10, such as numerical and structural alterations. In addition, epigenetic modifications, such as decreased DNA methylation of the IGF2-H19 region, autosomal gene mutations, i.e. in the gene CFTR and in the X chromosome, the CAG polymorphism in the androgen receptor gene, have also been involved11-13. Of interest is the azoospermia factor region (AZF region) localized on Yq, which contains genes involved in the control of male meiosis14. Six AZF regions are known, AZFa, AZFb, AZFc, and their combinations15. Non allelic homologous recombination between repetitive sequences can lead to chromosome deletions or duplications, this mechanism is believed to account for the random appearance of de novo AZF microdeletions16. AZF microdeletions have been proved to be in a clear cause-effect relationship with spermatogenic impairment14,17,18. Microdeletions are detected in 10%–15% of patients with NOA and 5%–10% of patients with severe oligozoospermia19,20. The most frequent deletion occurs in the AZFc region (~80%), followed by AZFb (1%–5%), AZFbc (1%–3%) and AZFa (0.5%–4%)21. Patients harboring deletion of AZFa can present hypo-spermatogenesis and inhibition of the production and maturation of germ cells22,23. The phenotype observed in patients with AZFb deletion is a pre-meiotic arrest with normal spermatogonia and primary spermatocytes. AZFb overlaps with the AZFc region24. The AZFc region contains critical transcripts for normal spermatogenesis. Spermatid or sperm maturation anomalies have been found in patients with AZFc microdeletions17.
While the analysis of AZF deletions have been introduced as a routine genetic test for infertile patients, the role of partial AZFc deletions, i.e., gr/gr deletion, b1/b3, and b2/b3, has been the focus of long-lasting debate. The risk associated with this genetic anomaly varies between populations, reaching the highest OR in Italians (OR 7.9, 95% CI 1.8–33.8)25. Current evidence suggest that the gr/gr deletion is a significant risk factor for impaired sperm production.
We designed the present study to analyze the frequency of microdeletions in the AZF region in a group of Mexican mestizo infertile men.
Materials and Methods
Patients
This study was performed at the Genetics and Genomics Department of the National Institute of Perinatology in Mexico during a four years period, all procedures were approved by the institutional ethics committee. Patients with idiopathic infertility were referred from the Andrology Department. Participants were invited to the study and signed an informed consent form. A total of 57 patients were included, 26 had azoospermia and 31 had severe oligozoospermia (12 criptozoospermic and 19 oligozoospermic), all of them underwent to a GTG karyotype. The control group was composed by 55 males with normal spermatobioscopy.
Molecular analysis
Genomic DNA was isolated from peripheral blood with the Wizard Genomic DNA Purification Kit (Promega) according to the manufacturer´s instructions. A NanoDrop 2000 Spectrophotometer (Thermo Scientific) was used to determine DNA purity and concentration.
Two multiplex PCR reactions were performed to analyze the AZFa, AZFb, and AZFc regions and singleplex PCR reaction to analyze the gr/gr region, as described elsewhere18. The multiplex PCR reaction employed the primers ZFX/Y, sY86, sY127, sY254 and the singleplex used the primers sY14 (SRY), sY84, sY134, and sY255. We confirmed the deletions using a single PCR reaction. For amplification of the gr/gr region, we used the primers sY1291 and sY1191. The heterochromatic Yq region was analyzed with the sY160 marker. The list of primer sequences, and expected product sizes has been previously published18.
Each multiplex or singleplex PCR reaction contained 0.7–1 mg of DNA, 200 nM of each primer and 1.5 units of HotStarTaq Master Mix Kit. Cycling conditions were as previously described20. PCR products were size separated by electrophoresis in a 2.5% agarose gel (Invitrogen, Carlsbad, CA, USA).
Statistical analysis
Descriptive statistics are presented for all variables. Kruskall Wallis test was performed to evaluate quantitative variables. Pearson`s χ2 test was used to compare proportions between study groups.
A multilayer perceptron neural network model was executed to determine whether the presence of a determined deletion could predict azoospermia, criptozoospermia, or oligozoospermia. A classification and regression tree (CRT) was later used to corroborate neural network predictions and as a predictive model for azoospermia, cryptozoospermia, or oligozoospermia, according to the presence of deletions in the different regions analyzed. Lastly, another CRT model was executed to determine whether the number of deletions in the evaluated regions could be related to any of the three diagnoses. Statistical analyses were performed using IBM SPSS Statistics (Armonk, NY, USA), version 22. The significance level was a = 0.05.
Results
We analyzed 55 individuals with normal spermatobioscopy as controls and 57 diagnosed with infertility. All participants had a normal karyotype. Within the infertility group, 26 were azoospermic (45.6%) and 31 were severely oligozoospermic, from these, 12 (21.1%) were criptozoospermic and 19 (33.3%) oligozoospermic. The mean age of participants was 32.7 (SD 6.7) years and mean semen sample volume was 2.56 (SD 1.86) mL. Kruskall Wallis tests showed no significant difference in participants’ age and semen sample volume among the different diagnoses (azoospermia, cryptozoospermia, and oligozoospermia).
None of the controls presented microdeletions within the STSs analyzed. We found a microdeletion in 9 (15.8%) individuals from the infertility group. When we compared the proportion of individuals with microdeletions through a Pearson X2 test we observed a statistically significant difference (p=0.002) (Table 1).
Table 1 Percentage of patients and controls with and without microdeletions
| Group | Without deletion n (%) | With deletion n (%) | Total | P* |
|---|---|---|---|---|
| Patients | 48 (84.2%) | 9 (15.8%) | 57 | 0.002 |
| Controls | 55 (100%) | 0 | 55 | |
| Total | 103 (92.0%) | 9 (8.0%) | 112 |
*Statistically significant difference between patients and controls by Pearson χ2.
Table 2 shows the number of patients with microdeletions according to the clinical diagnoses within the infertility group. We did not find statistically significant differences when comparing individuals with azoospermia versus severe oligozoospermia (Pearson X2 test, p=0.615).
Table 2 Proportion of azoospermic or severe oligozoospermic patients with microdeletions
| Diagnosis | Without deletion | With deletion | Total |
|---|---|---|---|
| Azoospermic | 22 (84.6 %) | 4 (15.4%) | 26 |
| Severe oligozoospermic | |||
| Criptozoospermic | 9 (75%) | 3 (25%) | 12 |
| Oligozoospermic | 17 (89.5%) | 2 (10.5%) | 19 |
| Total | 48 (84.2%) | 9 (15.8%) | 57 |
No statistically significant differences were observed between azoospermic and severe oligozoospermic patients by Pearson χ2 (p = 0.615).
Among azoospermic patients, one had a complete deletion of the AZFb region (absence of sY127 and sY134 markers; Figure 1A and B, patient AZP3). Another had a complete deletion of the AZFc region (absence of sY254 and sY255 markers, AZP4) (Fig. 1A and B). Two of them had the gr/gr microdeletion (absence of sY1291 and presence of sY1191 markers, patients AZP1 and AZP2) (Fig. 1C). Within the severe oligozoospermic group, two patients had a complete deletion of the AZFc region (Fig. 1A and B) (patients SOP4 and SOP5). Patient SOP4 presented absence of the sY1291 gr/gr marker (Fig. 1C), while patient SOP5 had absence of both gr/gr markers (Fig. 1C). One patient had a partial microdeletion of AZFc (absence of sY254 marker, SOP3) (Fig. 1A). Another had a complete gr/gr microdeletion (absence of sY1291 marker, SOP1) (Fig. 1C). Another patient presented a partial gr/gr microdeletion (absence of sY1191 marker, SOP2) (Fig. 1C). Table 3 summarize microdeletions findings.
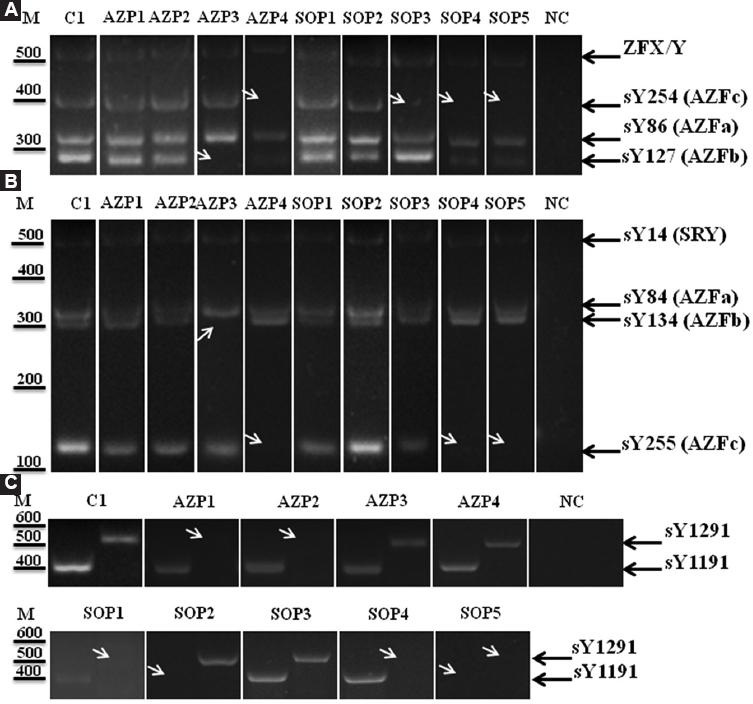
Figure 1 AZFa, AZFb, AZFc, and gr/gr microdeletions in azoospermic or severe oligozoospermic Mexican patients. A: representative image of multiplex PCR reaction A to analyze the presence/absence of STS sY86 (AZFa), sY127 (AZFb) and sY254 (AZFc), and the positive control ZFX/Y. B: representative image of multiplex PCR reaction B to analyze the presence/absence of STS sY84 (AZFa), sY134 (AZFb) and sY255 (AZFc), and the positive control sY14 (SRY). C: representative image of singleplex PCR reactions to analyze the presence/absence of STS sY1291 and sY1291. White arrows show the presence of microdeletion. AZP: azoospermic patients, C: controls, NC: negative controls, SOP: severe oligozoospermic patients.
Table 3 Summary of Y-chromosome microdeletions found in infertile patients
| Diagnosis | AZFb | AZFc | gr/gr | |||
|---|---|---|---|---|---|---|
| SY127 | SY134 | SY254 | SY255 | SY1291 | SY1191 | |
| Azoospermic AZP1 | X | |||||
| Azoospermic AZP2 | X | |||||
| Azoospermic AZP3 | X | X | ||||
| Azoospermic AZP4 | X | X | ||||
| Severe oligozoospermic SOP1 (Criptozoospermic) | X | |||||
| Severe oligozoospermic SOP2 (Criptozoospermic) | X | |||||
| Severe oligozoospermic SOP3 | X | |||||
| Severe oligozoospermic SOP4 (Criptozoospermic) | X | X | X | |||
| Severe oligozoospermic SOP5 | X | X | X | X | ||
A multilayer perceptron neural network model using the sigmoid activation function was performed to determine if the presence of deletions in the sY127, sY134, sY254, sY255, sY1291, or sY1191 regions were associated with azoospermia, cryptozoospermia, or oligozoospermia. The data were divided randomly into a training group (70%) and a holdout group (30%) with n1/n2 cross-validation to evaluate the accuracy of the network model. The model was re-run several times with different random starting seeds to ascertain that the results were consistent. The area under the curve for azoospermia, cryptozoospermia, and oligozoospermia in the training set were 0.640, 0.643, and 0.635, respectively. The model accurately predicted 54.3% of training cases. The regions with the highest importance to the model were sY254 (100%), sY1191 (99%), sY1291 (66.8%), and sY255 (65.2%). The predicted values for deletions in the regions with highest importance to the model according to diagnosis are presented in Figure 2. The model predicted that deletions in sY1191 were more likely related to oligozoospermia, while deletions in sY1291 were more related to azoospermia and deletions in sY254 were more related to cryptozoospermia. A follow-up CRT decision tree indicated that deletions in the sY1191 region were mainly associated with oligozoospermia (n = 2, 100%), whereas the absence of deletion in sY1191 and the presence of deletion in sY254 were mostly related to cryptozoospermia (n = 2, 66.7%) and to azoospermia (n = 1, 33.3%). On the other hand, neither deletion in sY1191 nor deletion in sY254, accompanied by a deletion in sY1291 was mainly related to azoospermia (n = 2, 66.7%) and to cryptozoospermia (n = 1, 33.3%) (data not shown). The most important predictive variables in the model were sY1191, sY254, and sY1291. It is noteworthy that none of the patients with azoospermia or cryptozoospermia had deletions in sY1191.
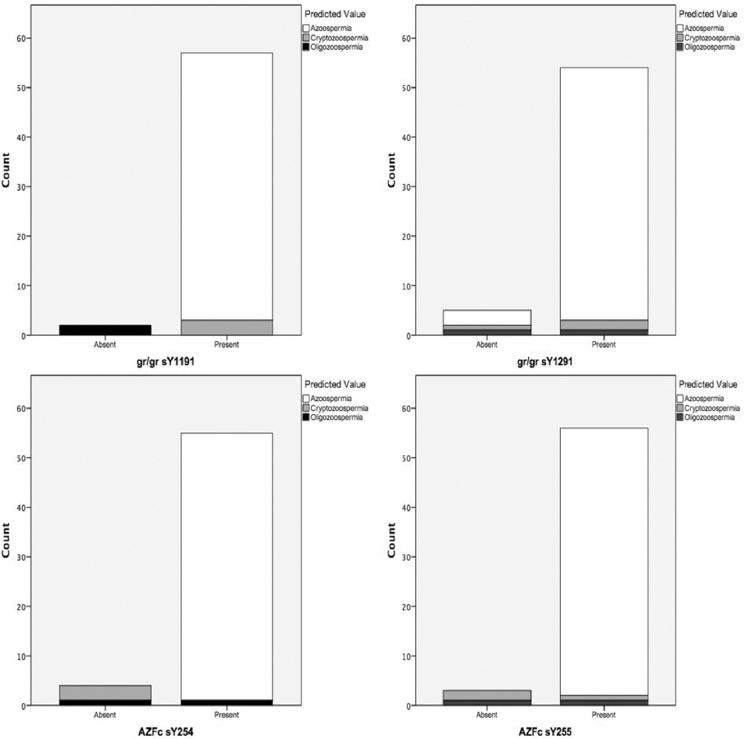
Figure 2 Stacked bar charts of the predicted values for azoospermia, oligozoospermia, and cryptozoospermia according to microdeletions obtained from a neural network model. The top left bar chart shows that the model predicted that patients with the sY1191 deletion were more likely to be oligozoospermic. The top right bar graph shows that the model predicted that patients with sY1291 deletions were more likely to be azoospermic. The bottom charts show that the model predicted that patients with sY255, and especially those with sY254, were more likely to be cryptozoospermic (criptozoospermic and oligozoospermic).
Finally, a CRT model was executed to determine if not only the presence of deletion for each region but the total number of deletions could predict any of the three diagnoses. The tree indicated that the most important independent variable predicting diagnosis was the total number of deletions (normalized importance of 100%), followed by sY1191. The model showed that patients with deletions in the sY1191 region were more likely to have oligozoospermia, but patients with no deletion in the sY1191 and one or more deletions in any of the other regions were more likely to belong to the azoospermia or cryptozoospermia groups (57.1% and 42.9%, respectively). The decision tree is shown in figure 3.
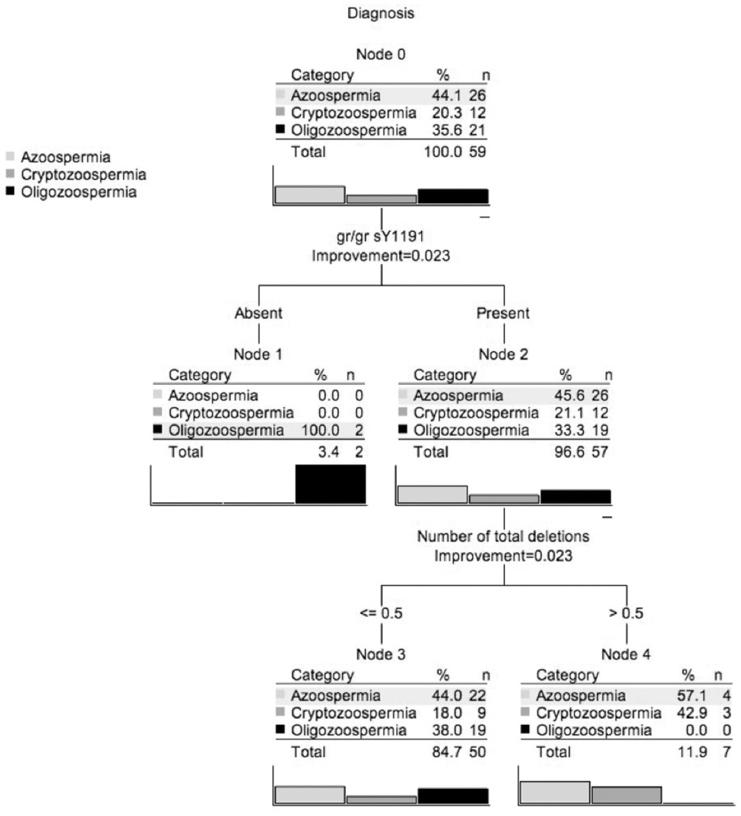
Figure 3 Classification and regression tree. The CRT indicates that the tree split first according to sY1191 deletions and that 100% of patients with this type of deletion had oligozoospermia. However, in those patients that did not have sY1191 deletions, the most important variable defining the infertility categories was the number of deletions per participant. The final nodes in the tree indicate that patients with one or more deletions were more likely to have azoospermia or cryptozoospermia.
Discussion
We investigated Y-chromosome microdeletions in patients diagnosed with infertility. We screened microdeletions using STS markers for the AZFa, AZFb, AZFc, and gr/gr regions. Regardless of deletion type, the overall deletion frequency in azoo-/severe oligozoospermic men was higher than in normozoospermic (15.8% vs. 0). The statistical analysis showed that microdeletions are significantly associated with infertility in our population (p = 0.002). This result suggests that such deletions could be a risk factor for impaired spermatogenesis in the Mexican population. There are few studies in Mexican populations analyzing the prevalence of Yq deletions in infertile men. Piña et al, studied the presence of Yq microdeletions in Mexican men from couples with recurrent pregnancy loss, they did not find microdeletions26. Martinez-Garza S.G, et al found that 12.2% of infertile males had microdeletions of AZFb or AZFc, however they did not analyze gr/gr microdeletions27. Our results, including gr/gr deletions, showed a higher percentage (15.8%), compared to their results. It is noteworthy that they used other STS markers, they found two patients with deletion of sY121 and/or sY128 in AZFb. However, the aforementioned markers are not included in the EAA/EMQN Guidelines 201320. These STS markers could be important in the analysis of Mexican populations and could be analyzed in future studies.
The impact of gr/gr deletions on male fertility is unclear. Gianchini et al, found that the frequency of gr/gr deletions was significantly higher in the infertile group compared to controls, suggesting a possible deleterious effect on spermatogenic efficiency. They reported an OR of 10.1, indicating that gr/gr deletions could be considered a risk factor for oligozoospermia28. However, other studies have not detected strong association. Hucklenbroich et al, did not find significant differences of gr/gr deletions in German population when compared men with NOA versus normospermic men29. A lack of association was also observed by Machev et al in Italian population30. They observed that 5.3% of infertile men (7/150) had gr/gr deletions compared to 0.5% of fertile individuals (1/189). Although these data suggested a significant association, from these seven patients, four were defined as idiopathic, one had a history of cryptorchidism and two had varicocele31.
In our study, from the infertile men who only presented a complete deletion of the gr/gr region, 2/26 were azoospermic (7.7%) and 1/31 (3.2%) had severe oligozoospermia (criptozoospermia). Whereas, none of the controls presented the deletion. There were significant differences in various parameters associated with semen quality in men with gr/gr subdeletions, mainly in the sperm concentration, which further reinforces the point that these mutations may be associated with spermatogenesis impairment. This observation has been described previously28. To further define the genotype-phenotype correlation, we found the role of partial gr/gr subdeletions to be more complicated than previously thought and probably is related to the study population32.
The Pearson χ2 test did not find differences in the STSs deleted between azoospermic and severely oligozoospermic patients. However, the neural network model showed that some STS deletions could be related to azoospermia, criptozoospermia, or oligozoospermia. The model showed that the sY1191 deletion could predict oligozoospermia, while the sY1291 deletion may predict azoospermia and the sY254 deletion could be related to criptozoospermia. These results were corroborated by a classification and regression tree (CRT). We also performed a CRT to determine if the number of deletions per patient could predict any of the diagnoses. Again, the CRT model showed that patients with deletions in the sY1191 region were more likely to have oligozoospermia, and patients without sY1191 deletion and one or more deletions in any of the other regions were more likely to be azoospermic or cryptozoospermic.
Although this study reports novel findings concerning the potential correlation between certain microdeletions with azoospermia, cryptozoospermia, and oligozoospermia, it has some limitations. Certainly, the sample size and the small number of microdeletions found may have influenced our results. A study with a larger sample size is necessary to confirm our results.
Future studies in larger groups should focus on the combined definition of the type and copy number of the AZFc genes deleted in men with partial deletions and the haplogroup of the Y chromosome. A detailed analysis of these and other yet unidentified genetic factors is necessary prior to offer assisted reproductive techniques.
Conclusions
Our findings corroborate the importance of microdeletions of the AZF region in infertile patients. Despite the controversy of the gr/gr deletion as a risk factor for male infertility, we did not observe this deletion in fertile controls. More studies with lager samples in ours and other populations are needed to define the gr/gr deletion as a factor compromising fertility. Nevertheless, the study of AZF microdeletions has to be included in the clinical approach of infertile males.











 nueva página del texto (beta)
nueva página del texto (beta)


