Introduction
Colonic lipomas (CLs) are benign, non-epithelial, fatty neoplasms with an incidence of 0.2% to 4.4%1. (1) Although infrequent, they are the second most common benign tumor of the colon, and 65-75% of the lipomas of the gastrointestinal tract occur in the colon, being the most frequently affected site2. (2) Mostly they are asymptomatic, and need no treatment; but around 25% of the cases may develop symptoms including bowel obstruction and intussusception3 (3); those larger than 4cm are considered giant and may be symptomatic in 75% of cases4. (4)
Intestinal conditions, such as intraluminal lesions alter bowel peristalsis and serve as a lead point to create an intussusception5(5). Although intestinal intussusception is a relatively common cause of bowel obstruction in children, it is uncommon in the adult population, causing <1% of bowel obstructions5. (5)
We report three cases of CLs in adult patients presenting with colo-colonic intussusception that required surgical management, the diagnosis was confirmed by histopathological examination of the specimens.
Case 1
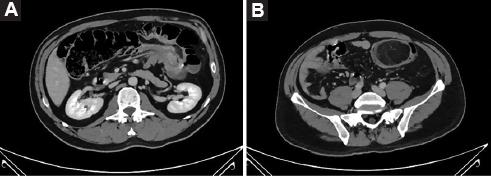
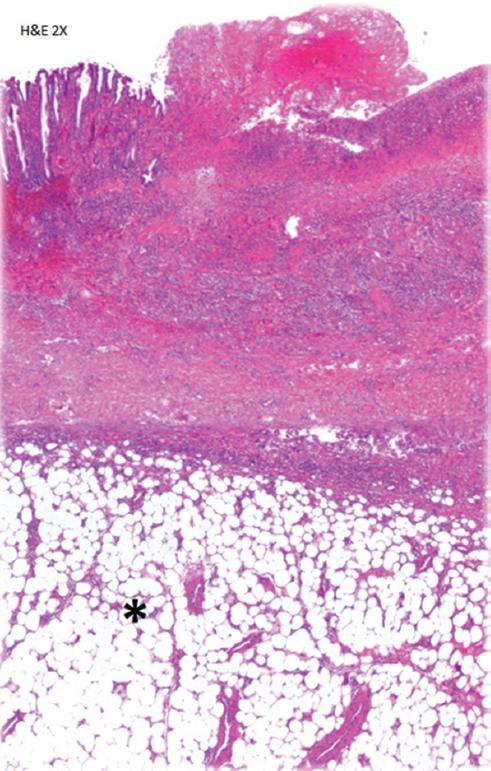
A 50-year-old male patient with no comorbidities complained of intermittent abdominal pain, change in bowel habits with constipation and narrow stools, associated with emesis, weight loss, and bloody stools. Colonoscopy and computed tomography revealed a 5.9x5.4x4.1cm mass located in the hepatic flexure of the colon. Right hemicolectomy with ileotransverse anastomosis was performed. He made an uneventful postoperative recovery. (Figs. 1-2)
Case 2
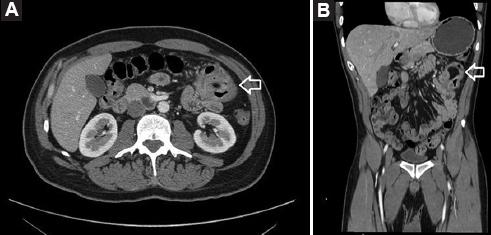
A 42-year-old male patient with a history of systemic arterial hypertension was referred to our surgical outpatient clinic with a one-year history of intermittent abdominal distension, diffuse abdominal pain, constipation, bloody stools, and weight loss. A colonoscopy showed a 3.5x2.7x2.6cm lesion in the transverse colon, on computed tomography an hypodense lesion with fat density was found, during colonoscopy the lipoma was ligated with an endo-loop to block the blood supply for ischemic resection; however, the lesion just developed ischemic changes but remained in place, so the patient was taken to surgery for segmental resection of the transverse colon. The patient progressed favorably, and was discharged without complications. (Figs. 3-4)
Case 3
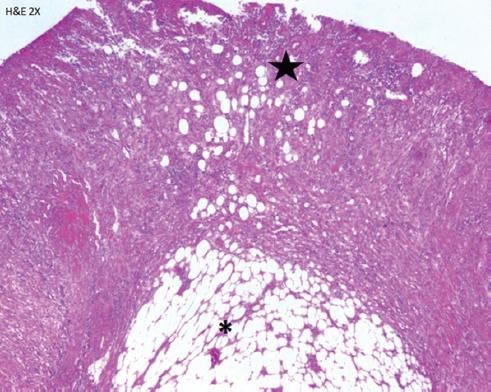
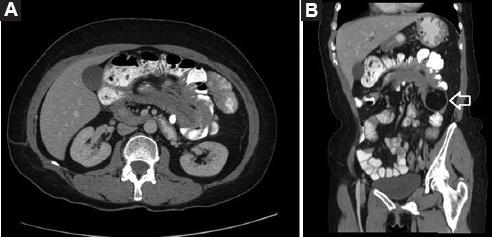
A 54-year-old female patient with no comorbidities was admitted to the emergency department, with an exacerbation of a chronic and intermittent diffuse abdominal pain, associated with change in bowel habits, nausea and vomiting.
On physical examination, the patient had soft abdomen with diffuse tenderness, without signs of peritoneal irritation. Abdominal computed tomography showed an ascending colo-colonic intussusception causing partial obstruction due to an intraluminal lipomatous mass of 5.1x5.5x3.4cm. A colonoscopy showed a subepithelial lesion located at the hepatic flexure of the colon with benign macroscopic characteristics. The patient was taken to right hemicolectomy with ileotransverse anastomosis and was discharged without complications (Figs. 5-6).
Discussion
Intussusception is common in children but infrequent in adults, around 95% of intussusceptions occur in pediatric population and the remaining 5% occur in adults6 (6), being the cause of <1% of cases of intestinal obstruction5 (5); meanwhile, colo-colonic intussusception represents 17% of all intestinal intussusceptions in adults7. (7) In a retrospective review of 44 cases of intussusception in adults, Honjo et al. found 12 enteric intussusceptions, 6 ileocolic intussusceptions, 16 ileocecal intussusceptions, and 10 colonic intussusceptions, of the latter only 1 case was of benign etiology7. (7)
Colonic lipomas measuring <2cm are usually asymptomatic, whereas those of >4cm are symptomatic in 75% of the cases8. (8) A review of the literature by Paskausas et al. analyzed 37 cases of CLs associated with intussusception, the ascending colon was the most frequently affected site9. (9)
An accurate preoperative diagnosis can be challenging since CLs have nonspecific clinical manifestations. Series of intussusception in adult patients report pain as the most common symptom (present in 71% to 90% of patients), and its intermittent characteristic favors a late diagnosis. Vomiting, and low gastrointestinal bleeding are the next most frequent10. (10)
Other symptoms include abnormal bowel habit, diarrhea, and anecdotally, patients may defecate an hemorrhagic tissue, due to the autoamputation of the lipoma11. (11)
In a review of adult intussusceptions by Azar et al., the mean duration of symptoms between onset and presentation was 37.4 days (range 1-365 days), and can be longer in patients with benign enteric lesions compared to those with malignant and colonic lesions5. (5)
Nowadays a great variety of diagnostic tools are available. Barium enemas show a filling defect, nonetheless, this finding is no specific for CLs. Computed tomography has been suggested as the preferred modality for diagnosing intussusception of CLs due to characteristic fatty densitometric values (-40 till -120 Hounsfield units)12,13.(12,13) However, intussuscepted lipomas may not demonstrate normal fat attenuation and may have heterogeneous appearance reflecting fat necrosis14. (14)
Magnetic resonance is particularly able to detect fatty lesions because of typical tissue signal intensity on T1-weighted and fat-suppressed images. However, this imaging method is rarely used to approach this type of lesions.
Colonoscopy may show CLs in the form of a yellow elastic submucosal mass, but sometimes hemorrhage, necrosis, and mucosal ulceration may be seen15. (15)
Regarding treatment, the general agreement is that CLs <2.0cm in diameter are accessible for endoscopic management, while this is not recommended for lesions >2.0cm due to the risk of complications16. (16)
For those patients taken for surgical treatment, formal colectomy and limited colon resection are considered as adequate treatment modality, particularly in those cases with a confirmed preoperative diagnosis17. (17)
According to Jiang et al., surgical intervention is appropriate when the lipoma is >4 cm in size; has associated intussusception and the patient is symptomatic, or when the lesion cannot be resected endoscopically18. (18) However, formal oncologic resections may be necessary in some cases if the diagnosis is uncertain.
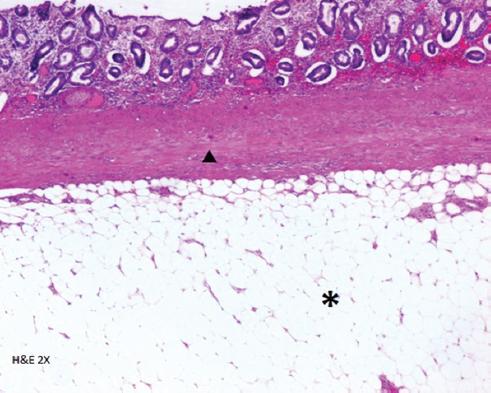
The definitive diagnosis is obtained from a histopathological exam19. (19) There are no reports of malignant transformations of CLs. However, some may have pseudosarcomatous changes when examined20. (20)
Conclusions
As CLs are uncommon, the diagnosis requires a high index of suspicion, and should be included in the differential diagnosis of symptomatic bowel tumors. Although intussusception itself carries a good prognosis, the most important prognostic factor is the nature of the lesion leading to the process.
Currently, surgery is still the treatment of choice, which depends on lipoma size, location, patient´s medical history, imaging, and intraoperative findings.











 nueva página del texto (beta)
nueva página del texto (beta)