Introduction
Undescended parathyroid adenomas are defined as glands located 1 cm or more cranial to the superior pole of the thyroid gland, and represent only 2-7% of the ectopic parathyroid adenomas. An ectopic location occurs in 16% of parathyroid adenomas. This makes undescended parathyroid adenomas a rare cause of primary hyperparathyroidism, accounting for just 0.91% of the cases or less1.
This anomaly is due to an undetermined error in the fetal development and normal descent of the parathyroid glands to their typical adult location. In the 5th week of the embryogenesis the parathyroid glands arise from endodermal epithelial cells2. The inferior parathyroid glands originate from the dorsal epithelium of the 3rd pharyngeal pouch with the thymus gland originating from the ventral aspect. The parathyroid migrates inferiorly and separates from the thymus to rest near the lower pole of the thyroid. The superior parathyroid glands originate from the dorsal epithelium of the 4th pharyngeal pouch and descend with the ultimobranchial body to reside close to the mid superior lobe. The superior parathyroid gland can fail to descend or end up in a more posterior location near the thyroid with less cranial-caudal displacement than the inferior parathyroid gland3.
Technetium sestamibi scintigraphy and ultrasound are the most common modalities used to localize adenomas and are often complementary. Historically, computed tomography (CT) imaging has generally been reserved for those patients in whom initial surgery has failed or those who have recurrent hyperparathyroidism despite treatment4. More recently, a 4D CT scan uses timed imaging after intravenous contrast to identify a hypervascular parathyroid adenoma. This imaging modality is helpful for adenoma localization when the initial studies are negative or for confirmation of a suspected ectopic parathyroid adenoma5.
Case 1
We present the case of a 57-year-old male who was discovered to have an elevated calcium for at least 1 year, complaining of tiredness and difficulty with his memory and concentration. There was a negative history of kidney stones or bone-related abnormalities. Clinical examination identified prominent submandibular salivary glands bilaterally (left > right), without any regional adenopathy, thyromegaly, venous distention, carotid bruit, tenderness, or any palpable thyroid nodules. Vital signs were blood pressure 141/86 mmHg, with a ventricular rate of 77 bpm. The previous testing revealed a 24-h urine calcium at 402 mg (normal values: 100-300 mg), serum calcium of 11.2 mg/dl (normal values: 8-10 mg/dl), parathyroid hormone (PTH) level of 208 ng/ml (normal values under 67 ng/ml), and low 25 OH Vitamin-D at 14 (normal 30-80). The patient had a parathyroid sestamibi scan at an outside institution. Images were taken at 15 min and 3 h after the injection of technetium sestamibi (Fig. 1). Images were reviewed by the surgeons. This demonstrated marked uptake in the left submandibular gland area compared to the right submandibular salivary gland. Delayed films appeared to indicate a separate focus of radioactivity to the initial uptake and persistent intense uptake in the left submandibular salivary gland area. These images suggested the possibility of an undescended parathyroid adenoma in the left neck but were not clearly diagnostic. A surgeon-performed cervical ultrasound examination revealed a normal sized thyroid and without imaging any abnormal parathyroid glands in the central neck near the thyroid gland or in the lower paratracheal area (Fig. 1). The lateral and upper neck were imaged with ultrasound looking for the possibility of an undescended parathyroid adenoma and initially, a small nodule was discovered medial to the bifurcation of the left common carotid artery that was felt to represent the rare presence of a lymph node medial to the carotid artery bifurcation or an undescended parathyroid adenoma. The patient underwent a 4D CT scan with spiral CT imaging without contrast and then arterial phase and venous phase imaging after the injection of intravenous contrast (Fig. 2). This revealed a 9.3 mm × 19.2 mm enhancing nodule medial and posterior to the distal left common carotid just inferior to the carotid artery bifurcation. A large left submandibular salivary gland was confirmed. Directed reexamination of the left lateral and upper neck with surgeon-performed ultrasound identified a deep hypoechoic nodule of 1.92 × 0.78 × 1.01 cm located medial and posterior to the bifurcation of the left carotid artery. Laterally, this was close to the level of the thyroid cartilage notch. On the basis of this evidence the patient underwent a targeted left neck exploration and excision of the abnormal parathyroid gland using gamma probe localization of the adenoma after the injection of technetium sestamibi 1 h before the operation, intraoperative PTH monitoring, and intraoperative nerve monitoring (Fig. 3). The gamma probe skin counts were 4600 counts/s. A 2.5 cm transverse incision in the direction of a natural skin crease was made over the lateral border of the sternohyoid muscle and medial border of the sternocleidomastoid muscle. The dissection was carried down between the sternohyoid and sternocleidomastoid muscles, medial to the identified carotid artery, down to the deeper cervical tissues. A small nodule was palpable there consistent with a possible parathyroid adenoma. The in vivo gamma probe counts over this nodule were 5500 counts/s indicating the likelihood of this nodule being a parathyroid adenoma. The nodule was carefully mobilized up into the wound, ligating feeding blood vessels before excising. The ex vivo gamma counts of the nodule were 2000 counts/s (36% of in vivo gamma counts), confirming the nodule as consistent with a parathyroid adenoma. The intraoperative PTH levels dropped from 245 preincision to 121 preexcision and then 40.9 and 32.8, respectively, 5 and 10 min after the excision of the undescended parathyroid gland. The gland weighed 1130 mg and was confirmed by pathology as a parathyroid adenoma.

Figure 1 Initial Image Studies; A.- Parathyroid Sestamibi Scan performed at 15 min after the Tecnessium Sestamibi injection B.- 3 h after injection. A: left Submandibular gland. B: apparent separate focus of ratio activity. C: longitudinal Neck Ultrasound depicting a hypoechoic nodule medial to the bifurcation of the left carotid artery. D: axial cut.
Case 2
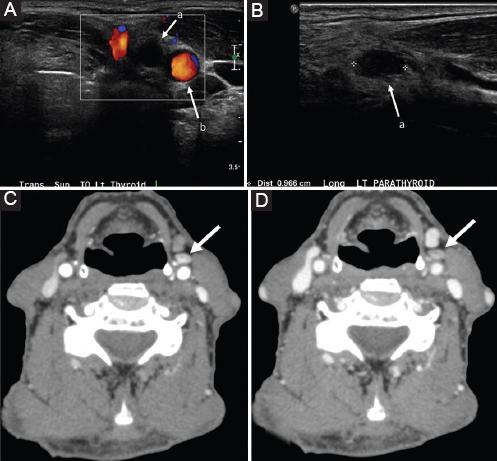
An 80-year-old male with a history of Parkinsonism presented for evaluation of hypercalcemia secondary to primary hyperparathyroidism. Recent calcium level was elevated most at 10.7, with a prior level of 11.7 and a PTH of 74 at the same time. Vitamin D level was 59. He was experiencing fatigue, weakness as well as problems with concentration and memory which he also attributed to his Parkinson’s. A surgeon-performed cervical ultrasound examination revealed a normal sized thyroid without imaging any abnormal parathyroid glands in the central neck near the thyroid gland or in the lower paratracheal area (Fig. 4). The lateral and upper neck were imaged with ultrasound looking for the possibility of an undescended parathyroid adenoma and initially, found a single nodule medial to the bifurcation of the common carotid artery that was felt to represent the rare presence of a lymph node medial to the carotid artery bifurcation or an undescended parathyroid adenoma. Fine-needle aspirate (FNA) with PTH of the nodule was done. He underwent a 4D CT scan with spiral CT imaging without contrast and then arterial phase and venous phase imaging after the injection of intravenous contrast (Fig. 4). This revealed an oval nodule measuring 7 x 5 mm anterior to the left common carotid artery just below the bifurcation. The lesion was isodense to musculature on precontrast sequence with marked arterial enhancement and partial washout on venous phase. Ultrasound-guided FNA reported cellular aspirate with bland overlapping cells and no colloid. Immunostain for PTH was reported negative, but in light of the clinical suspicion of parathyroid gland, and despite the equivocal PTH stain, morphologic features were highly suggestive of parathyroid tissue. Therefore, a 2 ml saline washout from FNA of suspected ectopic parathyroid was performed reporting PTH, FNA: 9724 pg/ml. On the basis of this evidence the patient underwent a targeted left neck exploration and excision of the abnormal parathyroid gland using intraoperative PTH monitoring and intraoperative nerve monitoring (Fig. 5). A 2.5 cm transverse incision in the direction of a natural skin crease was made over the lateral border of the sternohyoid muscle and medial border of the sternocleidomastoid muscle. The dissection was carried down between the sternohyoid and sternocleidomastoid muscles, anterior to the identified carotid artery. A small nodule was palpable there consistent with a possible parathyroid adenoma. The nodule was carefully mobilized up into the wound, ligating feeding blood vessels before excising. The intraoperative PTH levels dropped from 58 preincision to 23 preexcision and then 9 and 8, respectively, 5 and 10 min after the excision of the undescended parathyroid gland. The gland weighed 0635 mg and was confirmed by pathology as a parathyroid adenoma.
Discussion
Persistent hyperparathyroidism after failed cervical exploration usually occurs in < 10% of these procedures6 and is due to an ectopic parathyroid adenoma in 7% of cases7. For these patients, the identification of an occult lesion is key in decreasing morbidity associated with surgical exploration8. It has been stated that the major cause of operative failure is the surgeon’s inability to find the abnormal parathyroid glands (76.2%)9 and most cases of persistent or recurrent HPT after parathyroidectomy are due to missed glands in normal or ectopic locations10. For cases whereby sonography and sestamibi do not reproduce localizable lesions, evaluation with a cross-sectional imaging technique may be necessary. Studies have shown increased rates of recurrent laryngeal nerve injury and permanent hypocalcemia in patients who underwent reoperation for persistent primary hyperparathyroidism11.
What imaging protocol would work best for identifying an undescended parathyroid adenoma before a central neck parathyroid exploration? Ultrasound by an experienced endocrine radiologist or endocrine surgeon should be attempted first. A parathyroid adenoma clearly seen in the central neck supports proceeding with a focused parathyroid exploration. Examination of the upper neck medial to the carotid arteries should be done if no central neck parathyroid adenoma is identified. Undescended parathyroid adenomas are typically located medial to the bifurcation of the carotid artery. Lymph nodes in the upper neck are typically lateral to the carotid artery and medial or lateral to the internal jugular vein. Therefore, under these circumstances, finding a hypoechoic nodule medial to the bifurcation of the carotid artery without clear imaging evidence of a lymph node with a hyperechoic fatty hilum should raise suspicion for an undescended parathyroid adenoma. The approach to ectopic parathyroid adenomas generally requires confirmation with a second imaging study, either a technetium sestamibi nuclear medicine scan or 4D CT scan. However, it has been reported that initial nuclear medicine parathyroid sestamibi scan can read as within normal limits12 and even though the use of sestamibi SPECT/CT can reduce false negative interpretations on technetium 99 m sestamibi scintigraphy13, we would favor the 4D CT imaging majorly due to its anatomic clarity compared with technetium 99 m sestamibi scintigraphy and its higher diagnostic performance when compared with sestamibi SPECT/CT. Alternately, an undescended parathyroid adenoma that can be seen on ultrasound lends itself to further evaluation with FNA that includes PTH aspirates14. An elevated PTH aspirate confirms the presence of parathyroid tissue. The key to discovering an undescended parathyroid adenoma is the initial suspicion when the central neck ultrasound is negative for a parathyroid adenoma, leading to scanning the upper neck medial to the carotid arteries, followed best with a 4D CT scan for anatomic localization of the relatively hyper vascular parathyroid adenoma.
Conclusion
Undescended parathyroid adenomas are rare and are likely to be missed on standard parathyroid workup. It is an ectopic site that merits attention on any patient not only after a failed central neck exploration but should be considered when ultrasound imaging of the central neck is negative for a parathyroid adenoma. The appropriate imaging protocol uses ultrasound imaging medial to the carotid artery that can potentially identify the undescended parathyroid adenoma near the bifurcation of the carotid artery (Fig. 6). The localization can then be confirmed with a 4D-CT scan, nuclear medicine technetium sestamibi scan, or ultrasound-guided PTH aspiration. Localization directs primary minimally invasive parathyroidectomy surgery in the upper neck through a small incision.











 text new page (beta)
text new page (beta)