Introduction
Stereotactic brain biopsy (SBB) is used for establishing the histological diagnosis of intracranial lesions that, in view of their location or imaging characteristics, are not amenable for a direct surgical approach1.
Frame-based system has generally been considered the gold standard method for obtaining SBB2 over the frameless technique, although without significant differences in the diagnostic success between the two techniques, which are estimated in different reports to be between 89 and 94%2-5. Since SBB, although considered minimally invasive, is a surgical procedure carrying on some risks, it is important to optimize its success in providing a conclusive diagnosis6-8. In the present report we evaluated the diagnostic success of a frame based system SBB, having an intra-operative evaluation by a neuropathologist of the adequacy of multi-sample material obtained for histopathological analysis, against the complication rate of the procedure.
Materials and methods
We performed a retrospective analysis of 140 consecutive cases with intracranial lesions demonstrated by enhanced Magnetic Resonance Imaging (MRI) and operated over a period of 53 months (February 2014-June 2018). Patients considered for SBB were those in whom the location of lesions or their possible etiology precluded an open surgical intervention. Therefore, the aim of SBB was to establish the histological diagnosis of lesions for defining the most appropriate therapeutic approach in each patient.
The procedures were performed at the Unit for Stereotactic and Functional Neurosurgery of Mexico General Hospital.
One hundred and eight cases corresponded to suspected neoplastic lesions. Twenty (14%) of them benefited by subsequent ressective or tumor reduction surgical procedures. Others underwent chemotherapy and/or radiotherapy based on the histopathological diagnosis. Eighty-four (60%) were lesions located in eloquent areas, and thirty-six (24%) lesions in patients with comorbidities, functional impairment, or advanced age that increased risk for a major surgical procedure. Lesions were intracerebral subcortical, deeply located in the frontal 26%, temporal 10%, parietal 9%, and occipital 2% lobes, thalamus 19%, corpus callosum 7%, periventricular 4%, pineal region 4%, basal ganglia 7%, infratentorial 5%, and 6% were diffuse or multifocal (Table 1). Thirteen (9%) were cases associated to human immunodeficiency virus (HIV).
Table 1 Anatomic location of brain lesions
| Location | n | % |
|---|---|---|
| Frontal | 36 | 26 |
| Thalamus | 27 | 19 |
| Temporal | 14 | 10 |
| Parietal | 12 | 9 |
| CorpusCallosum | 10 | 7 |
| BasalGanglia | 10 | 7 |
| Brainstem | 7 | 5 |
| Paraventricular | 6 | 4 |
| Pinealregion | 5 | 4 |
| Occipital | 3 | 2 |
| Sellarregion | 1 | 1 |
| Multifocal | 9 | 6 |
| Total | 140 | 100 |
All cases had a contrasted MRI. Axial T1 Weighted images sequence 1.0 mm thick was used for planning the stereotactic approach. Patients signed an informed consent approved by the Institutional Ethics Committee Board that complies with Helsinki declaration. Demographic data, clinical and radiographic characteristics are presented as measures of central tendency. Analyses of differences between categorical variables were performed with the Chi-square test. p < 0.05 was considered statistically significant.
Under local anesthesia the Zamorano-Dujovny (ZD) stereotactic frame (FL Fischer, Freiburg, Germany) was placed aligned to the orbitomeatal plane. An enhanced cerebral computed tomography (CT) was obtained under stereotactic condition with 2 mm thick slices without interval. Stereotactic surgical planning used the PRAEZIS® software (Praecis AG, Heidelberg, Germany) of fused MRI and the enhanced CT for defining trajectories avoiding vascular structures. The targets for taking samples also avoided areas with restricted diffusion in the MRI sequences, considering those areas with great proportion of necrotic tissue and therefore with poor diagnostic value.
For biopsies in the pineal region trajectories were carefully planned avoiding the ventricular system and vascular structures, verifying the trajectory in the CT-MRI multiplanar images of the software. Precoronal entry point was preferred for lesions located nearby frontal, temporal, basal ganglia, and hypothalamus. Postcoronal entry point was used for lesions in the upper brainstem, periventricular, and corpus callosum. The parietal entry point was used for parietal and occipital lesions, and the sub-occipital entry point with inverted frame positioning was used for cerebellar lesions. At least, two targets were planed per patient and defined in the x, y, and z planes.
Procedures were performed under local anesthesia and mild sedation in most instances. The pre-established coordinates were verified in the stereotactic frame prior starting the procedure. Burr hole performed with a 14 mm auto-stop drill centered at the stereotactic cranial entry point. Dural opening performed by burning the dura using the monopolar cautery applied to the tip of the biopsy needle, avoiding cerebrospinal fluid drainage that might create a brain shift. Aspiration through a biopsy needle with a 2.5 mm lateral window at the side of the needle tip was obtained. Typically, sampling included the four quadrants of the needle obtaining 2.3 mm samples. Thereafter, biopsy needle was advanced 2.5 mm below the first sampled site and sampling was repeated in the same manner, obtaining a total of 8 samples. Neuropathologist in the operating room received and labeled the biopsied samples, staining them with Hematoxylin-Eosin. After an immediate microscopic examination, he evaluated if sampling was satisfactory for diagnosis. In those cases where the tissue obtained was not sufficient for the neuropathologist, the biopsy needle was directed to the 2nd target and the neuropathologist evaluated the biopsy material in the same way. One the biopsy was declared satisfactory for diagnosis; all samples were immersed in a paraffin block and taken to the neuropathology department for specific staining and immunohistochemistry, according to the type of lesion and the needs for its identification.
To rule out subclinical complications and to corroborate the adequate biopsied site, CT was performed within 24 h after the surgical procedure in all cases and fused with the pre-operative studies.
Results
Among the 140 SBB from February 2014 to June 2018, there were 79 (56%) men and 61 (44%) women. The mean age was 45 years (standard deviation [SD] 15.9 years). Histological diagnosis was performed in 131 of the 140 cases (94% overall diagnostic yield). The presurgical radiological diagnosis was correct in 39% of the cases. The mean hospital stay was 1.5 days. Of the 140 biopsied cases, 108 (77%) corresponded to neoplastic lesions and 32 (23%) were non-neoplastic. We performed craniotomy and resection after biopsy in 14% of cases (n = 20).
Regarding neoplastic lesions, high-grade astrocytomas (Glioblastoma WHO G IV and anaplastic astrocytoma WHO GIII) were the most frequently diagnosed group 40% (n = 56), we found an increase in the mean age of these patients (50.4 ± 15.6 years) compared to the rest of the sample. The radiological diagnosis was correct in 34%. Subsequent craniotomy and resection was performed in only six cases (9%).
The second group in frequency corresponded to low-grade astrocytomas (WHO GI and GII), we found 19 cases (14%), with a correct radiological diagnosis in 48% and a subsequent need for complete resection in 32% (n = 6). We documented ten metastasis (7%), primary tumors were identified in 90% of cases (six lung, two melanoma, and one thyroid), the radiological diagnosis was correct only in 20% of the patients and only one required complementary surgical management (Table 2).
Table 2 Histopathology of Stereotactic brain biopsies
| Neoplastic Lesions 108 (77%) | n (%) | MRI % accuracy |
|---|---|---|
| Glioblastoma | 41 (29) | 34 |
| Anaplasticastrocytoma | 15 (11) | 33 |
| Lowgradeastrocytoma | 9 (6) | 44 |
| Lymphoma | 8 (6) | 50 |
| Diffuseastrocytoma | 6 (4) | 50 |
| Pilocyticastrocytoma | 4 (3) | 50 |
| Germcelltumors | 5 (4) | 40 |
| Ganglioglioma | 2 (1) | 0 |
| Meningioma | 2 (1) | 50 |
| Centralneurocytoma | 2 (1) | 100 |
| Anaplasticoligodendroglioma | 1 (1) | 0 |
| Primitiveneuroectodermaltumors | 1 (1) | 0 |
| Pineocytoma | 1 (1) | 0 |
| Gliomatosiscerebri | 1 (1) | 0 |
| Metastasis | 10 (7) | 20 |
| Non neoplastic lesions 32 (22.9%) | n (%) | |
| Toxoplasmosis | 6 (4) | 66 |
| Tuberculoma | 2 (1) | 100 |
| Abscess | 2 (1) | 100 |
| HIV encephalitis | 2 (1) | 0 |
| Demyelinating process | 2 (1) | 0 |
| Venous angioma | 2 (1) | 100 |
| Syphilitic Gumma | 1 (1) | 0 |
| Neurocysticercosis | 1 (1) | 0 |
| Cerebral amebiasis | 1 (1) | 0 |
| Progressive multifocal leukoencephalopathy | 1 (1) | 0 |
| Vasculitis | 1 (1) | 100 |
| AVM | 1 (1) | 100 |
| Actinomyces spp | 1 (1) | 0 |
| Non diagnostic | 9 (6) | |
| Inflammation | 4 (3) | |
| Gliosis | 4 (3) | |
| Lymphoid infiltration | 1 (1) | |
Regarding non-neoplastic, toxoplasmosis was the most frequent lesion 4% (n = 6), followed by tuberculoma, abscesses, HIV encephalitis, demyelinating processes, and venous angioma (1% each). The radiological diagnosis was correct in 47% of infections and 100% of vascular etiologies (Fig. 1).
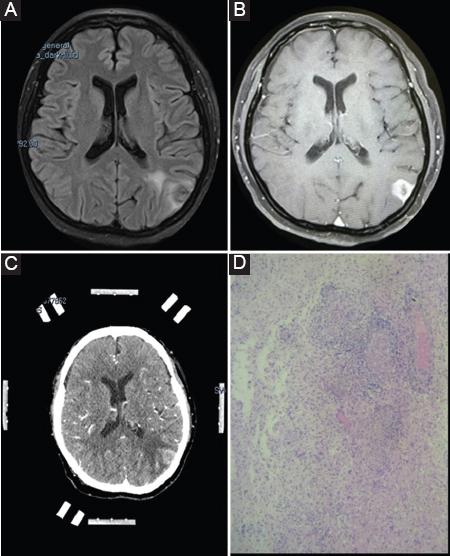
Figure 1 An illustrative case of a 50-year-old female patient with a left occipital lesion in whom the SBB radically changed diagnosis and treatment. A: FLAIR MRI and B: T1-enhanced in axial view showing a heterogeneous cortical lesion, with medium enhancement and central hypointense areas. C: Axial enhanced-CT with the stereotactic frame prior to the surgical procedure. D: Histopathological 100x with acute inflammation over a chronic granulomatous process with focal areas of necrosis and vasculitis. Before the SBB, a neoplastic lesion was suspected, the final result was a syphilitic gumma.
In 9 (6%) cases, the diagnosis could not be determined by the SBB. In these patients, the mean age was 40.22 ± 12.2 years, there were 8 men (89%). Radiological diagnosis corresponded to: 3 high-grade astrocytomas, 2 tuberculomas, 2 lymphomas, and 2 metastases. With respect to the location, we found 5 frontal, 2 brainstem, 1 thalamus, and 1 basal ganglia lesion (Table 2).
In 20 patients (14%), a complementary resection was performed after a certain diagnosis obtained by SBB. Of these, 10% of glioblastomas (n = 4), 100% of pilocytic astrocytomas (n = 4), 33% of diffuse astrocytomas (n = 2), 33% of anaplastic astrocytomas (n = 2), 100% of meningiomas (n = 2), 100% of arteriovenous malformations (n = 1), 50% of venous angiomas (n = 1), 50% of central neurocytomas (n = 1), 50% of gangliogliomas (n = 1), 12.5% of lymphomas (n = 1), and 10% of metastases (n = 1).
Failure in diagnosis was significantly associated with male gender (p = 0.041) and HIV patient’s lesions (p = 0.038).
Complications
We performed a post-operative CT scan for all patients looking for early complications. During our observation period, one death was documented, in a patient with a paraventricular temporal lesion with massive intraventricular hemorrhage in the post-operative period who ultimately had a diagnosis of low-grade astrocytoma. We documented three patients with small local bleedings in the biopsy area, all of whom did not require complementary surgical management, one of these cases corresponded to symptomatic hemorrhage with focal paresis of the right arm without posterior impact on clinical functionality. Symptomatic postoperative edema occurred in two patients requiring complementary management with dexamethasone 8 mg BID. In three patients pneumocephalus was documented by post-operative CT scan without clinical symptoms.
Discussion
In this 53 month retrospective study, we report important data about frame-based SBB in a tertiary referral hospital in Mexico. We found that high-grade astrocytomas were the most frequently diagnosed lesions, with high diagnostic accuracy (94%) and low number of complications (6%).
As in other series, the majority of patients were men in the fourth and fifth decades of life (61%), which correlates with the higher incidence of high grade astrocytomas in this age span9,10.
Lobar subcortial lesions were the majority 46%, followed by diencephalic 19%, and deep seated in 18%, this is similar to that previously described in other series8,11. Tilgner et al.,12 reported that biopsies of tumors located in the parietal lobe are more accurately diagnosed than those in other locations. In our cases, the location of the lesion was not associated with a better diagnostic accuracy.
According to that previous reported regarding diagnoses, all the series agree that high-grade astrocytomas (WHO Grades III and IV) are the most biopsied lesions, followed by central nervous system lymphomas and metastases. Nevertheless, the proportion of high-grade astrocytomas in our series is greater (40%) that the previously reported by other authors (21%13, 26%14, 32%10,11, and 34%15), this can be partly due by ethnic differences in our population, unknown to the best of our knowledge.
Regarding non-neoplastic lesions, we found a higher proportion of toxoplasmosis (4%) compared to other series (1%16), where the most reported findings were abscess, radionecrosis, and vascular lesions such as infarctions11,12,14. This can be explained by a large number of biopsied HIV patients in our series (9%).
When comparing the pre-surgical radiological diagnosis with the SBB result, we found that it was reliable only in 39% of cases, with better performance in the case of vascular (100%) and infectious lesions (47%). This data are comparable to that previously reported by Tilgner and collaborators (30%)12, but is far from those reported in the Quick-Weller series (76%)17, although the latter takes into account only lesions of the brainstem, which could facilitate radiological diagnosis. Any parameter we take, supports the use of SBB, since the reliability of the radiological diagnosis is low, so relying on the latter, can result in inappropriate treatment.
With respect to postoperative complications (6%), the occurrence of hemorrhage at the biopsied site is the most frequent complication as reported in other studies (2-8%)8,10,11,16,18 and was present in 2% of our cases, being the cause of death in one patient, and only demonstrated by post-operative CT scan in two patients. Of the nine cases reported in our series as complications, two were secondary to cerebral edema corresponding to 1% of the series. Transient neurological deficit was another complication, most likely secondary to edema at the biopsied site10,14,19. In three patients intracranial air collection was evident in post the post-operative CT scan, without clinical symptoms, not requiring further treatment and without demonstrable image displacement of the stereotactic objective. We found no information regarding this complication in the literature.
In the previous reports, mortality secondary to SBB was settle from 1% to 2%14,15,19. Risk factors associated with mortality are size of the lesion to be biopsied, particularly for neoplasms; increase in neovascularization, which confers a greater possibility of edema and hemorrhage and patients with a lower degree of functionality16,19,20.
Accurate histological diagnosis is essential for the patient´s appropriate and effective treatment options according to the type of brain lesion. The overall diagnostic yield of SBB in our series was 94%, being among the highest in the literature. This number is comparable to that previously described by Nishihara et al. 97%18, Hall et al. 95%14, and Waters et al., 95%7. Success of SBB derives from surgeon’s experience, which improves diagnostic performance up to 10%21, having in the operating room an experienced neuropathologist analyzing the adequacy of the biopsied material7,12,15, the nature of biopsied lesions, being easier to determine the diagnosis in high grade tumors8,12,15, and the number of samples obtained13,22. Furthermore, lesions > 1 cm7 represent an easier target to approach. The high diagnostic accuracy in our study is most likely related to the conjunction of these factors. When conducting an intentional search for what we consider to be a primary factor for success in diagnostic performance, which is the presence of a neuropathologist who determines the adequacy of the sample, we find that the existing evidence supports this hypothesis. Tsermoulas et al. found that the failure in diagnosis decreased from 7% to 6% when incorporating the neuropathologist for the trans-surgical review of the sample obtained23. It is the same case of Hall et al. whom reported an increase in diagnostic performance from 80% to 96%14. On the other hand, in the studies where the biopsy was not evaluated in the surgery, diagnostic yields were reported between 83%13 y 86%10.
Complementary surgical resection was performed in 20 cases (14%); data that agrees with that previously reported in other series such as that of Lara-Almunia et al. 20%21 and Kim et al. 15%15. In the present study, in all these 20 cases there was a diagnostic doubt of neoplastic versus infectious etiology, when neoplastic lesion was confirmed by SBB, the complementary resection was performed.
The limitation of the present study is its retrospective design, which does not allow us to evaluate the variables that could affect the overall diagnostic performance.
Conclusion
Frame-based SBB continues to be a safe, useful and inexpensive procedure, requiring but 2-3 days hospitalization, particularly for those cases where cytoreduction is not a first instance option, either due to the location of the lesion or the patient´s physiological status. The diagnostic performance of SBB increases when strategies such as the intraoperative cytological evaluation by a neuropathologist are included in the study. A higher number of biopsy samples also increases diagnostic accuracy.











 nova página do texto(beta)
nova página do texto(beta)


