Introduction
Atherosclerosis is a systemic pathology involving the entire vascular system. Smoking, hyperlipidemia, diabetes mellitus, and hypertension are known risk factors for the development of atherosclerosis. These risk factors also increase the incidence of peripheral arterial disease (PAD)1,2. Advanced age is an additional risk for PAD due to atherosclerosis3,4.
PAD includes occlusive or aneurysmatic diseases of aorta and all aortic branches except coronary arteries5. PAD treatment includes Mediterranean type nutrition, lifestyle changes, and medical treatments as well as interventional and surgical treatments6,7. With the recent advances in technology, endovascular treatment options are frequently preferred instead of surgical treatment, especially in high-risk patients they have other comorbidity factors with PAD8,9. Although surgical revascularization is accepted as the gold standard treatment in distal PADs, endovascular treatment options are also very important in distal PADs due to morbid and mortal complication risks such as graft thrombosis, graft infections in long-term follow-ups10,11. According to The Inter-Society Consensus for the Management of PAD (TASC II), lesions in the lower extremity arteries are classified as Type A, B, C, and D lesions. Endovascular interventions are preferred in Type A lesions and surgical interventions are preferred in Type D lesions. In Type B and C lesions, endovascular or surgical interventions can be applied depending on the condition of the patient and concomitant diseases. However, endovascular interventions in Type B lesions and surgical interventions in Type C lesions should be prioritized12.
It is known that parameters such as heart rate, mean arterial pressure, and arterial oxygen saturation (SaO2) used during pediatric cardiac surgery operations are not always sufficient to show real tissue oxygenation13. The use of near-infrared spectroscopy (NIRS) method has come to the agenda to show tissue oxygen saturation. For this purpose, the NIRS method was started to be used with the INVOS (Covidien, Somanetics, Troy, MI.) device. It is stated that the device shows the saturation of the watershed zone, which is a mixture of 1/3 arterial blood and 2/3 venous blood at a depth of 1-1.5 cm from the skin14. In a case with complex aortic pathology and requiring reoperation, the follow-up of tissue oxygenation with NIRS from two anatomic regions (cerebral and right thigh) during the pre-operative period has been reported to make them aware of the right leg ischemia that developed after placing a cross-clamp into the aorta15. In the study of Toraman et al., there was a correlation between NIRS measurement and tissue oxygen saturation16. In our study, we aimed to present the effectiveness of atherectomy, drug-eluting balloon, and combined therapy with values determined by NIRS in patients they have PAD.
Patients and methods
Ethical explanation
Ethical approval was not required since it was a retrospective study. The head of the clinic and all the authors approved the submission and publication of this study. After explaining the interventions, risks, and benefits in detail as a policy of the health system in the country, informed consent was obtained from the relatives of each patient before the procedures.
Materials and methods
Patients with intermittent claudication or critical leg ischemia (Rutherford class 3 or more) have been viewed in the study. There were 30 male and 9 female patients. Patients were followed up before the procedure, at the 1st h after the procedure, and at the 3rd month after the procedure, with simultaneous ankle-brachial pressure index (ABPI) measurements, walking distance measurements, and measurement of tissue oxygenation by NIRS method. Patients with under 1-year life expectancy, have paclitaxel allergy and antiplatelet therapy contraindicated patients were excluded from the study. During the procedure, the ipsilateral or contralateral femoral artery was used for entry. Following the 6F sheath placement, 100 IU/kg heparin was given to the patients as standard dose.
Twenty-six patients received drug-eluting balloons. Thirteen patients underwent atherectomy and received drug-eluting balloons. The determination of the need for atherectomy was based on the degree of calcification of the arterial structure, the patient's age, the duration of the symptoms, and the resistance to the predilatation balloon.
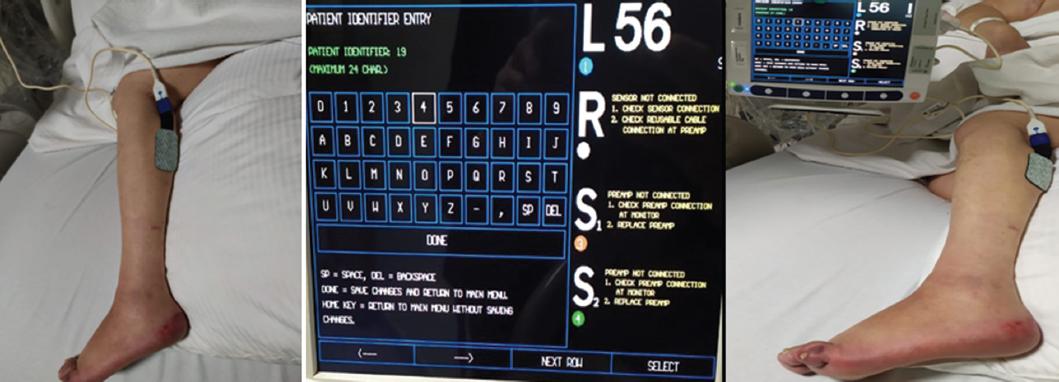
NIRS probe was placed on the skin of the same side gastrocnemius muscle of all patients underwent to the procedure (Fig. 1). All patients were treated under mild sedation with 2 l/m nasal oxygen mask.
Following the passage of the lesion with guidewire in the drug-eluting balloon group, predilatation was performed with a standard balloon (Fig. 2). 4.5-7 mm thick and 100-250 mm long balloons were used. Balloon opening times were determined for an average of 3 min. The time was extended by opening the balloon again in case of being an inflow reducing dissection or > 40% stenosis. When the target inflow was achieved, the process was terminated. Following the loading of 300 mg clopidogrel after the procedure, antiplatelet treatment was applied by 75 mg clopidogrel p.o. and 100 mg aspirin p.o. daily. At the end of the 3rd month, ABPI and walking distance measurement were performed. Tissue oxygenation was evaluated simultaneously with the NIRS method. The patients were followed up with 100 mg aspirin p.o daily.
In the group of patients who underwent an atherectomy and received a drug-eluting balloon, after the passage of the lesion with guidewire, predilatation was performed with a standard balloon. Turbohawk catheter (Covidien Mansfield, MA, USA) was used as an atherectomy device. 4.5-7 mm thick and 100-250 mm long balloons were used. Balloon opening times were determined for an average of 3 min. The time was extended by opening the balloon again in case of being an inflow reducing dissection or > 40% stenosis. When the target inflow was achieved, the process was terminated. Following the loading of 300 mg clopidogrel after the procedure, antiplatelet treatment was applied by 75 mg clopidogrel p.o. and 100 mg aspirin p.o. daily. At the end of the 3rd month, ABPI and walking distance measurement were performed. Tissue oxygenation was evaluated simultaneously with the NIRS method. The patients were followed up with 100 mg aspirin p.o daily.
In the 3rd month, it was decided to evaluate with peripheral angiography in patients with a decrease in ABI value and to re-initiate in case of detection of restenosis. No restenosis was detected in any of the control patients. Medical follow-up continued.
Results
Pre-operative NIRS results and post-operative NIRS results were compared in both patient groups. NIRS value was found to be 45.8% preoperatively, 77.2% postoperatively, and 79.7% at 3rd month in the patient group undergoing atherectomy. The success of the procedure was 100% in the 3rd month controls of the combination of atherectomy and drug-eluting balloons. The NIRS value was found to be 52.7% preoperatively, 71.6% postoperatively, and 69.9% on the 3rd month in the patient group received only drug-eluting balloon. When all the results were evaluated, it was determined that the increase in blood flow in the tissues was higher in patients who received combined therapy. In addition, similarity was detected between both patient groups in pre-operative and post-operative ABPI measurements.
Discussion
The frequency of PAD increases in society with the increasing awareness and increasing awareness of its pathophysiology. However, with the development of interventional materials used, lesions that could not be treated many years ago can be treated today7.
Risk of amputation and early deaths in the long-term are less common in distal PADs than iliofemoral occlusive diseases. Endovascular methods are preferred more frequently as a treatment of distal PADs with the developing technology. However, the biggest problem in endovascular treatment is restenosis17,18. In addition to balloon angioplasty and stent implantation, atherectomy was added as a treatment method into the other endovascular procedures to prevent restenosis18. With increasing experience, stents have been replaced by medicated balloons and atherectomy in the endovascular treatment of distal PADs.
Atherectomy procedure was performed for the 1st time in 1985 as percutaneous for resection of calcific plaques19. When atherectomy patients were evaluated with short and long-term follow-ups, similar results were found with other endovascular procedures20,21. To prevent the development of restenosis in patients undergoing atherectomy, drug-eluting balloons were started to be used22. It has been reported that drug-release balloons prevent the development of restenosis due to platelet inhibition and growth factor release properties22.
In a study comparing only drug-eluting balloons and standard balloons, in early follow-up, no significant difference was initially detected between the two groups, but at the end of 1 year, the clinical improvement in the medicated balloon group was significantly higher. In addition, the rate of limb recovery in the drug-eluting balloon group was found to be 82.0% at the end of 1 year, while it was 65.6% in the standard balloon group and it was reported that the drug-eluting balloon group was statistically superior in terms of amputation rates23. In a study in which atherectomy and drug-eluting balloon was used together, the opening rate was 90% in the early period and 100% in the long term22. In another study which atherectomy and drug-eluting balloon were combined, these rates were found to be 85.7-92.9%23.
Toraman et al. showed that NIRS reflects tissue oxygenation rate to a depth of 1.5 cm16. This result supports the angioma hypothesis to demonstrate tissue microcirculation.
Conclusion
Although NIRS mainly shows venous oxygenation in the tissue, it is known that high venous oxygenation in tissues is valuable for microcirculation and collateral vascular circulation. When patients with similar post-operative ABPI measurements were evaluated with NIRS, venous oxygenation was observed higher in patients used treatment methods combined with atherectomy. According to these results, we thought that treatment methods combined with atherectomy has increased microcirculation and collateral circulation more than other methods.
In the light of all these results, multi-center studies are required to achieve longer-term evaluations and more permanent results.











 nueva página del texto (beta)
nueva página del texto (beta)