Introduction
Prostate cancer (PCa) is a major public health concern worldwide, and in 2018, 1,276,106 new cases were reported. Moreover, PCa is the second most commonly diagnosed cancer and the second cause of cancer-related death in Mexican men. In addition, PCa ranks among the top 10 causes of death in Mexico's general population, and the mortality rate expected for 2020 is 11.5 in every 100,00 men diagnosed with PCa1-4.
In developed countries, 80% of PCa cases are detected in early stages with a prostate-confined disease, whereas in Mexico, 80% are advanced-stage diseases when diagnosed, halting the chance for intent-to-cure treatments3,5.
PCa early detection (PCa-ED) in asymptomatic men through a digital rectal examination (DRE) and prostatic-specific antigen (PSA) proved a positive impact dropping mortality rates. Nevertheless, controversy remains around the related risk of overtreatment and overdiagnosis. PCLO trial failed to demonstrate a significant effect on long-term mortality in North American men. On the other hand, the European trial ERSPC found a long-term reduction of 21% in cancer-specific mortality rate, remarking the need to submit 781 men to PCa-ED to detect 27 cases and prevent one death6,7.
Although these trials' methodologies were different and not without biases, pooled data from both trials were reanalyzed by Tsodikov et al., concluding that in fact, PCa-ED drops cancer-specific mortality rate by 7-9%8.
Current American Urological Association (AUA) guidelines recommend providing patients with information about risk and benefits of PCa-ED to reach a shared decision. Nonetheless, Mexico lacks strong PCa-ED programs which could have an impact on stage at diagnosis and mortality rates9.
Primary care physicians (PCPs) have an important role in PCa-ED as they are the ones who mainly carry it and refer patients further to urology when needed. Current tendencies on PCa-ED among PCP in Mexico are to date unknown. Therefore, we consider that this could be a strategic target for improvement in PCa mortality rates in the long run. The objective of this cross-sectional study was to assess PCP knowledge and skills on PCa-ED trough a modified survey from Drummond et al.10.
Materials and Methods
Survey development
A self-administrating survey assessing knowledge and skills on PCa-ED for PCP previously developed by Drummond et al., was modified. Data on PCPs practice, skills, and knowledge regarding PCa-ED were included in the study. The survey was evaluated and analyzed by a panel of urologists for content discussing. Afterward, it was analyzed by an expert on surveys and questionnaires development and proper modification on wording and syntaxes were made, and a first draft was obtained, which was then delivered to five subjects and last modifications were made based feedback, reaching the final version (Supplementary material 1).
Survey administration and data collection
PCPs were approached in a scheduled session during a local family medicine annual meeting and invited to participate. Only PCPs who voluntarily accepted, with current public and/or private clinical activities within Southeast Mexico, were included. PCPs were categorized by academic degree as social service medical doctors, general practitioners, family medicine physicians, and family medicine residents. After a briefing about the survey and the scope of the study, questions and doubts were cleared and every PCP was provided with the printed self-administrating survey to fill in. Data were then emptied in a Microsoft Excel database.
Statistical analysis
A Kolmogorov-Smirnov normality test and descriptive statistics were conducted. Categorical data were compared by the c2 test. A logistic regression model was carried out to assess the propensity of PCP to test PSA in asymptomatic men for PCa-ED. All p < 0.05 values were considered statistically significant. Analysis was done using SPSS v. 21 software.
Results
A total of 170 PCP completed the survey. Median age was 33 (29-50) years and 58.2% were female. Regarding academic level, 51.8% were general practitioners, 14.7% family medicine physicians, 25.3% family medicine residents in training, and 8.2% social service medical doctors. Factors related to PCa-ED among PCP are summarized in table 1.
Table 1 Primary care physicians' characteristics and practice trends related to prostate cancer early detection
| n = 170 | n | % |
|---|---|---|
| Sex | ||
| Male | 71 | 41.8 |
| Female | 99 | 58.2 |
| Age | ||
| 33 (29-50) years | ||
| Academic degree | ||
| General practitioner | 88 | 51.8 |
| Family medicine physician | 25 | 14.7 |
| Family medicine resident | 43 | 25.3 |
| Social service medical doctor | 14 | 8.2 |
| Training finish year | ||
| 2009 (1993-2012) | ||
| 1977-2008 | 83 | 48.8 |
| 2009-2017 | 87 | 51.2 |
| PCa-ED† institutional program | ||
| Yes | 69 | 40.6 |
| No | 101 | 59.4 |
| Do you routinely practice PCa-ED†? | ||
| Yes | 95 | 56 |
| No | 75 | 44 |
| Self-perception of training in PCa-ED† | ||
| Well trained | 45 | 26.5 |
| More or less trained | 102 | 60 |
| Not well trained | 23 | 13.5 |
| Do you have access to PSA‡ testing at your institution? | ||
| Yes | 129 | 75.9 |
| No | 41 | 24.1 |
| DRE§ monthly performed for PCa-ED† | ||
| None | 104 | 61.2 |
| 1-5 | 60 | 35.3 |
| 6-10 | 5 | 3.0 |
| > 10 | 1 | 0.6 |
| Are you aware of national guidelines on PCa-ED†? | ||
| Yes | 122 | 71.8 |
| No | 48 | 28.2 |
Knowledge of the predictive value of PCa-ED tools
Mean score of risk factors knowledge was 51.5 ± 15.7%. A score above the mean was not associated with testing PSA on asymptomatic men (p = 0.674). Risk factors outcomes are summarized in table 2. The positive predictive value (PPV) of PSA + DRE was overestimated by 65.3% os respondents.
Table 2 Knowledge about prostate cancer risk factors among primary care physicians
| Risk factor | Correct n (%) | Does not affect risk n (%) | Reduces risk n (%) | Increases risk n (%) | I'm not sure n (%) |
|---|---|---|---|---|---|
| Older age (> 50 years) | 158 (92.9) | 4 (2.4) | 6 (3.5) | 158 (92.9) | 2 (1.2) |
| First-degree relative with PCa† | 157 (92.4) | 4 (2.4) | 6 (3.5) | 157 (92.4) | 3 (1.8) |
| Smoking | 11 (6.5) | 11 (6.5) | 7 (4.1) | 144 (84.7) | 8 (4.7) |
| High fat diet | 104 (61.2) | 26 (15.3) | 7 (4.1) | 104 (61.2) | 33 (19.5) |
| First-degree relative with breast cancer | 79 (46.5) | 49 (28.8) | 2 (1.2) | 79 (46.5) | 40 (23.5) |
| HPB‡ | 27 (15.9) | 27 (15.9) | 4 (2.4) | 132 (77.6) | 7 (4.1) |
| African-American race | 84 (49.4) | 10 (5.9) | 17 (10) | 84 (49.4) | 59 (34.7) |
†PCa: prostate cancer early detection;
‡BPH: benign prostatic hyperplasia
Institutional programs and skills on PCa-ED
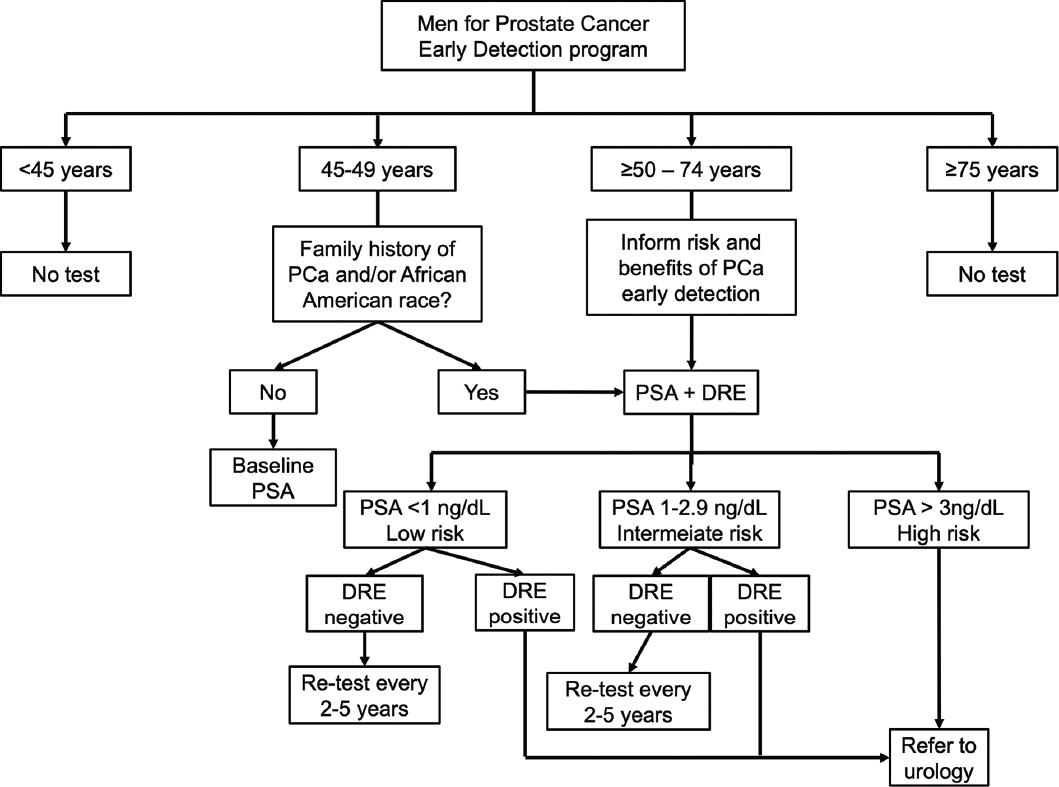
Having an institutional program for PCa-ED was answered by 40.6% of PCP. Moreover, 76% of PCPs have access to PSA testing in their work facilities/institution. Only 13.5% were self-perceived as "not well-trained" for PCa-ED. Furthermore, 56% reported carrying out PCa-ED routinely. Testing PSA on asymptomatic was considered as a proxy for PCa-ED and was found on 40% of PCP. The selected age ranges for PSA in asymptomatic men are presented in figure 1.
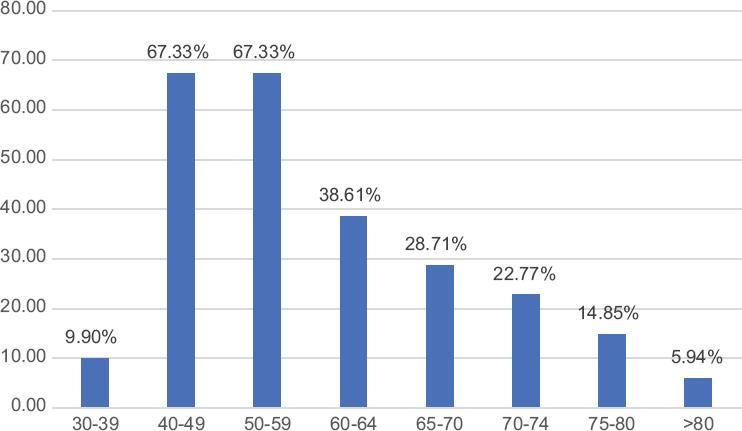
Figure 1 Age ranges chosen by primary care physicians for testing prostatic-specific antigen in asymptomatic men.
The 61.2% of PCP answered they do not carry out any DRE for PCa-ED. Moreover, 60.6% lacks proper physical space at their facilities, 44% lacks assistance, and 39.4% lacks time for DRE in daily practice. Nevertheless, these factors were not associated with weather or not carry out a DRE (p = 0.196, p = 0.122, and p = 0.108, respectively).
Factors related to testing PSA in asymptomatic men
Unadjusted logistic regression model found that fewer years in practice and being a family medicine resident were factor related with a less likelihood of testing PSA in asymptomatic men whereas having access to PSA testing and an institutional program on PCa-ED, increased the probability. However, the only factor significantly related in the multivariate model was having access to PSA testing at their work institution, as shown in table 3.
Table 3 Factors associated with the primary care physicians' propensity to test PSA in asymptomatic men
| Test PSA in asymptomatic men n (%) | OR‡ univariate (CI§ 95%) | p | OR‡multivariate (CI§ 95%) | p | |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 41/71 (57.7) | 0.88 (0.47-1.65) | 0.708 | 1.34 (0.67-2.68) | 0.404 |
| Female | 60/99 (60.6) | 1 | 1 | ||
| Training finish year | |||||
| 1977-2008 | 57/83 (86.7) | 1 | 1 | 0.63 (0.29-1.33) | 0.630 |
| 2009-2017 | 44/87 (50.6) | 0.46 (0.25-0.87) | 0.017* | ||
| PCa-ED institutional program | |||||
| No | 53/101 (52.5) | 1 | 0.027* | 1.54 (0.75-3.18) | 0.237 |
| Yes | 48/69 (69.6) | 2.07 (1.08-3.94) | |||
| Academic degree | |||||
| General practitioner | 56/88 (63.6) | 1.43 (0.77-2.66) | 0.245 | 1.13 (0.30-4.23) | 0.850 |
| Family medicine physician | 18/25 (72) | 1.9 (0.75-4.88) | 0.165 | 1.19 (0.23-6.03) | 0.825 |
| Family medicine resident | 19/43 (44.2) | 0.43 (0.21-0.87) | 0.019* | 0.64 (0.16-2.48) | 0.521 |
| Social service medical doctor | 8/14 (59.4) | 0.90 (0.29-2.72) | 0.857 | 1.55 (0.42-5.66) | 0.500 |
| Institutional access to PSA† testing | |||||
| Yes | 87/129 (67.4) | 3.95 (1.90-8-40) | 0.001* | 3.36 (1.54-7.30) | 0.002* |
| No | 14/41 (34.1) |
CI: coefficient intervals;
‡OR: odds ratio; PCa-ED: prostate cancer early detection;
†PSA: prostatic-specific antigen.
*p < 0.05
Discussion
This is the first work on PCa-ED trends among PCP in Mexico, where currently, PCa is overall the most common solid tumor in men. The role of PCa-ED is paramount on detecting significant PCa in early stages and it drops the mortality rate up to 21%2,7,8.
Findings related to PCa-ED skills and knowledge are notable, with a low frequency of PCP practicing PCa-ED and mostly using concepts which differ from scientific evidence. Despite this, solely, a small proportion were self-perceived as "not well-trained" (13.5%) (Table 1).
According to the AUA guidelines, PCa-ED is performed through PSA and DRE9. In this work, 56% of PCP answered carrying out PCa-ED, nonetheless, 61.2% do not perform a single DRE and over 95% perform < 5, monthly. Furthermore, 40% do not test PSA on asymptomatic men, and those who did, mostly selected age ranges outside the evidence-based recommended (Fig. 1). Likewise, Tasian et al. reported on 82 PCP from San Francisco that 86% carry out PCa-ED in < 60% of men over 50 years old. However, a survey about PCa-ED practice among PCP from the United Kingdom found that solely 24% had not tested PSA on asymptomatic men within the past 3 months. Drummond et al. reported a higher rate of PCa-ED practice on 1625 Irish PCP (79%), although the age ranges also differ from the evidence-based recommendations. These data evidence that the rate of PCP in Mexico performing PCa-ED is low and outside the suggested age ranges10-12.
On the other hand, PCP scored low in knowledge about PCa risk factors (51.5 ± 15.7%, table 2). Factors as older age and a first-degree relative with PCa were correctly identified by > 90%, nevertheless, smoking was wrongly identified as a risk factor by a higher rate (84.7%) than that reported elsewhere (29-56%). Although controversial, meta-analyses have failed to prove an association of smoking as a risk factor10,11,13. Likewise, prostatic hyperplasia was wrongly marked as a risk factor for PCa by 77.6%, whereas solely 28% of the Irish PCP did, even when evidence points otherwise10,14. African-American race was correctly identified as a risk factor by 49%, whereas Tasian et al. and Drummond et al. reported 98% and 17%, respectively. Furthermore, the rate of PCP self-perceived as "not well-trained" reported by Drummond et al., was more than twice than the herein reported (37% vs. 13.5%)10,11.
Data suggest a lack of continuing medical education on PCa, nevertheless, our findings, as well as those reported by Tasian et al., showed no association between risk factors knowledge and testing asymptomatic men11.
Based on these findings, it is important to improve PCPs training on PCa risk factors, as it might reverberate on better health promotion and PCa prevention, but training focused on clinical skills for PCa-ED is mandatory, since over 28% of PCP were not aware of national guidelines on PCa-ED.
Furthermore, these heterogenic data point that the PCa-ED conducted in Southeast Mexico is suboptimal and of lower rate compared to that reported elsewhere10,11. This can be partly explained by the high rate of PCP lacking an institutional program or a dedicated clinic to PCa-ED (59.4%) and by the fact of not having access to PSA testing by almost one quarter. Moreover, the rate of PCP who do not carry out DRE was quite high (> 60%) and nonetheless the institutional limitations may prevent them to conduct it such as lack of space, assistance, and time, these were not associated to whether or not performing a DRE (p > 0.05).
A PSA > 3.0 ng/dL holds ~ 25% risk of PCa and a PPV < 30% in the PCa-ED15,16. More than half of PCP overestimated the PPV of PSA and interestingly, despite the lower rate of DRE conducted, also the PPV of DRE and DRE + PSA was overestimated. Similar results were reported in Malaysia and Ireland, were > 50% overestimated PPV from tools used for PCa-ED. A deficient knowledge on this regard carries a risk of overdiagnosis10,17.
Factors related to preventing testing PSA on asymptomatic men on unadjusted model suggest a relation with experience, as PCPs who been in practice fewer time or still in training (family medicine residents) were less likely to perform PCa-ED (Table 3). This matches with other studies where longer time in practice (> 10 years) at least doubled the likelihood of testing PSA on asymptomatic men (odds ratio [OR]: 2.15, IC95% 1.11-4-16, p = 0.03), suggesting that engaging PCP on adequate continuing medical education programs focused on PCa-ED can improve PCa diagnosis. Family medicine residents are trainees, and this hypothetically should have increased the likelihood of testing, nevertheless, other factors as the lack of time due to busy schedules and a supervised decision-making by attendings could have impacted on these results, but furthers studies are needed10,17.
Multivariate analysis showed that having access to a PSA testing at least triples the likelihood of testing PSA in asymptomatic men (OR: 3.36, IC 95% 1.5-7.30, p = 0.002) (Table 3). This result is reasonable and advises that every PCP must have access to PSA testing in their institutions. Drummond et al. reported that PCP having institutional "men clinics" were more likely to test PSA on asymptomatic men. Hence, access to PSA testing and institutional guidance trough programs or dedicated clinics is a promising strategy for improving PCa-ED in Mexico. Therefore, for PCP currently lacking institutional guidance, a flowchart is provided for PCa-ED decision-making (Fig. 2), although further validating studies are needed, and educational intervention strategies trials are warranted10.
Regardless this work focus on the role of PCP, conducting programs of PCa-ED in Mexico go beyond in complexity. In addition, official regulation on PCa-ED is ambitious and yet controversial. A recent insight of PCa-ED in Mexico was published by Lajous et al., and it's suggested that following the official normativity is challenging as Mexico probably lack the wanted infrastructure and resources to bear the extra burden of around 15 million men undergoing PCa-ED18. Following the authors' statements, we consider that outlining a PCa-ED national effort requires not only the PCP topics addressed here but also a collective endeavor along health institutions to provide a wider overview and determine the settings needed for this challenging situation.
Some limitations are warned in this work: (I) Southeast Mexico has a high proportion of rural communities, which might not reflect the same situation of other regions; (II) related literature published arise from non-standardized surveys and questionnaires, hence, outcomes are not always uniform and exactly transposable, and (III) subjecting a patient to PCa-ED is a shared decision process which requests patients engagement on his own health, a variable which was not considered by this study.
Conclusions
PCa-ED drops the cancer-specific mortality rate and is mainly performed by PCP. The lack of access to PSA testing, institutional guidelines and programs dedicated to PCa-ED, added to a scarce knowledge of PCa and a presumably suboptimal continuing medical education programs in Southeast Mexico, turns out in a low rate of PCP performing PCa-ED and far from evidence-based recommendations. The development of a nationwide strategy for practice and training in PCa-ED tailored to PCP is mandatory for improving the CaP mortality rate and increases the likelihood of diagnosing patients with prostate-confined stages trough an informed and shared decision-making process.











 nueva página del texto (beta)
nueva página del texto (beta)