Introduction
Biliopleural fistula (BPF) is a pathological communication between the biliary tree and the pleural space. There are several causes described in the literature, which we can summarize in 5 groups1-3:
− Congenital
− Infectious (amebic liver abscess, pyogen, etc.)
− Bile duct obstruction (excluding iatrogenic or traumatic causes)
−Traumatic (blunt or penetrating)
− Iatrogenic (after liver resection, radiofrequency ablation, chest drainage, etc.)
Pathogenesis can be explained by two mechanisms3-5: in the first case, bile duct obstruction is the primary cause of BPF formation due to trauma, inflammation, tumors, etc. This obstruction leads to biliary retention, biloma, and an abscess that gradually erodes the diaphragm and creates communication to the pleural space. In the second case, there is no obstruction of the bile duct, but if the presence of a diaphragmatic/hepatic erosion, whether inflammatory, infectious, or traumatic that conditions biliopleural communication. In both cases, if there is a previous pulmonary condition that adheres the lung to the parietal pleura (old complicated parapneumonic effusion, empyema, etc.), there is a possibility that the path fistulizes to the bronchial tree and have a bronchobiliary fistula, a rare situation within the entity6. In any case, the preferred anatomical point for the formation of this communication is in the posteromedial region of the right hemidiaphragm, a site in contact with the naked area of the liver3,4,6,7.
BPF is a rare complication, so there is no epidemiological data on it. Among the most common causes reported in the literature were infectious causes such as liver abscess; however, in recent years, the traumatic cause (mainly penetrating) has been more frequent in the case and series reports (Table 1). In a reference trauma center such as our hospital, the traumatic cause is the most frequent, followed by infectious causes.
Table 1 Advance in the management of biliopleural fistulas
| Author | Year | No. of patients | Etiology | Type of fistula | Initial therapy | Second line of treatment | Results | Especial recommendations |
|---|---|---|---|---|---|---|---|---|
| Ferguson and Burford 20 | 1967 | 7 | Trauma (×4) Abscess (×2) Biliary obstruction (×1) |
BPF BBF |
Surgical | No recurrences | Summarize the basic steps for the Surgical treatment of BFP | |
| Saylam et al.4 | 1974 | 6 | Echinococcosis (×2) Abscess (×2) Desconocido (×2) |
BPF | Surgical | Mortality: 1 due to septic shock | It focuses on thoracotomy If a biliary obstruction is found, it must be resolved first |
|
| Boyd6 | 1977 | 16 | Biliary obstruction Iatrogenic |
BPF BBF |
Surgical | Not specified | Correction of biliary obstruction thoracic drainage are necessary | |
| Terris et al.21 | 1997 | 3 | Echinococcosis | BPF BBF |
Surgical | Reoperation in 1 patient | 1 death from pulmonary embolism | A case of left BBF is described |
| Oparah y Mandal22 | 1978 | 4 | Trauma (penetrating) | BPF | Surgical: thoracotomy +/- laparotomy with pleural catheter | No recurrence Patients with only a thoracic catheter had prolonged hospitalization |
The use of pleural drainage only with a probe is indicated only if drainage is performed early in combination with adequate subphrenic drainage. | |
| Wei et al.23 | 1982 | 2 | Biliary obstruction (stones) | BBF | Surgical: abdominal approach | No recurrence | ||
| Warren et al.8 | 1983 | 15 | Biliary obstruction iatrogenic (×10) Congenital (×1) Trauma (×2) Stones (×2) |
BPF (×13) BBF (×2) |
Surgical: abdominal approach Only 1 patient with lobectomy |
Reoperation in 9 patients | 63 surgical procedures in total They eventually recovered |
Suggest abdominal approach for biliary obstruction |
| Crnjac et al.2 | 1987 | 30 | Hydatid liver disease | BBF | Surgical: thoracotomy, laparotomy or both with pulmonary resection, cyst resection, diaphragmatic repair, and subphrenic drainage for 2-4 weeks | Reoperation in 2 patients | 3 patients died (10.3%) 2 patients with BBF recurrence |
Thoracotomy if pre-operative studies show irreversible lung involvement and a single cyst |
| Gugenheim et al.24 | 1988 | 16 | Biliary obstruction iatrogenic
(×8) Echinococcosis (×7) Amoebic abscess (×1) |
BBF | Surgical: abdominal approach | Reoperation | 42 surgeries in total They all recovered. |
Abdominal approach when BBF results from a biliary
condition Thoracic approach to traumatic BBF and assess pulmonary resection |
| Yilmaz et al.25 | 1996 | 11 | Complicated hydatid liver disease (×8) Biliary obstruction iatrogenic (1) Hydatid liver disease+ stones (×1) Amoebic abscess (×1) |
BBF | Conservative: nasobiliary drainage in 4
patients Biliary stent + nasobiliary drainage in 7 patients |
Conservative treatment is repeated in 3 cases. Prolonged stay in patients with biliary stent + nasobiliary drainage | Everyone resolved | First successful series in non-surgical BFF treatment |
| Sentuk et al.26 | 1998 | 3 | Alveolar-hydatid disease (×1) Hydatid liver disease (×2) |
BBF | Conservative: ERCP + sphincterotomy post-surgery (1
case) ERCP + nasobiliary drainage (2 cases) |
Conservative treatment is repeated: octreotide (1 case) biliary stent (2 cases) | Recurrence in all cases | The treatment of BBF due to hydatid liver disease is not satisfactory either by surgical or conservative treatment; the reason is the most invasive nature of the disease |
| Chua et al.27 | 2000 | 2 | Iatrogenic | BBF | Conservative: biliary drainage (1
case) Surgical: thoracotomy with pulmonary and fistula resection (second case) |
Surgical after the recurrence of the first case | Both patients recovered | Describes the use of vascularized intercostal pedicle and flat pericardial to close the fistula |
| Kabiri et al.28 | 2001 | 8 | Abscess: Amoebic (×3) Pyogen (×1) Trauma (×3) Iatrogenic (×1) |
BPF BBF |
Conservative: in 7 cases, sphincterotomy + pleural
drainage + octreotide Surgical: one case, repair of the biliary lesion |
Reoperation: 2 cases | Everyone improved | BFP is successfully treated with conservative
management Surgery is reserved for the failure of this management It is routinely used octreotide |
| Gerazounis et al.29 | 2002 | 3 | Echinococcosis | BBF | Surgical: right posterolateral thoracotomy | 2 patients died, the rest of the patients improved | Suggests surgery in complicated cases of echinococcosis in BBF | |
| Uchikov et al.9 | 2003 | 3 | Hydatid liver disease (×2) Echinococcosis (×1) |
BBF | Surgical: thoracotomy | Everyone improved | ||
| Ong et al.17 | 2004 | 2 | Biliary obstruction por stones (×1) Iatrogenic (×1) |
BBF | Conservative: ERCP + sphincterotomy + stent + octreotide | Surgical: only in 1 patient | 1 muerte por laceración de la vena cava inferior | Suggests the use of octreotide in conservative treatment |
| Peker et al.30 | 2007 | 4 | Hydatid liver disease | BBF | Surgical: 2 cases Conservative: 2 cases |
Everyone improved | Proposes a treatment algorithm for BFF | |
| Tocchi et al.31 | 2007 | 31 | Hydatid liver disease | BBF | Surgical: pulmonary resection was required in 25 cases | 3 patients murieron (9.6%) 26 patients se recuperaron |
It focuses on the thoracoabdominal approach | |
| Erygit et al.5 | 2007 | 3 | Abscess (×2) Penetrating trauma (×1) |
BFP | Surgical: thoracotomy and pulmonary resection in two cases | No recurrences reported | ||
| Aydin et al.32 | 2009 | 3 | Abscess (×1) Iatrogenic (×2) |
BBF | Conservative: percutaneous drainage with endoscopic sphincterotomy + stent | No recurrences reported | Suggest conservative treatment Fistula embolization is described for the 1st time |
|
| Gandhi et al.33 | 2009 | 1 | Trauma (blunt) | BPF | Conservative: ERCP + sphincterotomy + stent | Thoracotomy | Recurrence that needed surgery | Complete resolution |
| Ball et al.34 | 2009 | 1 | Trauma (penetrating) | BFP | Conservative: ERCP + sphincterotomy | Complete resolution | ||
| Mehrzard et al.35 | 2012 | 1 | Trauma (blunt) | BPF | Conservative: ERCP + sphincterotomy | Late thoracotomy (1 year later) | Recurrence after 1 year | Thoracotomy was required after 1 year after the fistula was resolved |
| Liao et al.16 | 2012 | 1 | Trauma (blunt) | BPF | Conservative: ERCP | Full resolution |
BPF: bilopleural fistula; BBF: biliobronchial fistula; ERCP: endoscopic retrograde cholangiopancreatography.
The clinical manifestations are described as acute or chronic: the acute event the patient begins with respiratory stress, febrile syndrome, pleuritic pain in the lower portion of the right hemithorax, irritative cough, yellowish sputum in cases of BBPF, and right pleural effusion. The chronic condition is characterized by chronic cough, occasional yellow sputum, intermittent fever, and pneumonia-like conditions8,9.
In recent years, conservative treatment has become more important in the treatment and the advent of endoscopic pancreatic cholangiography (endoscopic retrograde cholangiopancreatography [ERCP]) has resulted as an effective element in the treatment of BPF despite the few case series that exist in the literature10,11, which is why there are no guidelines for optimal treatment. In this paper, we present the experience of the use of ERCP in patients with BPF treated in our Hospital Universitario "Dr. José Eleuterio González" in the last 3 years.
Materials and methods
A descriptive retrospective study was carried out, including patients who were detected the presence of fructose bis-phosphate (FBP) for various causes, including penetrating wounds. We obtained the information of clinical records, diagnoses were assessed, characteristics of the lesions, initial repair technique, days of hospital stay, and their outcome after performing all of our ERCP patients. We made a statistical analysis with the JMP 10 program. These patients were in a period from August 2016 to August 2019 in our Hospital Universitario "Dr. José Eleuterio González" in Monterrey, N.L., Mexico.
Results
We obtained a total of 8 patients with a diagnosis of FBP in a period of 3 years, of which 6 were men (75%) and 2 women (25%), with a mean age of 24.5 years. The diagnoses were three in all, traumatic, which we divided into gunshot wound (GSW) and stab wounds and infectious (Fig. 1).
Our 7 trauma diagnosis patients showed a double penetrating lesion, either by a projectile or by a knife, which required a surgical approach; all of them underwent an exploratory laparotomy and only 2 of the 7 trauma patients a concomitant right thoracotomy was required due to the initial trauma, either for the repair of pulmonary lesions or control of chest bleeding. Due to the double penetrating lesion, there was a need for diaphragmatic repair, which debrided the edges in the firearm injuries and performed primary repair of the diaphragm; in one patient, an omentum patch was performed and in the second trauma patient was placed a pleura patch (Table 2). The eighth patient was a female with a diagnosis of pyogenic liver abscess who had her laparotomy abscess drained with an omentum patch placed on the liver bed.
Table 2 Population with their initial diagnoses, initial surgery, and type of diaphragmatic repair
| Patient | Diagnosis | Injuries | Surgery | Repair |
|---|---|---|---|---|
| 1 | GSW | Liver injury SII + Intestinal injury SIII + intercostal laceration | Laparotomy + Right thoracotomy | Primary + pleural patch |
| 2 | GSW | Liver injury SIII | Laparotomy | Primary |
| 3 | GSW | Liver injury SII | Laparotomy | Primary + omentum patch |
| 4 | SW | Liver injury SII | Laparotomy | Primary |
| 5 | GSW | Liver injury SIII + colon lesion SII + Intercostal artery laceration | Laparotomy + Right thoracotomy | Primary |
| 6 | GSW | Liver injury SII+ lung laceration | Laparotomy + Right thoracotomy | Primary |
| 7 | SW | Liver injury SIII | Laparotomy | Primary |
| 8 | Pyogenic liver abscess | Does not apply | Laparotomy | Primary + omentum patch* |
Firearm projectile wound (GSW), puncture wound (SW), injury stage (S).
*This patient underwent surgical drainage of the liver abscess and the omentum patch was placed on the liver bed; GSW: gunshot wound, SW: stab wound.
All our patients had a need for the placement of a pleural catheter (PC) from the beginning due to the double penetrating lesion. The outflow of liquid with biliary characteristics was observed by the PC between days 3 and 14 post-placement (mean of 5.7 days); the fistulas recorded an expense of approximately 100 cc of biliary characteristics in 24 h. No other imaging study was performed for diagnosis due to the obvious clinical signs of patients with the presence of right pleural effusion and the characteristics of the fluid drained by the PC. Clinically, patients diagnosed with BPF due to trauma remained hemodynamically stable, with no evidence of systemic inflammatory response; the patient with a diagnosis of liver abscess was detected the presence of BPF at 14 days post-PC placement, remained persistent febrile due to an intra-abdominal collection secondary to her diagnosis, which was evacuated by punction; however, the patient was complicated with intrahospital pneumonia which culminated in her death.
All of our patients underwent ERCP with sphincterotomy between days 2 and 10 after diagnosis of BPF (mean of 4.3 days). Once the procedure was performed, we obtained the resolution of the BPF in 7 of 8 patients (87.5%). We define as a response to treatment the decrease in the biliary expenditure by the thoracic catheter to < 10 cc in 24 h with radiological evidence of little or no residue in the pleural cavity, which was obtained from these 7 patients between days 3 and 5 post-ERCP (average of 3.12 days). No complications of ERCP were reported.
We had mortality in 2 patients which are worth analyzing in detail: the first patient who died was a GSW in which, in his associated lesions, a colon lesion was detected; in his post-operative, the patient was complicated with the presence of BPF which was detected on the 5th day after PC placement, ERCP was performed on the 10th day (ERCP delayed due to poor patient conditions) and we obtained a response to appropriate BPF treatment on the 5th day after ERCP; however, the patient's conditions did not improve and finally the patient dies from sepsis. The second case was a patient with a diagnosis of pyogenic liver abscess who was referred to our hospital with PC and for follow-up. We detect the presence of BPF on the 14th day after PC; late ERCP is performed due to poor conditions of the patient (on the 6th day after diagnosis); however, due to abdominal sepsis knotted to a diagnosis of hospital-acquired pneumonia, the patient passes away.
At present, at long-term follow-up, the 6 patients in whom we obtained a good response to ERCP treatment remained uncomplicated, these patients had PC withdrawn, major surgery was avoided, and no inflammatory response data were discharged for follow-up at the office. During his surveillance, there was no evidence of a recurrence of pleural effusion, an increase in bilirubin, or leukocytosis, so they were definitively discharged from the consultation.
Discussion
The presence of BPF is a low-frequency entity, as we saw reported in the literature, the infectious cause was the first cause described; however, in the most recent reviews, the penetrating traumatic cause is the one that currently prevails, probably due to the change in society and the current problems that we face and that we could verify in our study5,12-16. Its treatment begins from the early diagnosis, preventing the increase and complications of the BPF itself because the bile fluid it has a corrosive potential on the lung and pleura11,13. That is why a high degree of clinical suspicion is mandatory in its management.
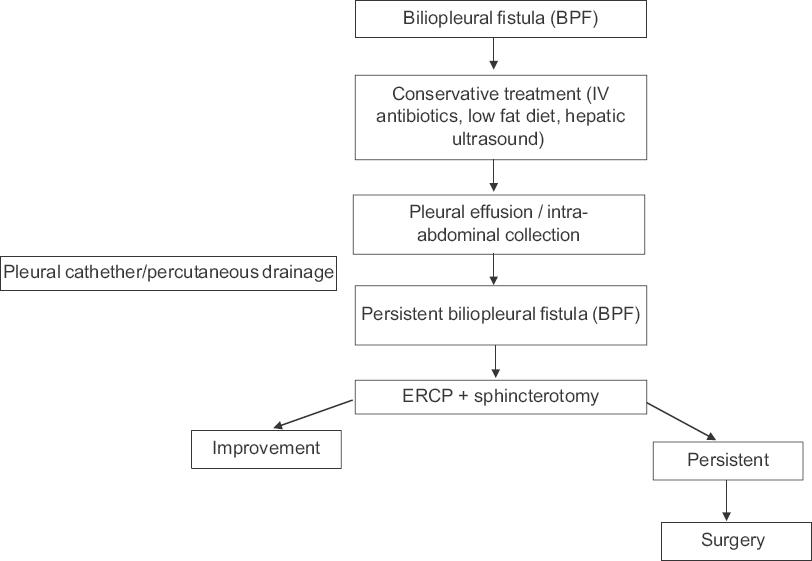
Due to the analysis of the experience obtained in our study and compared to that described in the international literature, we propose standardization in the treatment of BPF. Once the presence of BPF has been demonstrated, it is proposed to start with conservative management, which consists of the use of intravenous antibiotics, low-fat diet, analyze the use of somatostatin17, and liver ultrasound with right pleural space screening in which it can be identified pleural effusion and/or the presence of right subdiaphragmatic collection, so the PC is placed for pleural effusion and/or percutaneous drainage for intra-abdominal collections. The persistence of bile fluid by the PC dictates the need to assess the use of ERCP. This procedure is beneficial due to its potential diagnosis when performing an endoscopic and subsequently therapeutic cholangiography; considering the principle of any fistula, ERCP with sphincterotomy will reduce the distal resistance of the sphincter of Oddi which is around 18 ± 2 mmHg, in addition to the normal pressure of the common duct which is between 10 ± 2 mmHg, this pressure gradient will be reduced to 1 ± 1 mmHg after a spherotomy18. Due to this principle, ERCP with sphincterotomy is recommended within 72-96 h after PC placement and persistence of bile fluid outflow. It is expected to have BPF resolution within the first 48 h11. This conservative management does not increase the morbidity that surgical treatment entails. The pharmacological agents that reduce the pressure of the sphincter of Oddi have been proposed; however, their role in the management of BPF is unclear19. The percentage of success reported in the literature is close to 97% of cases, and the rest of patients culminate in the need for surgical treatment. That is why a BPF management algorithm is proposed (Fig. 2). In studies published in the literature, it does not dictate a difference between results according to cause (infectious vs. traumatic); in this series of cases, we found traumatic as the most frequent cause; however, we obtained an infectious cause in which he died of sepsis. It is important to note that the infectious origin of this entity is much more infrequent, that is why infectious versus traumatic analysis is difficult.
Conclusion
This study tries to be an initiator in the treatment of a very infrequent complication; its rarity is reflected in the few patients that were obtained in 3 years in a reference center in our country; however, good results were obtained with this observational study. This management algorithm is proposed to carry out prospective studies once this entity that is little described has been identified.
The importance of the benefit of biliary decompression in BPF is important, showing that it significantly reduces the morbidity and mortality offered by surgical treatment. The recommended time to perform it is 72-96 h after diagnosis of BPF when the patient's clinical conditions allow it; in this way, it has found the benefits of avoiding surgical treatment (intra-hospital days, costs, etc.).
Our series is the largest reported in the literature in recent years, which was treated with conservative management based on ERCP and sphincterotomy for BPF, obtaining promising results and promoting the use of this management algorithm in our center and serving as a basis for long-term prospective comparative studies.











 nueva página del texto (beta)
nueva página del texto (beta)