Introduction
Gastrointestinal (GI) schwannomas origin from Schwann cells sheath of the Auerbach´s plexus1. They are classified as mesenchymal tumors such as leiomyomas, GI stromal tumors (GIST), lipomas, and hemangiomas2.
Schwannomas represent 2-6% of GI mesenchymal tumors3. The most common localization is the stomach, followed by the colon and the rectum4.
Gastric schwannomas are almost always detected as a subepithelial mass like other mesenchymal tumors of the stomach5. Although they have a similar presentation, they have different behavior, therapeutic options, and prognoses. What makes each mesenchymal tumor different are the specific histology and immunohistochemical markers.
Clinical cases
The first case is a 66-year-old female with obesity, type 2 diabetes, hypertension, and atrial fibrillation. She was admitted to the hospital for dysphagia of 6 months of evolution. The patient reports progressive worsening, with intolerance to solid food. Within the diagnostic study, an ultrasound of the abdomen was performed, showing a solid lesion in the wall of the gastric antrum. In view of this finding, a high-resolution gastroscopy was performed. The examination showed a 5 cm hiatal hernia and an elevated 20 mm lesion in the major curvature covered with normal mucosa, suggestive of extrinsic compression (Fig. 1). Endoscopic ultrasound showed a hypo-echoic and heterogeneous 26 mm lesion suggestive of GIST in the gastric body. This lesion was in the 4th layer, the muscularis propia (Fig. 2). The abdominal computed tomography (CT) evidenced a 3cm exophytic mass in the antrum (Fig. 3). With the suspicion of a gastric GIST, a laparoscopic resection of the mass was performed. During the same procedure, assuming that the hiatal hernia could be the cause of the dysphagia, a hiatoplasty with mesh and a Nissen-type fundoplication was performed. The piece showed an intraluminal tumor of 3 × 2.5 cm with an elastic consistency and a lobed surface that respects the mucosa and retracts the serosa. Under the microscope, a neoplastic mesenchymal proliferation was observed, centered on the muscular layer, respecting the mucosa, submucosal, and serosa. It was constituted by spindle cells arranged in fascicles with collagen stroma and without necrosis. No mitosis figures were observed. The immunohistochemical study presented a tumor with positive staining to S-100 and negative to CD34, CD 117, actin, and desmin, a typical immunohistochemistry of schwannoma (Fig. 4). After 18 months of follow-up, the patient showed no signs of tumor recurrence in the complementary control tests. In addition, dysphagia disappeared after surgery.

Figure 1 Gastroscopy of the first case where a 2 cm elevated lesion with respected mucosa is observed.

Figure 2 Endoscopic ultrasound of the first case showing a 26 mm lesion, hypoecogenic and dependent on the 4th layer.

Figure 4 Immunohistochemistry of the first patient’s tumor. A: wavy splindled cells separated by woven fibrotic bundles. (H-E 10x). B: gastric schwannoma shows spindle cel tumors (H-E 10x). C: the tumors cells are spindle shapped with elongated nuclei and form loose interlacing fascicles or whorls (H-E 40x). D: intense expression of S-100 immunostain in tumor cells.
The second case is about a 64-year-old male who was followed for 9 years for a subepithelial gastric mass. He was diagnosed with an magnetic resonance imaging (MRI) performed on suspicion of choledocholithiasis. Initially, the lesion, located in the minor curvature of the gastric body, was 15 mm in diameter. In subsequent controls, it increased in size. In the last CT scan, the size was 30 mm. The high-resolution endoscopy showed an oval lesion of about 4 cm in the anterior face of the gastric body covered with normal mucosa (Fig. 5). Endoscopic ultrasound showed a slightly heterogeneous and hypoechoic lesion of 2.5 × 1.5 cm in diameter in the upper gastric body. The study showed that the lesion was located in the 4th layer (Fig. 6). In view of the progressive growth, it was decided to perform a laparoscopic resection of the tumor. The anatomopathological study showed a 2 × 2.5 cm intramural node that respects the mucosa and serosa. Microscopically, it was a neoplastic fusocellular proliferation centered in the muscular layer with collagen stroma and without necrosis. The cells presented a poorly defined eosinophilic cytoplasm, nuclear atypia, and low mitotic index (1 mitosis per 50 high magnification fields). Immunohistochemistry showed intense positivity to S-100 and negativity to CD34, CD117, actin, and desmin (Fig. 7). After 2 years of follow-up, there is no evidence of recurrence after a gastroscopy and a CT scan of the abdomen.

Figure 6 Endoscopic ultrasound of the second case showing a slightly heterogeneous and hypoechoic lesion of 2.5 x 1.5 cm located in the 4th layer.
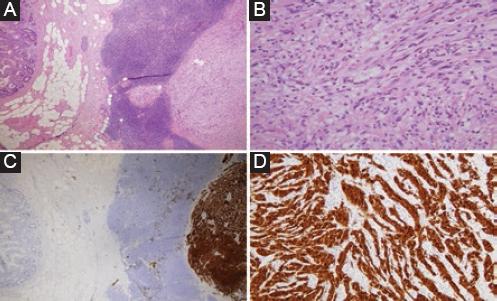
Figure 7 Immunohistochemistry of the second case tumor. A: gastric wall with intramuscular lesion, with prominent reactive lymphoid infiltrate in the periphery (H-E 4x). B: fusiform cells without cytologic atypia and significant mitosis (H-E 40x). C and D: intense expression of S-100 immunostain in tumor cells.
Discussion
Gastric subepithelial tumors are found in approximately 1 in 300 gastroscopies performed on adults. They occur as protrusions on the inner surface of the gastric lumen covered by normal epithelium. These lesions may be caused by a tumor in the gastric wall or by extrinsic compression6.
These tumors are classified as non-neoplastic and neoplastic. The non-neoplastic ones include inflammatory lesions, cysts, and ectopic pancreas. The most important neoplastic lesions are mesenchymal tumors and lymphomas. Mesenchymal tumors mainly include GIST, myogenic tumors such as leiomyomas and leiomyosarcomas, neurogenic tumors including schwannoma and neurofibroma and vascular tumors7.
In this paper, we present two cases of schwannomas. These tumors originate from the Schwann cells of the nerve sheaths. They are rare in the GI tract and their most frequent location is the stomach followed by the rectum. Their clinical presentation is variable, but most are asymptomatic, and their diagnosis is casual. The symptoms, when present, are usually due to their complications (digestive bleeding, compression, obstructive symptoms due to abdominal mass, and invagination)8. In endoscopy, they present as subepithelial elevated lesions with a firm consistency. Endoscopic ultrasound usually shows a hypoecogenic lesion originating from the 4th layer (muscle layer)9. Contrast-enhanced CT shows homogeneous attenuation with minimal increase in the arterial phase and delayed increase in the equilibrium phase7.
Due to its frequency and potential for malignancy, the main differential diagnoses of gastric schwannomas are GISTs. Their most frequent location is the stomach. The most frequent symptoms are bleeding and abdominal discomfort due to the mass effect. Some studies show that between 15 and 30% are asymptomatic10. The endoscopic features of GISTs are common to all other gastric subepithelial tumors, a smooth bulge covered by normal mucosa. When these tumors grow, they may show mucosal ulceration. Endoscopic ultrasound usually shows a hypo-choic or anechoic and slightly heterogeneous tumor. Hyperecogenicity can be a sign of malignancy. The tumor usually depends on the 3rd or 4th layer and rarely on the 2nd layer. CT images vary according to size and aggressiveness. Small and benign lesions are usually well-defined, homogeneous with variable contrast enhancement. Large and aggressive tumors may be lobulated, with irregular margins, mucosal ulceration, central necrosis, and heterogeneous contrast enhancement7.
There are methods for sampling these tumors to make a histological diagnosis based on endoscopy or endoscopic ultrasound11. However, if the suspected diagnosis is a GIST, due to the risk of bleeding, we do not perform these kinds of tests in our hospital. Therefore, we apply the following protocol (Fig. 8): first, an endoscopy is performed to exclude epithelial lesions. Then, an endoscopic ultrasound confirms that the lesion is subepithelial. If the lesion is < 2 cm and shows no suspicious signs, only follow-up is performed. If it is larger than 2 cm or has any suspicious features, the next step is to perform a CT scan or MRI to better characterize the lesion and its possible dissemination. If, after these studies, the suspected lesion is GIST or another lesion suggestive of malignancy, the lesion will be surgically removed if there is no contraindication for it.
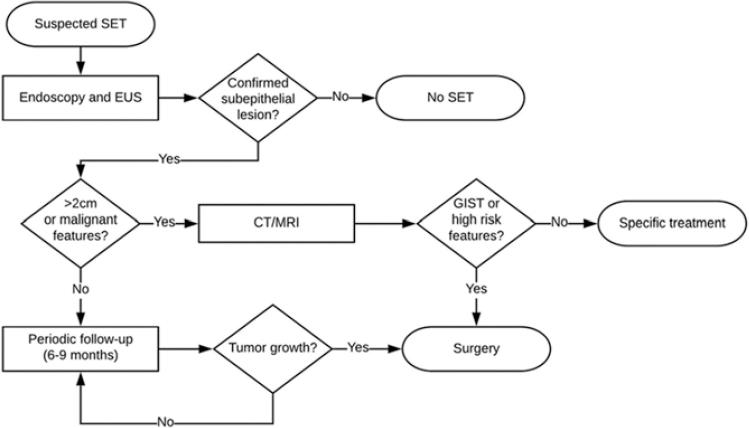
Figure 8 Protocol for the management of asymptomatic subepithelial gastric tumors in our institution.
This protocol applies to casually diagnosed subepithelial tumors. If the tumor produces symptoms, and there is no contraindication, treatment would be surgical. The therapeutic algorithm is based on the National Comprehensive Cancer Network guidelines which indicate that tumors suspected of GIST larger than 2 cm or those with high-risk characteristics are more likely to behave malignantly, and therefore, treatment should be surgical. If the suspicion is clearly of another type of lesion, the taking of samples for diagnosis could be considered, and the corresponding treatment applied.
This therapeutic management implies that the differential diagnosis of these tumors is generally done post-operatively in our institution. This diagnosis is based on the immunohistochemical examination of the surgical pieces. Schwannomas are positive for S-100 and negative for CD117, CD34, SMA, and desmin. Performing this diagnosis properly is very important because, in contrast to GIST, they are tumors with a very low malignant potential and resection with margins is practically curative.
Conclusion
Pre-operative differential diagnosis of gastric subepithelial lesions is complex. Endoscopy and endoscopic ultrasonography are often non-specific and are unable to differentiate practically benign lesions such as schwannomas from potentially malignant lesions like GIST. In our center, the therapeutic management is not based on a histological diagnosis due to the risk of bleeding from GIST after a puncture and is based on imaging characteristics and size. Therefore, the definitive diagnosis is made after the immunohistochemical analysis of the piece. This diagnosis is very important because resection with margins is practically curative in the case of schwannomas.











 nueva página del texto (beta)
nueva página del texto (beta)




