Introduction
Colorectal cancer is one of the most frequent cancers and the second in mortality1. Approximately 20% of patients with colon cancer will present metastases at diagnosis and up to 50% will develop them during the course of the disease, with the liver, lung, and peritoneal being the most common2,3.
Metastases in the thyroid gland are unusual. They appear in 1.4-3% of patients whose initial suspicion was thyroid carcinoma4. However, studies of autopsies of subjects with disseminated neoplasms have found between 2 and 24% of metastases on this gland5,6. The origin of the primary tumor is usually the lung, kidney, or breast depending on the series7-9. Metastases of colorectal cancer on the thyroid are extremely rare and are usually diagnosed after several years of follow-up4.
Clinical case
We present the case of an 85-year-old female patient who underwent a right hemicolectomy in 2004 for a T3N0M0 cecum adenocarcinoma and who presented pulmonary metastases of the tumor up to 3 times during the following 5 years, requiring segmental resections and adjuvant treatment with oxaliplatin and capecitabine. Subsequent follow-up was carried out without incident until 14 years later when an elevation of the carcinoembryonic antigen was detected in an analytical control. At this time, the patient had begun to develop dysphonia and dysphagia. A positron emission tomography-computed tomography (PET-CT) was performed (Fig. 1), evidencing pathological uptake at the thyroid level and the study was completed with an ultrasound-guided fine-needle aspiration, observing a 3 cm nodule with irregular edges being biopsied with a cytopathological diagnosis of Bethesda VI, compatible with large bowel metastasis. The immunohistochemical study showed positivity for CDX2 and CK20 and negativity for CK7.

Figure 1 Positron emission tomography-computed tomography showing the pathological uptake in the thyroid gland.
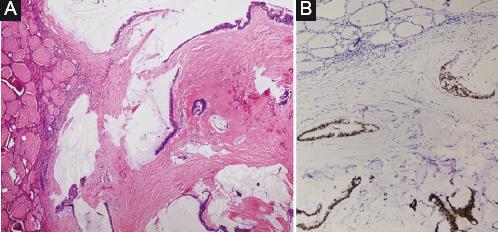
Surgical treatment was carried out, evidencing important infiltration of pre-thyroid muscles, trachea, and cricoid cartilage by the tumor located in the right thyroid lobe. Due to this, it was decided to perform the right hemithyroidectomy to alleviate the patient’s symptoms. The patient went through the post-operative period without incident and was discharged with good progress. The definitive pathological anatomy confirmed that it was a metastasis from adenocarcinoma of intestinal origin with positive staining for CDX2 and CK20 (Fig. 2).
Discussion
The first reference in literature of a metastasis in the thyroid gland is attributed to Virchow, who described a metastasis of a testicular tumor in 1871. Despite being a highly vascularized organ, the incidence of metastasis to the thyroid is low. The causes of this phenomenon are not clearly defined, but classically, the speed of blood flow and the high concentration of iodine and oxygen in the thyroid parenchyma are proposed7. In fact, thyroid disorders that reduce blood supply or iodine levels such as Hashimoto’s thyroiditis have been proposed as risk factors for thyroid metastases10.
The series with the highest number of cases of thyroid metastases from colorectal cancer show a similar proportion of involvement in men and women. The most frequent location of the primary tumor is the left colon or rectum and most patients present or have presented other distant metastases being the most frequent pulmonary metastases.
In some cases, this pattern of dissemination of the disease is not associated with liver metastasis, a fact that can be explained by hematogenous extension through the vertebral venous system avoiding the portal system11. This system was described by Breschet, in 1919, and is a venous plexus lacking valves, which connects the pelvis with the systemic circulation and the central nervous system. In 1940, Batson gave it clinical significance by relating it to the bone spread of prostate cancer.
The clinical presentation is variable. Many patients are asymptomatic and the diagnosis is obtained during the follow-up. If there are symptoms, a palpable cervical mass is the most frequent and may be associated with dysphagia, dysphonia, or dyspnea as in the case of our patient12.
The elevation of tumor markers can be an early diagnostic sign. Imaging tests such as CT, ultrasound, or PET scan may be useful, but fine-needle aspiration is the test of choice to differentiate a primary thyroid nodule from a metastasis6. Immunohistochemistry of primary thyroid tumors is positive for CK7 and negative for CK20, while in metastases of colorectal origin, like our patient, it is positive for CK20 and negative for CK7.
Treatment options are not clearly defined. There is not enough evidence on the extent of surgical resection. In bilateral disease, total thyroidectomy is recommended. If the disease affects only one of the lobes, most authors recommend lobectomy to minimize the risk of recurrent laryngeal nerve or parathyroid injury6; however, others defend total thyroidectomy based on the high probability of multicentric disease13. Local resection would be indicated in those patients, in whom only symptomatic palliation can be offered.
Lymph node involvement is rare, so prophylactic lymphadenectomy is not recommended6. The penetration of chemotherapy is low in the thyroid gland; however, recent studies show benefit when combining different agents. Finally, the role of radiotherapy is mainly the palliative treatment of symptoms in patients with unresectable disease or who would not support surgery14.
The prognosis of these patients is generally unfavorable. Survival is determined by the degree of malignancy of the primary tumor and by the presence or absence of metastasis in other locations. Surgical treatment with R0 resection of thyroid disease seems to be able to increase survival if there are no other metastases11.
Conclusion
The metastasis of colorectal adenocarcinoma in the thyroid gland is a rare entity, but it should be part of our differential diagnosis in patients with new appearance thyroid nodule with a previous oncological history. Although there is no established standard treatment, surgical resection has proven to be a valid option for the management of this disease, either with curative intent or for the palliation of local symptoms.











 nova página do texto(beta)
nova página do texto(beta)