Introduction
Anterior cervical spine surgery (ACSS) is a commonly indicated procedure to solve a variety of cervical spine pathologies (vertebral body fractures, tumors, and degenerative disk disease)1,2, at present, there exist a wide spectrum of surgical techniques able to be done through an anterior approach, whose main target is to provide neurological decompression of the neural axis, correct deformity, and preserve or attain mechanical stability3. Current series report good to excellent results on pain and neurological deficit improvement with high patient satisfaction scores4 irrespective of the chosen surgical technique, never the less, early in the post-operative period, and even in the long-term follow-up, a number of patients suffer from dysphagia, because significant retraction may be exerted on the esophagus during the surgical procedure or related to adverse outcomes from surgery such as post-operative hematoma, recurrent laryngeal nerve palsy, esophageal injury, post-operative adhesions, and device migration1,3,5. Dysphagia, being a well-known complication of ACSS5,6, can interfere with daily and social life, affecting prognosis adversely because of dehydration, malnutrition, or ineffective protection of airway from aspiration, ultimately becoming a life-threatening condition in severe cases1,2,7.
Dysphagia is defined erratically as a subjective increase in the time or effort required to move food from mouth to the stomach or more practically as difficulty in swallowing solids and liquids, and as a matter of inconsistency in diagnostic criteria across the scientific literature, its ranges vary widely from 1% to 80%1,5,8. In prospective studies, rates of dysphagia 1-month postoperatively are reported to be as high as 50%, which might decrease progressively overtime to 10-12.5% at 1 year9-11. Risk factors to the development of dysphagia include female gender, age over 60 years, smoking, preexisting swallowing dysfunction, C4-C5 and C5-C6 involvement, and multilevel surgery9,12,13.
Most anterior cervical surgery trials are focused in outcomes related to fusion rates and pain relief as well as neurologic deficit recovery, but few researches have been undertaken to determine dysphagia rates consistently as well as in the measures to prevent its post-operative incidence9. There is some evidence about steroids use, graft type, low profile plates, and surgical approach regarding dysphagia rates with no guidelines established up to date3,8,14-20. In this paper, we sought to describe our experience with a minimally invasive tubular approach for the anterior cervical procedures such as anterior cervical discectomy and fusion (ACDF) and total disc replacement (TDR) (arthroplasty), with the aim to compare our rates of dysphagia with those of available literature.
Materials and methods
The present work represents a retrospective observational cohort study with historical cohort comparison. We review the clinical files of patients undertaking a minimally invasive tubular approach to the anterior cervical spine to perform an ACDF or arthroplasty from 2013 to 2017. We collected data from clinical files and divided them by type of surgery, we then review variables such as sex, age, body mass index (BMI), surgical procedure, surgical time, bleeding, number of operated levels, radicular and neck pain visual analog scale (VAS), dysphagia VAS at post-operative day 1, 1 month, and end of follow-up. We processed data with SSPS 22 software, performing demographic statistical analysis and comparing incidence rates of radicular and neck pain VAS, dysphagia VAS from pre-operative to 1st-day post-operative, 1 month, and end of follow-up. We then compared dysphagia rates for the type of surgical procedure.
Results
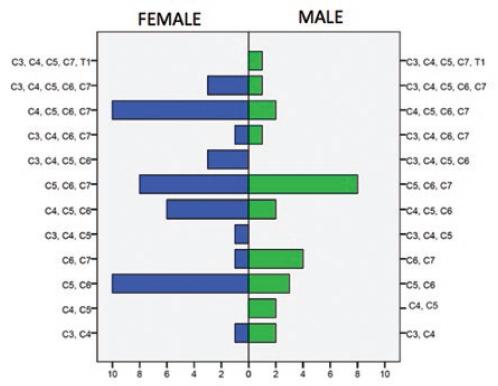
We collected 81 patients operated by a minimally invasive approach from 2013 to 2017 by the senior author (JASS), 70 patients underwent surgery for ACDF (44 females and 26 males) and 11 patients (8 females and three males) or arthroplasty.
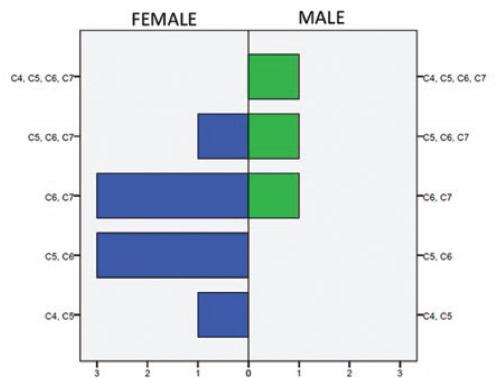
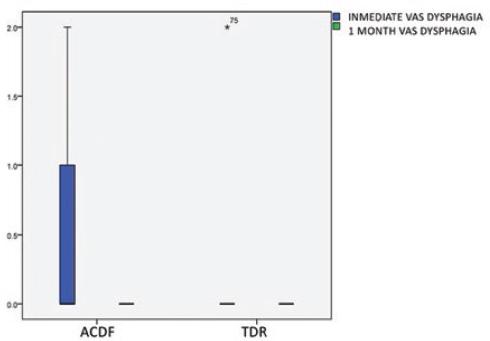
Mean age in ACDF group was 52.5 years (11.9 standard deviation [SD]), mean BMI was 24.8 (3.7 SD), mean operated levels per patient were 2.01 (0.8 SD), mean surgical time was 156.8 min (SD 67.2), and mean surgical bleeding was 39.07 ml (SD 31.03). When analyzed by the number of levels, surgical time resulted to be 55.5 min (20.0 SD) per level, and bleeding was 23.23 ml per level (22.5 SD). Mean pre-operative radicular pain VAS was reported to be 6.77 (1.2 SD) as compared to 1.35 (1.1 SD) mean VAS at the end of follow-up (p < 0.01). Mean pre-operative neck pain was reported to be 4.16 (2.7 SD) as compared to 0.67 (0.9 SD) mean VAS at the end of follow-up (p < 0.01). Mean post-operative VAS dysphagia on day 1 post-operative was 0.27 (0.4 SD) with a minimum of 0 and a maximum of 2, and no dysphagia was encountered at 1-month post-operative (p < 0.01). The mean follow-up period was 32.7 months (13.0 SD) with a minimum of 9 months and a maximum of 60 months. Figure 1 shows patients distribution by operated level. Figure 2 demonstrates immediate day 1 post-operative VAS dysphagia distribution (0 means no dysphagia). Figure 3 shows significant changes (p < 0.01) in mean dysphagia rates at day 1 post-operative and 1-month follow-up.
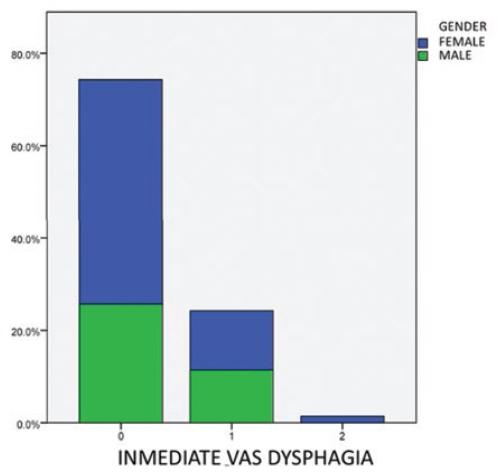
Figure 2 Immediate day 1 post-operative visual analog scale dysphagia distribution (0 means no dysphagia).
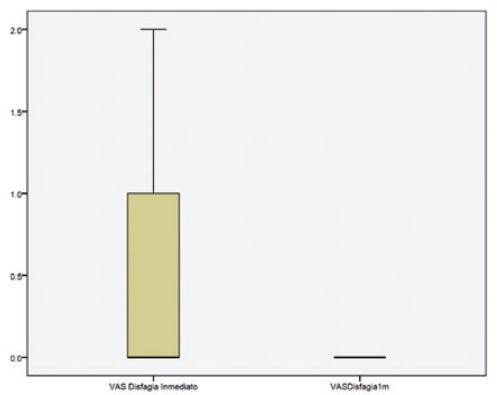
Figure 3 Significant changes (p < 0.01) in mean dysphagia rates at day 1 post-operative and 1-month follow-up.
Mean age in arthroplasty group was 42.7 years (13.0 SD), mean BMI was 24.44 (3.0 SD), mean operated levels per patient were 1.36 (0.6 SD), mean surgical time was 125.45 min (SD 34.7), and mean surgical bleeding was 30.64 ml (SD 14.5). When analyzed by the number of levels, surgical time resulted to be 54.77 min per level (16.0 SD), and bleeding was 23.74 ml per level (9.2). Mean pre-operative radicular pain VAS was reported to be 7.0 (1.1 SD) as compared to 0.64 (0.8 SD) mean VAS at the end of follow-up (p < 0.01). Mean pre-operative neck pain was reported to be 3.09 (2.5 SD) as compared to 0.64 (0.8 SD) mean VAS at the end of follow-up (p < 0.01). Mean post-operative VAS dysphagia on day 1 post-operative was 0.18 (0.6 SD) with a minimum of 0 and a maximum of 2, and no dysphagia was encountered at 1-month post-operative with no statistically significant difference (p = 0.341) due to the low sample size. The mean follow-up period was 26.7 months (6.7 SD) with a minimum of 18 months and a maximum of 36 months. Figure 4 shows patients distribution by operated levels. Figure 5 demonstrates comparative day-1 post-operative and 1-month VAS dysphagia distribution between ACDF and arthroplasty. Table 1 shows dysphagia rates reported in current literature as compared to the present series (Modified from Shriver).
Table 1 Dysphagia rates reported in current literature as compared to the present series (Modified from Shriver 2017). FU = Follow-Up
| Author | Day-1 (95% CI) | End of FU Rates | FU Months |
|---|---|---|---|
| Soriano 2018 | 23.5 % (Mean) 9.1% (Artroplasty) 25.7% (ACDF) |
0% (Since 1-Month) | 31.85 |
| World Global Rate | 8.5% | 46.7 | |
| Graham 2014 | 8.1% | 6 | |
| Burkus 2014 | 9.8% | 84 | |
| Hou 2013 | 9.7% | 22.5 | |
| Kepler 2012 | 39% | 1.5 | |
| Coric 2011 | 6.1% | 24 | |
| Cheng 2011 | 16.7% | 36 | |
| Mcaffe 2010 | 8% | 24 | |
| Anderson 2008 | 7.2% | 24 | |
| Fernández-Fairen 2008 | 6.1% | 24 | |
| Xie 2007 | 13.3% | 24 | |
| Song 2006 | 2.6% | 24 | |
| Bazaz 2002 | 20.2% | 6 | |
| Bruneau 2001 | 1.9% | 24.6 | |
| Bolesta 200 | 6.7% | 42 |
Discussion
Current research on dysphagia after ACSS has focused on surgical approach (ACDF vs. TDR, vs. anterior cervical corpectomy and fusion vs. ZERO-P)21-26, steroid use (intraoperative vs. post-operative, local or systemic)27, and graft implications (bone morphogenetic proteins two use vs. autografts vs. allograft)18,28, as well as overall incidence28, but few researches have been taken over the impact of minimally invasive approaches to reduce incidence rates.
Minimally invasive approaches have the common aim of avoiding biomechanical complications and are associated with decreased pain and morbidity in the early post-operative period, as well as with faster recovery rates accounting for the increasing number of safe outpatient-procedures being performed nowadays even in the cervical spine29,30. The present study was conceived based on the concept that minimally invasive approaches reduce soft-tissue trauma31, and so for reduce post-operative complications, such as dysphagia, a well-known complication related to soft-tissue edema (among other causes) after an ACSS6. Theoretically, a lesser rate of dysphagia in the early post-operative period would provide a proof of concept that minimally invasive tubular approaches, in fact, reduce soft-tissue trauma and their related complications. Worldwide rates of dysphagia are reported to be around 8.5 (5.7-11.3%, 95% confidence interval) as reported by Shriver et al. in their meta-analysis of 14 papers evaluating post-operative dysphagia after ACDF28, among them, the greatest rate of dysphagia (39%) was reported by Keppler on a cohort study with mean follow-up of 1.5 months1, becoming also the paper with the shortest follow-up, which translates in a high dysphagia rate in the early post-operative period, providing evidence of the important role of soft-tissue trauma in the genesis of dysphagia, a fact that can help understand why steroids have proofed effective in reducing early post-operative dysphagia32-34 driven by their known anti-inflammatory effects. Conversely, our present series results report a 9% rate of dysphagia by 1-month follow-up, presenting a 9% dysphagia rate in day-1 post-operative that fully recovered by the end of follow-up.
Conclusions
Based on this result, we can assume that minimally invasive techniques may provide an effective and safer surgical approach to the anterior cervical spine to reduce post-operative dysphagia related to soft-tissue trauma, as stated by the present series results effectively reducing early post-operative dysphagia to 9% in day-1 post-operative (as compared to 39%) and to 0% (as compared to 8.5% reported worldwide, 46.7 months mean follow-up) by 1-month follow-up. Further research with a level 1 evidence randomized clinical trial may help underscore the importance of adopting minimally invasive techniques in the armamentarium of spine surgeons to achieve better results in the anterior cervical spine, a surgical procedure that is well known by their excellent results, that can further been improved by reducing soft-tissue trauma-related complications that have potentially life-threatening outcomes such as dysphagia, and by the same time increasing patient satisfaction by a faster recovery rate and reducing hospital stay.











 nueva página del texto (beta)
nueva página del texto (beta)