Background
Periampullary cancer accounts for over 30,000 cancer-related deaths per year in the United States1. The incidence increases to 87.2 cases per 100,000 in patients over 80 years of age. Risk factors for pancreatic cancer are unknown; however, it is considered that some may be coffee, tobacco, and a history of chronic pancreatitis or diabetes2.
Survival in periampullary bile duct cancer is 20-25%, for ampullary disease, it is 30-40% and for duodenal tumors, 50-60%; for this reason, some surgeons recommend only palliative care3,4. At diagnosis > 80% are considered unresectable with a 5-year survival after pancreaticoduodenectomy (PD) of 15-20%5.
PD is considered the surgical standard for biliary, periampullary duodenal and pancreatic head neoplasms. It is the only curative treatment option in these pathologies. PD has an accepted low mortality rate of 3-5% with a high morbidity of 40-50% due to pancreatic fistulas and delayed gastric emptying6-8.
Some long-term consequences of PD are malnutrition associated to weight loss, malabsorption, and chronic need of supplementation due to a deficiency of micronutrients that are normally absorbed in the proximal intestine9. Pancreatic fistula is the most feared complication; therefore, multiple techniques of pancreatojejunostomy anastomosis have been described. No technique has proven to be a permanent solution to this problem.
Materials and methods
This was a retrospective cohort study of cases retrieved from the Department of Statistics of the "Dr. José Eleuterio González" University Hospital in Monterrey, Mexico. All PD cases from 2005 to 2014 were reviewed. This article does not contain any studies with human subjects performed by any of the authors, no informed consent was required, and no identifying information is included. Patients with resectable tumors defined by the absence of distant metastases and without local extension to the celiac axis, hepatic artery, and the superior mesenteric artery were included. Patients treated with derivative surgery or with the absence of a clinical record were excluded. We obtained 178 cases, of which 27 were excluded resulting in a total of 151 patients who underwent PD. This was a single surgeon and single-center study.
Other variables reviewed were age, gender, initial symptoms, medical history, comorbidities, hospital stay, pre-operative studies, number of transfusions, days in intensive care, classification of the American Society of Anesthesiologists (ASA), surgical time, clinical stage, post-operative complications, morbidities, and post-operative mortality.
With regard to the surgical technique, all patients were approached with a bilateral subcostal laparotomy. Resectability without vascular invasion or extrahepatic disease was confirmed during surgery. The Kocher maneuver was performed and the common bile duct was divided. Subsequently, an anterior plane is created, the portal vein and superior mesenteric artery are dissected, and the distal stomach is divided preserving the pylorus. Afterward, the distal jejunum was divided near the ligament of Treitz and the previous pancreas was divided in front of the portal vein; subsequently, the branches of the superior mesenteric vein are ligated and the hepatic artery is dissected. Three anastomoses are performed:
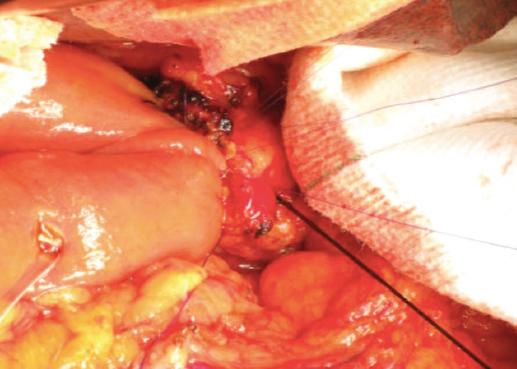
(1) antecolic terminoterminal hepaticojejunostomy; (2) terminoterminal telescope pancreatojejunostomy, which was performed in all cases with duct mucosa and pancreatic duct cannulation (Fig. 1), with additional intermittent circumferential points to the jejunum, which were reinforced with a second circumferential layer and placement of a pancreatic duct catheter; and (3) laterolateral gastrojejunostomy. Selection bias was avoided by the patient list provided by the statistics department, performance bias with all the procedures done by a single surgeon, and reporting bias was avoided by the revision of surgery professors.
For statistical analysis, SPSS version 22 (IBM, Armonk, NY, USA) was used. The variables were compared using the Mann-Whitney U-test and the Chi-square test with a statistical significance of p < 0.05.
Results
A total of 151 cases with a mean age of 55 years and a total of 91 men (60%) and 60 women (40%) were reviewed. The mean body mass index was 25 kg/m2, with 76 (50%) patients above 25. Regarding the clinical history, a diagnosis of Type 2 diabetes mellitus was found in 50 (33%) patients and hypertension in 40 (26%), and 15 patients had a previously diagnosed carcinoma.
The most common symptoms were jaundice in 110 (73%), abdominal pain in 20 (13%), and oral intolerance in 10 (6%). Of all patients with jaundice and abdominal pain, 63% also presented oral intolerance. Regarding pre-operative weight loss, 35 (23%) patients had a loss of > 5 kg, and 40 (27%) patients had a high nutritional risk score greater than 3 points.
A pre-operative tumor size > 2 cm was reported in 50 (32%) patients. Total and direct bilirubin was reported elevated in 106 (70%) patients. Aspartate aminotransaminase increased more than twice its normal value in 55 (36.6%) patients, and alanine aminotransferase increased more than twice in 40 (26%) patients; finally, CA 19 was reported in 55 (36.6%) patients. No patient underwent preoperative chemotherapy (CT) or radiotherapy (RT) and a risk of the ASA was reported in two or higher in 116 patients (76%).
Diagnosis of ampulloma (duodenal or pancreatic head tumor) was done in a total of 131 (86.5%) patients, five cholangiocarcinoma, 10 insulinomas, and five neuroendocrine tumors. The mean operating time was 248 min with a mean bleeding volume of 1000 ml reported. For transfusions, only 25 (16.6%) patients required three or more transfusions. 35 (23%) patients required intensive care, lasting a mean of 9 days. Mean hospitalization was 11 days with 110 (73%) patients staying < 10 days.
As for morbidity, 30 (20%) cases reported: 12 collections (7.9%), 10 pancreatic fistulas (6.6%), and 8 episodes of post-operative bleeding (5.2%). Patients with post-operative bleeding were reoperated and patients with intra-abdominal collection were managed with percutaneous catheter placement. Five post-operative mortalities (3.3%) were reported due to pancreatic fistula and abdominal sepsis.
The pathological diagnosis of 131 patients admitted to surgery was ampulloma, from which a total of 81 patients presented duodenal adenocarcinoma and 50 tumors included pancreatic head adenocarcinomas, cholangiocarcinomas, neuroendocrine tumors, and insulinomas. Mean tumor size was 1.5 cm for adenocarcinomas, 60 (46%) patients had positive nodes, and positive margins were found in 15 (11.5%).
In post-operative management, 60 (40%) patients were followed, of which 25 received CT only, another 10 RT only, and 25 received a combination of CT and RT. Distant metastases were found in 40 (26%) patients during follow-up at 2 years. 2-year survival was 38%.
Statistical analysis was done comparing the group of patients who survived and the group of patients who died (Table 1) to obtain predictors of mortality. These were the presence of a previous medical disease, days of hospital stay, post-operative margins, and weight loss.
Table 1 Comparison between survival and 2-year mortality during the 2-year follow-up
| Variables | 2-year survival (%) | 2-year mortality (%) | Survival versus mortality |
|---|---|---|---|
| Patients | 106 (70) | 45 (30) | |
| Mean age | 54 | 57 | ns |
| Mean BMI, kg/m2 | 24 | 26 | ns |
| Comorbidities | 50 (47) | 20 (44) | <0.05 |
| Initial symptoms | ns | ||
| Jaundice | 70 (66) | 40 (88) | |
| Pain | 20 (19) | 5 (12) | |
| Weight loss (kg) | 10 (9) | 0 | |
| Others | 5 (4) | 0 | |
| Mean nutritional risk | 2.29 | 2 | ns |
| Biliary dilatation | 40 (38) | 20 (44) | ns |
| Total bilirubin | 7.9 | 7.76 | ns |
| Direct bilirubin | 5.11 | 4.76 | ns |
| AST | 113 | 110 | ns |
| ALT | 106 | 105 | ns |
| AP | 392 | 294 | ns |
| Lewis antigen (CA19-9) | 57.72 | 71.02 | ns |
| Mean ASA | 2 | 2.2 | ns |
| Mean surgical time, minutes | 253 | 236 | ns |
| Mean bleeding, milliliters | 995 | 1194 | ns |
| Transfusions, units | 0.9 | 1.6 | ns |
| ICU admission | 0.5 | 1.7 | ns |
| Complications | 20 (19) | 25 (55) | ns |
| Inpatient days | 9.5 | 16.5 | <0.05 |
| Tumor size >2 cm | 50 (47) | 25 (55) | ns |
| Positive nodes (post-operative) | 45 (42) | 15 (33) | ns |
| Positive margins | 10 (9) | 5 (12) | <0.05 |
| Post-operative clinical phase | ns | ||
| T1 | 40 (38) | 25 (55) | |
| T2 | 20 (19) | 0 | |
| T3 | 40 (38) | 15 (33) | |
| T4 | 5 (4) | 5 (12) | |
| Post-operative follow-up | |||
| CT (±) RT | 45 | 15 (33) | ns |
| Weight loss, kg | 0 | 8.5 | <0.05 |
| Metastases | 20 (19) | 15 (33) | ns |
| Mean 2-year survival | 11 m | ns |
Statistical tests were done with the Mann-Whitney U-test and Chi-square test with a significance of p < 0.05, ASA: American Society of Anesthesiologists, AST: aspartate aminotransferase, ALT: alanine aminotransferase, AP: alkaline phosphatase, ICU: intensive care unit, CT: chemotherapy, RT: radiotherapy, ns: not significant, BMI: body mass index.
In addition, the node-positive group and the node-negative group were compared and no statistical significance was found. Finally, the groups of patients who suffered complications versus those without complications and only days of hospital stay and weight loss were significant (p ≤ 0.05).
Discussion
Halsted, in 1898, was the first to successfully attempt local resection of a periampullary carcinoma. Alessandro Codivilla was the first surgeon to perform a PD. Allen Whipple subsequently modified this technique in 1935. This technique for handling pancreatic tumors and periampullary was complex and was associated with a very high morbidity and mortality10.
During our 10-year experience, different aspects of this technique progressed achieving reduction in surgical times, intraoperative bleeding, and number of transfusions11. Our morbidity rate remained 20%. A serious complication is post-operative bleeding, which can be managed using interventional angiography with embolization; however, in our case, due to our available resources, reoperation was our preference.
A comparison of surgical procedures performed from 2006 to 2010 and from 2011 to 2015 was made (Table 2) and found an improvement in surgical time (−39.8 min), a reduction in intraoperative bleeding (−64.2 ml) and in the number of blood units transfused intraoperatively (−0.5). Characteristically, most of our patients arrive at late stages of disease with obstructive jaundice and advanced tumor sizes12. This is why distant disease and advanced cancer stage in our post-operative patients were reported. Early diagnosis is important and a high clinical suspicion is essential in this pathology.
Table 2 Surgical evolution of patients in a 10-year period
| Year of surgery | Total patient | Surgical time, min | Transoperative bleeding, mL | Transfusions, units |
|---|---|---|---|---|
| 2006 | 13 | 323 | 768 | 2.5 |
| 2007 | 16 | 315 | 618 | 2.8 |
| 2008 | 14 | 357 | 620 | 2.3 |
| 2009 | 16 | 269 | 664 | 1.6 |
| 2010 | 17 | 289 | 632 | 1.1 |
| Total 2006-2010 | 76 | 310.6 | 660.4 | 2.06 |
| 2011 | 15 | 317 | 779 | 2.3 |
| 2012 | 18 | 315 | 675 | 1.7 |
| 2013 | 16 | 282 | 560 | 2 |
| 2014 | 12 | 190 | 267 | 0.5 |
| 2015 | 14 | 250 | 700 | 1.3 |
| Total 2011-2015 | 75 | 270.8 | 596.2 | 1.56 |
| Improvement | 151 | −39.8 | −64.2 | −0.5 |
| Statistical significance | ns | ns | ns |
Statistical tests were done with Chi-square test with a significance of p < 0.05, ns: not significant.
Our technique with duct-mucosal anastomosis and pancreatojejunal telescope anastomosis with cannulation of the pancreatic duct (Fig. 1) managed to maintain a rate of pancreatic fistula of 6.6%. This technique helps decrease the rate of pancreatic fistula and leakage preventing accumulation of pancreatic secretions and anastomosis to exclude direct contact with the pancreatic juices, the most important handicap includes patients with hard pancreas which is associated to a higher fistula rate13.
Mortality in our review is 3.3%. One of the most feared complications is a pancreatic fistula, which can quickly endanger the patient's life because it leads to peritonitis and severe sepsis. All patients who died before 2 years had similar symptoms and laboratory findings compared to patients with a better outcome. Factors such as personal background, post-operative complications, and surgical time were significantly different between these groups. Patients with a poor prognosis characteristically presented a significant weight loss during their post-operative evaluations.
Despite maintaining a low mortality rate, some surgeons, due to a lack of technical resources, identify an advanced stage of disease, and therefore, only a derivative procedure can be offered. Laparoscopic PD is considered only in a subset of patients because this procedure is associated with an increased incidence of pancreatic fistulas14. Therefore, open surgery remains our institutional choice. The number of procedures performed in recent years has been increasing. It has already been reported that the effect of high-volume centers in the evolution of patients involves a reduction in perioperative morbidity and mortality.
Several limitations of this study include that this was a single institution and single surgeon experience, an important number of patients did not attend their follow-up in our institution.
Conclusion
Negative prognosis predictors in our study include the presence of previous comorbidities, positive resection margins, and post-operative weight loss. Pancreatic fistula is the most feared complication; no technique has proven to be a permanent solution to this problem. The end-to-end telescope anastomosis with duct-to-mucosa anastomosis and cannulation of the pancreatic duct appears to have a lower fistula rate than reported before.











 text new page (beta)
text new page (beta)