Introduction
Osteochondral lesions of the talus (OLTs) are characterized by damage to the articular cartilage of the talus and the underlying subchondral bone. They include a group of injuries that involve juvenile osteochondritis dissecans (JOCD) and osteochondral fractures of the talus. OLTs are frequently associated with sports-related injuries.1 The treatment in juvenile patients differs from that in adult patients because the youth population have a higher healing potential.2 The aim of this review is to provide an overview of the current evidence for the diagnosis and treatment of OLTs in the skeletally immature patient.
Etiology
Despite increasing recognition among children and adolescents, the etiology and pathogenesis of OLTs remain largely unknown. It is widely accepted that OLTs are caused by both traumatic and nontraumatic events. Regarding traumatic events, up to 50% of ankle sprains and over 70% of ankle fractures may develop osteochondral lesions. Tol et al,3 reported that 93% of patients with a lateral lesion had a history of trauma; whereas only 62% of patients with a medial lesion had a history of trauma.
A traumatic insult can cause damage to the cartilage and lead to microfractures of the subchondral bone. Subsequently, synovial fluids penetrate the microfractures, and the loading leads to high fluid pressure, which in turn induces osteonecrosis and cyst formation. In addition, poor vascularization of the talus increases the risk of osteonecrosis and diminishes the healing capacity.4 OLTs without a history of trauma may be caused by multiple factors including repetitive microtrauma, ischemia, subsequent avascular necrosis, genetic predisposition, and endocrine or metabolic factors. Moreover, recent evidence suggests that JOCD may be associated with vitamin D deficiency.5 Ankle morphology may also be related to these lesions, resulting in altered contact mechanics and increased stress on cartilage loading of the affected articular surface.6
Diagnosis
Most patients recall a previous initial trauma as a pain trigger in association with diffuse ankle pain, swelling, and tenderness deep in the medial or lateral ankle that increased with weight bearing and activity. Additionally, recurrent sprains and unbalanced loading of the foot may be noted. Physical examination of OLTs is challenging because of their often vague and nonspecific symptomatology. A meticulous clinical examination should be performed focusing on the areas of tenderness, limitation in the range of motion of the ankle, subtalar and talonavicular joints, medial and lateral ankle stability, and hindfoot alignment.7
Currently, there is no consensus regarding the appropriate imaging protocol. The standard diagnosis includes weight-bearing anteroposterior (AP) mortise and lateral radiographs of the ankle. Nevertheless, they have low sensitivity, and the OLT can be misdiagnosed in over 40% of cases. Plain films may reveal other pathological conditions such as fractures, coalitions, exostoses, and tumors. Hindfoot alignment can be radiologically assessed using the Saltzman or Meary views. In the vast majority of cases an MRI is useful to evaluate OLTs activity and concomitant injuries (Figure 1).8 Likewise, a CT scan can accurately identify and locate lesions. Moreover, it can identify the amount of bone attached to the osteochondral lesion, define the size of the subchondral cysts, and allow evaluation of bony healing.9

Figure 1: Anteroposterior and lateral radiographs, and magnetic resonance imaging (MRI) showing a stable posteromedial OLT.
Recently, several new imaging methods have been developed. SPECT-CT provides an accurate assessment of the location and metabolic activity of an OLT, other pathologies, and the surrounding bone.10 Nevertheless, the radiation to which a patient is exposed should not be overlooked. Computed tomography arthrography (CTA) has a higher sensitivity and reliability regarding detection of osteochondral lesions at the ankle compared with conventional MRI.11 It has also been reported as a follow-up marker for articular tissue growth and subchondral bone consolidation.11 A disadvantage of CTA is that it is an invasive procedure.
Treatment options and outcomes
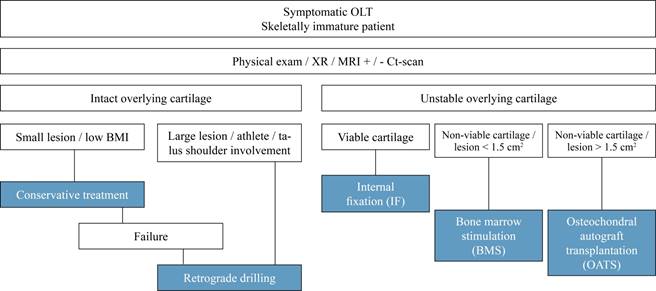
Treatment strategies of OLTs in the skeletally immature population depend on the magnitude of symptoms, lesion morphology (stable versus unstable, overlying cartilage integrity, etc.), size, nature of the lesion (traumatic versus JOCD), ankle stability, lower extremity alignment, and previous treatment.2 The preferred treatment algorithm is described in Figure 2.
Nonoperative treatment
Non-operative treatment is indicated for symptomatic, stable lesions. The aim of conservative treatment is to facilitate the natural healing potential of the damaged tissue and resolve edema within the joint by avoiding weight bearing. Although there are no precise protocols for conservative strategies, treatment most commonly used consists of restriction of activities, immobilization, non-steroidal anti-inflammatory drugs (NSAIDs), and rehabilitation to regain ankle motion, strength, proprioception and stability. A recent systematic review12 assessed the evidence for conservative management of OLTs, reporting a pooled success rate of 44% (95% CI: 37-51%), and a conversion to surgery rate of 62% (95% CI: 54-70%). Although conservative treatment may relieve symptoms in the short term in 4 of 10 patients, the long-term outcomes of these treatment strategies have not been established. It is questionable whether this is an optimal outcome, particularly in an adolescent athlete. In our experience, conservative treatment is best indicated for skeletally immature patients with low body mass index (BMI) and small stable lesions.
The authors initiated a randomized controlled trial on the optimization of non-operative treatment in children with OLT. Based on promising results in the knee,13 this trial compares a strict protocol in the intervention group to «supervised neglect» in the control group. Patients in the intervention group undergo non-weight-bearing immobilization with a cast for six weeks in phase one. At the end of phase one, patients must have shown clinical progression in order to go to phase 2. In phase 2, which starts between week 6 and 12, a supervised rehabilitation starts with progressive weight bearing. If patients show clinical and radiological improvement at the end of phase 2, phase 3 can be started between week 12 and 16. The final phase is aimed at supervised return to sports. Clinical and radiological follow-up for at least two years is standard. As this trial is currently underway, the results are not yet available.
Surgical treatment
Surgical treatment is usually indicated for symptomatic stable lesions that fail primary conservative management and for unstable lesions.14 Relative surgical indication is an athlete with a symptomatic stable lesion with large size and/or involvement of the talus shoulder. Surgical options include retrograde drilling, internal fixation, bone marrow stimulation (BMS) and reparative or replacement techniques. Treatment should be individualized, considering lesion characteristics and patient and parent preferences. If the articular cartilage of the lesion is intact on all articular surfaces, including the vertical surface in the gutter, and the cartilage is normally consistent with arthroscopic probing, retroarticular drilling is indicated. The success rate ranges from 78% to 99% in different series15,16,17 (Figure 3). If the articular surface is breached but the cartilage is normal in appearance and consistency, and a piece of subchondral bone is attached to the lesion, internal fixation (IF) may be indicated through either an arthroscopic or an open approach, using bioabsorbable pins, screws, or bone pegs. In addition, local cancellous bone can be added with the lift-drill-fill-fix technique to improve healing potential.18 The advantage of this treatment option is that it restores the natural congruency of the subchondral bone and preserves hyaline cartilage. A systematic review12 reported a success rate of 79% (95% CI: 61-91%) with internal fixation.
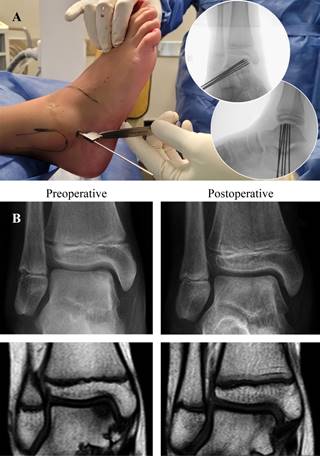
Figure 3: A) Retroarticular drilling using fluoroscopic-guided 1.6 mm K-wires. B) Preoperative and postoperative (6 months follow-up) magnetic resonance imaging (MRI) showing complete healing after retrograde drilling.
Patients with OLTs that are less than 1.5 cm with degenerated overlying cartilage, and those that have failed IF, are probably best treated with arthroscopic debridement and BMS (Figure 4). Series have shown good outcomes in 68-85%.19,20,21,22 In contrast to the native articular hyaline cartilage, BMS induces the formation of fibrocartilaginous tissue, which has inherently different biological and mechanical properties that are likely to degenerate over time. OLTs that are greater than 1.5 cm in diameter and have damaged and nonviable overlying articular cartilage, as well as lesions that failed previous surgery, may perform best with osteochondral autograft transplantation (OATS), talar osteoperiostic grafting from the iliac crest (TOPIC procedure),23 fresh osteochondral allograft, or chondrocyte regeneration techniques. These treatments can provide satisfactory clinical results but are technically demanding and have disadvantages; including donor site morbidity, talar surface mismatch, and limited availability of graft material. This is not a common scenario in young patients, and available data is very limited in the pediatric-adolescent population. Moreover, medial malleolar osteotomy is often required to gain perpendicular access to lesions. Therefore, these surgeries are usually postponed until the physis is closed2 (Figure 5).

Figure 4: Arthroscopic view showing an osteochondral lesion of the talus after debridement and bone marrow stimulation using a microfracture pick.
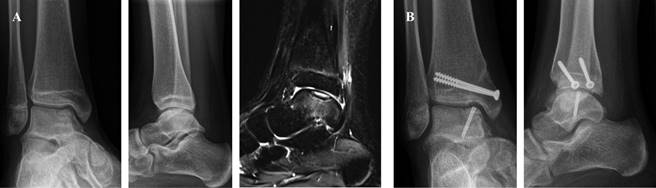
Figure 5: A) Anteroposterior and lateral weight-bearing radiographs, and magnetic resonance imaging (MRI) showing a posteromedial unstable OLT in a 15-year-old skeletally mature girl. B) Lift-drill-fill-fix (LDFF) technique was performed with bone graft harvested from tibial osteotomy.
Additionally, preoperative recognition and consideration of malalignment is critically important in cartilage surgery. In skeletally immature patients with significant deformities guided growth can be utilized for surgical correction.
Conclusion
OLTs are a relatively uncommon source of ankle pain in skeletally immature patients. An individualized treatment algorithm, guided by patient and lesion characteristics, should be indicated. Nonoperative treatment has a limited role in symptomatic lesions. Retroarticular drilling is indicated for symptomatic lesions with intact articular cartilage that fail nonoperative treatment. Unstable lesions may be treated with fixation or fragment excision and BMS depending on the osseous component and size. Larger lesions with poor articular cartilage can be treated using more complex reparative or replacement techniques. Current evidence demonstrates that surgical treatment can produce satisfactory clinical outcomes in the short- and mid-term follow-up. However, further well-designed clinical trials with high methodological quality are required to establish the most effective treatment.











 nueva página del texto (beta)
nueva página del texto (beta)