Introduction
Mirror hand syndrome, it is a very rare dysontogenic deformity of the upper extremity, a spectrum of cubital dimelia, characterized mainly by the symmetrical duplication of the image of the fingers, the ulna, ulnar carpal bones, absence of thumb and, in occasions, of the radius; with symmetric polydactyly from the midline, with an absent thenar region and with trifalangic fingers in semiflexion (due to the weakness of extensor muscles of the forearm), also described as ulnar deviation with an active and passive limitation for palmar extension.1 There are usually alterations of the bones and muscles of the forearm, which are more evident in the spectrum of classic ulnar dimelia, affecting both the proximal and distal joints.2 Also, it is often accompanied by an alteration of the lower extremities or some other congenital malformation.3 An attempt has been made to explain the genetic alteration of the malformation, finding specific genes with variable expression and multilocus.4 There are approximately 60 cases described in the literature since its first description in 1587.5,6
Al-Qattan et al.1 classified this deformity as a spectrum (Table 1), based on it, this patient presents an intermediate mirror type 3A (in the so-called «classical» form of the spectrum of mirror hand, the forearm contains 2 ulnae, one hypoplastic in most patients).
Table 1: Classification of mirror hand-multiple hand spectrum (Al-Qattan MM et al ).
| Type | Name | Clinical features |
|---|---|---|
| 1 | Ulnar dimelia | Multiple fingers with two ulna: |
| Type A: each ulna es well formed | ||
| Type B: the preaxial ulna lacks the styloid process or is hypoplastic | ||
| 2 | Intermediate type | Multiple fingers with two ulna (one of the ulna is vestigial) and a radius |
| 3 | Intermediate type | Multiple finger with one ulna and a radius: |
| Type A: radius well-formed | ||
| Type B: hypoplastic radius | ||
| 4 | Mirror hand syndrome | Bilateral multiple fingers in complex syndactyly |
| Type A: Sandrow syndrome = the forearm contains two ulna | ||
| Type B: Martin syndrome = the forearm contains an ulna and a radius | ||
| 5 | Multiple hand | Complete duplication of the hand including the thumb with a normal forearm |
Also, we can classify it according to the classification proposed by Swanson7 and adopted by the American Society for Hand Surgery (ASSH) and the International Federation of Societies for Hand Surgery (IFSSH), having a defect by duplication type III (Table 2).
Table 2: Classification of congenital hand deformities (IFSSH).
| Type | Description |
|---|---|
| I | Failure of formation |
| II | Failure of differentiation |
| III | Duplication |
| IV | Overgrowth |
| V | Undergrowth |
| VI | Constriction band syndromes |
| VII | Generalized anomalies and syndromes |
One of the main objectives of the surgical correction of the mirror hand deformity is the reconstruction of the thumb, which is done by the pollicization of one of the radial fingers. In this article, we present a bilateral mirror hand syndrome, treated with bilateral Buck-Gramcko type pollicization in 2 surgical times 6 months apart, as well as functional evaluation with particular attention to the thumbs.
Case presentation
We present the case of a patient admitted to our hospital, presenting bilateral polydactyly. The patient had no family history of congenital malformations, and as a past medical illness, she was diagnosed with Hirschsprung’s disease at birth, requiring surgical treatment at one month of age, with resection and derivation of the aganglionic segment, without complications.
Physical examination presented (Figure 1) both symmetrical thoracic extremities, without shortening nor scapular waist or joint elbows deformities, with posterior hypoplastic forearm musculature, without limitation for prone-supination, both wrists in flexion pose at 40o, limited to 20° extension. The hands with the presence of 6 fingers in both hands in an attitude of flexion, presenting three post-axial triphalangeal fingers and three preaxial, morphologically normal. The examination shows complete mobility arches in shoulders and elbows, without joint instability, with limitation in both wrists (palmar flexion of 75°, dorsal extension 20°, abduction and adduction 5°), the arcs of mobility of the postaxial fingers was normal, and the preaxial fingers showed complete mobility arcs but decreased strength 4/5 on the Daniel’s scale, without pain. Simple X-rays of both hands were requested (Figure 2), finally integrating the diagnosis of bilateral mirror hand syndrome.

Figure 2: Simple hand X-ray: polydactyly is observed, with the presence of 6 metacarpal bones with their respective phalanges, with absence of thumb, presence of 2 nuclei of ossification of the carpus and radio-ulnar growth physis. Six triphalangic fingers are seen in both hands, with a distal hypoplastic phalanx of the first radial finger of the left hand.
After an informed consent by the parents of the patient, surgical treatment was decided on, in 2 surgical times 6 months apart, which consisted of bilateral pollicization using the principles described by Buck-Gramcko8 for the reconstruction of the thumb keeping the more functional accessory radial finger and a transfer of the intrinsic muscles. The surgical technique is described below, which was the same in both surgical times.
Starting with the incision, although there are many described for pollicization of the thumb in mirror hand syndrome,9,10,11 none is based on the principle described by Buck-Gramcko in the functional and cosmetic requirements, so the characteristics of our approach were:
Wide approach for the dissection of the anatomical elements, which achieves a limited scar.
A cutaneous flap to allow full abduction and opposition of the thumb.
A scar that is not around the base of the «new» thumb, to avoid retraction and trophic changes.
Form a «fold» from the base of the middle finger to the base of the thumb, in a precise position, reducing risk of retraction.
After the incision on the palmar and dorsal side in the hypothenar region corresponding to the 1st and 2nd radial finger, dissecting to the tendinous plane, we released the interosseous muscles of the first radial finger, identifying and releasing the neurovascular bundles, and the extensor and flexor tendons. A carpometacarpal arthrotomy and ablation of the skeleton of the second radial finger was performed.
Scheker-type incision is made in the second radial finger, neurovascular bundles are identified and released from flexor II to flexor IV and pulleys A1 and A2, performing microdissection of the common digital nerve to zone IV, ligating the radial digital artery of the third radial finger. We continue with the identification and release of interosseous muscles, lumbricals muscles, intermetacarpal ligament and extrinsic extensor tendons as well as the dorsal venous system.
Subsequently, a section was made through the distal physis of the 1st radial metacarpal to perform a carpometacarpal arthrotomy and ablation of the first metacarpal and the second radial finger, maintaining the reduction in hyperextension of the metacarpal head and fixation with 0.35 K-wire, making the fixation of metacarpal to the distal carpus with 4-0 nylon suture.
The first radial ray was rotated longitudinally by 30°, palmar abducted by 40°, to avoid a hyperextension deformity and fixed with absorbable sutures and in position with a 0.35 K-wire. Based on previously described techniques (Pintilie et al10) tendon transfer was made from the common extensor of the fingers to the lumbrical with a interosseous tenodermodesis to the radial aspect of the finger, the interosseous fixation to remnants of pulleys with plication of the extensor apparatus extrinsic towards the thumb, so that the radial intrinsic muscles function as abductors, and the ulnar muscles as their synergists (Figure 3).
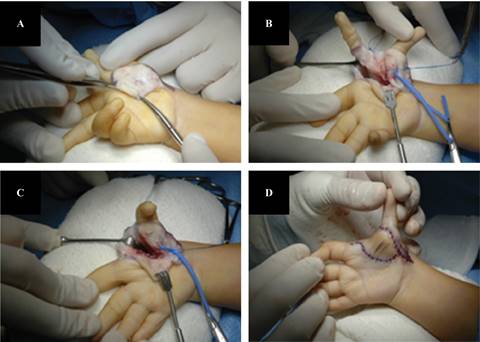
Figure 3: Surgical technique: Scheker type incision is made in radial second finger (A), neurovascular bundles are identified and released from flexor II to flexor IV and pulleys A1 and A2 (B), ablation of first metacarpal and second finger radial (C) and wide flap closure avoiding scar retraction (D).
The closure of flaps was performed with 5-0 Nylon and, at the end of surgery, the thumb had a satisfactory aesthetic appearance, the attitude of the wrist in discrete flexion was still present, so we left a splint with a Spica, the only technical difference between surgeries was that a Hemoclip (vascular ligation) was used in the left hand (Figure 4). With ischemia on average of 97 min (99 min and 96 min respectively) and a total average surgical procedure duration of 193 min (197 min and 190 min respectively). We had no neurovascular complications.

Figure 4: Simple hand X-ray (postoperative): five fingers are observed in both hands, with a Kirschner in the first carpometacarpal joint in the form of a temporary fixation.
The cast and K-wire were removed four weeks after surgery and a short arm thumb Spica splint was fabricated. She received postoperative physical therapy and occupational therapy, based on physical agents (paraffin) to facilitate healing, pain control and tissue regeneration, laser and therapeutic ultrasound and electro-stimulation to thenar region (reactivation and recruitment of motor muscle fibers) were also applied.
Occupational therapy facilitated recruitment of muscle fibers for fine and thick grasps and scopes. Activities for encouraging grasp pattern include tearing up paper, picking up pencils, opening containers, playing with small objects (cars, coins and blocks), coloring/scribbling and pulling apart sticker, obtaining excellent response for the flexor pollicis longus. We continued with a splint to improve the position of the thumb in the carpometacarpal joint, and with occupational therapy, favoring a thick and fine grasp for 1 year (Figure 5).
Results
There are a variety of factors that affect outcome,12 including status of fingers, age of surgery, technical factors (incision, technique, dressings, etc.), the surgeon and rehabilitation. The main factor is the preoperative status of the index finger and the presence or absence of adequate muscles/tendon units. At the two-year follow-up, the patient presented the following:
The active ranges of mobility of the interphalangeal and metacarpophalangeal joints of the thumb have remained stable in both hands. She presents a wide range of movement in the ulnar joint (flexion-extension 120-10°, pronation-supination 0-30°) and in the wrist joint (palmar flexion 80°, dorsal flexion 45°, adduction 5° and abduction 20°) as well as a good hold function of the hand were achieved with thumb flexion MCP 0-40, PIP 5-45° and abduction-adduction 0-50°. We achieved a complete opposition of the new thumb with respect to the other fingers.
The strength of the clamp between fingers was for 75.2% of the force normal for age, while the force of the lateral clamp was for 66.3% and that of the fist was for 69.1%.
The result of the subjective assessment was that the parents considered the function of the hand and right thumb as Good, and of the left hand as Excellent; the appearance of both hands as Good, based on the quick-DASH and PRWE questionnaire (Patient Rated Wrist and Hand Evaluation).13 The satisfaction of the surgeon with the function and appearance of both surgeries, was 85% and 90% respectively.
Discussion
There are few descriptions of the mirror hand syndrome in the literature. There may be a complete duplication of the hand, including the thumb with a normal radius and the ulna.3 King and Hoyes6 described a case with eight digits in the hand and a forearm with an ulna and a distinguishable radius. Yang et al7 reported a case with multiple fingers but with a different radius and ulna. Barton et al2 described a variant with multiple fingers, two ulnae (one vestigial) and one radius. These variants are probably intermediate between the classic ulnar dimelia and multiple hand deformities, since the duplication of the hand is incomplete.
This rare malformation of both hands presented great surgical challenges. Primary reconstruction, particularly pollicization, must be done as soon as possible.3 And hope that it is not necessary to make additional corrections, referring to the function of the elbow and wrist, which in this case had no congenital malformation. Temporary immobilization by a Kirschner wire in the metacarpophalangeal joint is a valuable way to achieve a correct position of pollicization.
The comparison of the results of this study with previous studies is difficult because most of them have provided a minimum objective description of the physical characteristics and a limited subjective evaluation of the aesthetic result without long-term postoperative follow-up.
The patient in our case report had a radius and an ulna clearly discernible and, therefore, cannot be classified as ulnar dimelia, otherwise «non-classical mirror hand», presenting a normal skeletal pattern of the forearm, as well as normal function of the elbow and forearm joint. The lack of extension of the wrist is common in the true ulnar dimelia, since the lack of a radius is usually accompanied by a lack of extensors of the wrist, it is not clear why there was weakness of the extensor mechanism of the wrist in this case, we try to explain it by means of a dichotomy between bone development and muscular development. Nowadays, our patient is able to perform her daily activities with both hands, particularly after the improvement of the mobility and strength arcs obtained due to a specialized physical therapy.
Due to the dynamic nature of the deformities of the mirror hand, the associated functional and structural alterations can develop even after the initial successful reconstruction,13 so we recommend a long-term follow-up, since the secondary surgical corrections will be efficient at any age, stating that primary surgery has to be done as early as possible taking advantage of the patient’s cerebral plasticity in terms of use and function of the limb. The ideal age to perform surgery is debatable. Even though earlier surgery takes advantage of brain plasticity and ease of incorporation into activities, we must deal with the relatively small anatomical size of the neurovascular and musculocutaneous structures. We recommend pollicization at about one year of age to allow for some hand growth, while optimizing the positive aspects of youth.











 nueva página del texto (beta)
nueva página del texto (beta)




