Introduction
The distal radioulnar joint (DRUJ) is a hemi-joint, and together with the proximal radioulnar joint it forms the radioulnar joint. It is formed by the radius sigmoid notch and the ulnar head. The DRUJ parallel surfaces provide pronation and supination in a range of 150o-180o,1 while a difference in the articulating curvature yields certain osseous stability.2,3 Stabilization of this joint is provided by both intrinsic and extrinsic stabilizers, the most important being the triangular fibrocartilage complex (TFCC) and the joint capsule.4 These structures prevent the DRUJ from luxation during movement3 and transmit the load from the hand and wrist to the elbow and shoulder,5 making the DRUJ a weight bearing joint that needs congruency to function. The highest degree of mechanical efficiency of the DRUJ is achieved when in neutral position with the elbow in 90o of flexion.
Ulnar shortening (US) osteotomy has been used to treat TFCC tears with or without instability,6 ulnocarpal abutment,7,8 and early osteoarthritis.9 US is contraindicated in advanced cases of DRUJ osteoarthritis. Nevertheless, when the ulnar head is still partially covered with cartilage, US adjusts the contact area between the sigmoid notch and the ulnar head. US not only changes the contact area inside the joint, but it also tightens the radioulnar and ulnocarpal ligaments.10 The tightening of these ligaments may also improve mild DRUJ instability. US decreases the axial force over the TFC yet maintains its lifting ability against gravity force, which is the most important function of the DRUJ. Another US relative contraindication is the presence of an oblique, distally orientated sigmoid notch, the type 3 according to De Smet, due to an incidence increase of degenerative changes.11,12,13 However, it could still be a valid option while trying to address DRUJ early osteoarthritis,9 and it should not be used in severe OA when all of the cartilage has been worn out. For the early stage there are other options available, such as radial sigmoid notch osteotomies,14,15 ulnar metaphyseal osteotomies16,17 and soft tissue reconstruction or interposition procedures.18 Traditionally, «salvage procedures» have been used for end stage DRUJ OA,18 but none of them restore DRUJ stability and function except joint replacement.19,20,21
Fifteen years ago, a series of 32 patients treated with US for early osteoarthritis (OA) was published by the senior author, showing good and excellent results reported in 56% of the cases.9 Even though some information regarding US results has been produced since then, to our understanding there is no previous study regarding the risk and rate of having a secondary DRUJ procedure, particularly DRUJ implant arthroplasty replacement after US osteotomy. The purpose of this study was to evaluate patients that had US, and its relationship of the sigmoid notch type with presence of OA and the necessity of DRUJ replacement after US.
Materials and methods
After obtaining IRB approval for the study, 130 charts from patients who had osteotomy procedures at the distal end of the forearm performed by the senior author between 2002 and 2016 were obtained. Inclusion criteria included patients that undergone US for painful early OA, DRUJ instability and ulnar abutment, diagnosis for each of these conditions was done clinically and radiographically. Six patients that had radial shortening were excluded and 5 more with incomplete charts were eliminated from the analysis (Figure 1). 124 wrists of 119 patients underwent ulnar shortening osteotomy with Rayhack’s technique22 for ulnar impaction syndrome, DRUJ instability or painful early DRUJ osteoarthritis, in whom symptoms did not resolve with conservative treatment and the necessity of DRUJ replacement after US. A retrospective review of the clinical course of these 119 patients was performed, which included type of sigmoid notch, indications for the procedures and demographic data.
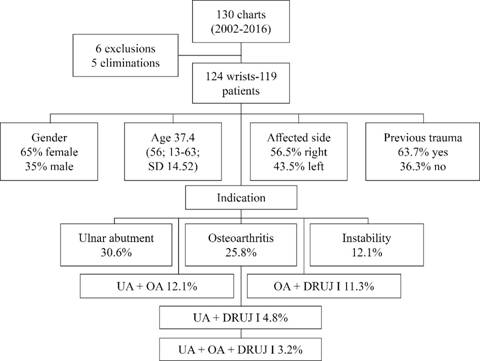
Figure 1: Flow chart depicting the patient demographics and review procedure. The indication is also enlisted with patients with osteoarthritis (OA) in bold letters. SD = standard deviation, UA = ulnar abutment, OA = osteoarthritis, DRUJ I = distal radioulnar joint instability.
Demographics
Eighty-one patients (65%) were female and 43 were male (35%). The mean age at the time of the US osteotomy was 37.4 years ± 14.52. The right side was affected in 70 cases (56.5%) and the left in 54 (43.5%). The indications for the osteotomy were ulnar abutment (UA) in 38 cases (30.6%), DRUJ early osteoarthritis (EO) in 32 cases (25.8%), DRUJ instability (DI) in 15 cases (12.1%), combined UA and EO in 15 cases (12.1%), 4 cases with UA, EO and DI (3.2%), 6 cases with combined UA and DI (4.8%) and EO and DI in 14 cases (11.3%). In total, 69 patients had OA in different stages as US indication, as an attempt to decrease the progression of OA. Previous wrist trauma was present in 79 patients (63.7%), but not in the other 45 patients (36.3%) (Figure 1). In those patients with previous trauma, the time elapsed between injury and US was 3.5 years ± 6.6.
Clinical and radiographic evaluation
All patients were evaluated at every office visit by the senior author. All of them had preoperative and postoperative X-rays done in standard position, which is 90o of elbow flexion and shoulder abduction with the forearm in neutral rotation. The ulnar variance was then assessed prior to and after surgery visits as described by Palmer11.23 The sigmoid notch type according to De Smet11,13 was then identified measuring the sigmoid notch angle, and finally classified in type 1 those with a positive angle, meaning a conical shape; type 2, neutral angle, a cylindrical shape; and type 3, negative angle, hemispherical shape (Figure 2). Older X rays were assessed directly on negatoscope and newer ones with OmniVue®Web, version 2.4 Build 63. (Genesis Digital Imaging, Inc. 2009.) software.

Figure 2: Schematic DRUJ morphology, showing the three sigmoid notch types as described by DeSmet. Positive angle equals conical shape (type 1), neutral angle a cylindrical shape (type 2), and negative angle a hemispherical shape (type 3). Modified from: De Smet L, Fabry G with permission.11
Surgical procedure
The main goal of surgical treatment was to stop or reduce pain and other symptoms produced by ulnar abutment or DRUJ instability and to stop or slow down DRUJ OA progression, but not necessarily to achieve neutral or negative ulnar variance. An oblique controlled osteotomy was performed in all the cases by the senior author, using Rayhack system generations I or II (Wright Medical. Memphis TN). The specialized instrumentation allows the creation of two precise 45o cuts and a known amount of ulnar shortening. It also facilitates additional compression of the bone surfaces. In the majority of cases the plate was applied on the volar aspect to the ulna to counteract the gravity forces that could make the construct fail. After surgery, the wrist was immobilized with a long arm splint in neutral position. After two weeks, the wrist was placed on a long arm cast or brace. Active range-of-motion exercises were started at 6 weeks, and weight-bearing was allowed when there was clinical and radiographic evidence of osseous union.
Follow-up
During the postoperative follow-up, serial X-rays were taken at the first visit at two weeks after surgery until a clinical diagnosis of healed bone. This diagnosis was defined by both signs of trabecular bone formation with blurring of the osteotomy gap, and absence of pain during physical examination. The pain was reported as present or absent after bone consolidation. Postoperative forearm radiographs were measured to quantify the amount of ulnar shortening. Complications were found in 4 of 124 wrists after US. One patient had a non-displaced fracture post-hardware removal that healed after closed immobilization. One patient had a delayed union that healed after surgical treatment with iliac crest bone grafting. Two patients had axillary block neuritis related to the anesthetic procedure.
Statistical analysis
Variables were operationalized, and qualitative variables were categorized to allow statistical analysis. Categorical and ordinal variables were expressed using frequencies and ratios. Descriptive statistics were reported as the mean, range and standard deviation. For statistical purposes only, the patients were divided into 3 groups and 7 sub-groups based on the indication for surgery due to the co-existence of more than one DRUJ initial pathology in some wrists and 3 groups based on their sigmoid notch type, to determine whether there was an association between sigmoid notch type and the indication for ulnar shortening or the conversion to the DRUJ implant. In univariate analysis, the Student t-test was used for comparison of continuous variables and the chi-square test was used for comparison of categorical variables. In multivariate analysis, from two to seven-way ANOVA was performed for subgroups analysis. Statistical analysis was done using StatPac, version 4.0 with the significance level set at 0.05.
Results
Of the 124 wrists treated with ulnar shortening osteotomy with Rayhack’s technique, 105 patients (84.7%) had 2.5 mm shortening, 13 patients (10.5%) had 5 mm shortening, 5 patients (4%) had 7.5 mm shortening, and 1 more (0.8%) had a 15 mm long shortening. The preoperative ulnar variance ranged from -5 to 15 mm with a mean of 1.73 ± 2.47 mm. The postoperative ulnar variance ranged from -6.1 to 2.8 mm with a mean of -1.38 ± 2.50 mm. The overall bone healing time was an average of 3.33 ± 129.6 months. At the time of healing 54% of the patients were free of pain (n = 67), and 46% of patients had residual pain (n = 57).
Twenty-four patients (19.4%) had a cubital tunnel release procedure done in the same extremity before or after the US. The mean follow-up was 25.39 ± 29.68 months. The sigmoid notch type distribution for type 1 was 69 patients (55.6%), type 2 was 32 patients (25.8%), and type 3 was 23 patients (18.5%). The mean sigmoid notch angle was 8.55 ± 13.6 degrees. Sixteen patients (12.9%) had workers’ compensation insurance. Thirty-seven patients (30%) had hardware removal, including the 13 patients that had further DRUJ replacement.
Of the 13 patients that required a DRUJ semi-constrained arthroplasty (conversion rate 10.4%), the time from US to DRUJ arthroplasty was 21 ± 21.9 months on average. To determine if the sigmoid notch type could be related to DRUJ pathology and necessity of DRUJ prosthetic replacement, a further analysis was made in this group of patients, in whom the sigmoid notch was type 1 in 6 patients (46.1%), type 2 in 4 (30.8%), and type 3 in three (23.1%). After ANOVA analysis, there was no significance between groups for age, indication, amount of shortening and time to bone healing. However, a slight tendency for conversion of the sigmoid notch type 3 group was observed, but it did not reach significant difference (p values 0.55 & 0.54) (Figure 3). While narrowing the analysis with the subgroup of patients with OA, a tendency for conversion was also seen, but again, did not reach significant difference (p values 0.45 & 0.38) (Figure 4).

Figure 3: The graphic shows a slight tendency for conversion to DRUJ arthroplasty was observed with a sigmoid notch type three group, but it did not reach significant difference.
Discussion
This study of a large series of patients supports and extends previous findings regarding US as treatment for DRUJ pathology. Patients showed successful healing with a 1.7% nonunion rate, superior to many reports in the literature of 6.3 to 10% using different techniques. Megerle et al.24 reported a 10% nonunion rate (4 of 40 patients) using whether a 6-hole AO 3.5-mm-low contact dynamic compression plate (LC-DCP) (DePuy-Synthes) or 7-hole US plate with sliding hole. In 2006, Sunil et al.25 compared a free hand US technique using standard 5- or 6-hole AO 3.5-mm dynamic compression plate (DCP) (DePuy-Synthes) on 45 ulnas with 3 nonunion cases (6.6%) vs the Rayhack technique (52 ulnas) with 0 non-unions. In a case series of 63 patients, Chan et al.26 report 4 nonunions (6.3 %), using a jig for osteotomy and 3.5 DCP for fixation. More recently, Papatheodorou et al.7 report a 164-patient series showing a 98.8% union rate, using a step-cut technique and a 7-hole 3.5-mm standard neutralization plate. Beckers et al.17 report a metaphyseal ulnar shortening technique, using two self-tapping lag screws (1.5 or 2 mm) as a method for fixation with a 100% healing rate (only 12 patients). In their series, de Runz et al.27 had one nonunion in 46 patients (2.2%) using transverse u oblique osteotomies and a 3.5-mm LC-DCP for fixation. Finally, Rayhack28 reports only one nonunion in a small series of 23 patients treated with his technique.
In the present study, 54% (67/124) of the patients reported complete pain relief. Previous studies reported on US have varied with respect to complete pain relief. Scheker and Severo9 reported a similar finding of 16/32 patients (50%) with complete pain relief. During their study, Megerle et al.24 used the visual scale analogue (VAS) for pain and the postoperative pain levels averaged 4.9 (range, 0-8) on the VAS with no statistical difference between the two groups in relation with plate location. Papatheodorou et al.7 reported a postoperative pain VAS score of 1.6 on a cohort of 164 patients. Beckers et al.17 showed that 6 of their 12 patients (50%) had pain after the metaphyseal US, and those 6 patients required a second surgery for implant removal, resulting in pain relief in only two of them. On the other hand, Rajgopal et al.6 reported a 6.7% (5/75) rate of complex regional pain syndrome. De Runz et al.27 reported 3 of 46 patients with postoperative pain, but they reported only pain related to hardware location. Chan et al.26 reported persistent discomfort as a common postoperative finding in 32 out of 63 patients (51%). Finally, Sunil et al.25 reported persistent pain in 19 out of 95 patients (20%) and 39 patients (41%) with complete pain relief.
We had a 30% rate of hardware removal, including 13 patients that underwent DRUJ replacement. When compared with previous results, Chan et al.26 reported plate removal performed at the request of the patient in 27 out of 63 (43%) cases. Rajgopal et al.6 demonstrated a 45.3% rate of hardware removal in their sample. In 2015, de Runz et al.27 reported hardware removal in 28 out of 46 patients (60.8%). The lag screws used to stabilize metaphyseal US were removed in 50% of the cases.17 Meanwhile, Papatheodorou et al.7 reported only twelve out of 124 patients (7.3%) having plate removal. Finally, Megerle et al.24 reported 11 patients with plate removal, with a larger proportion of plates removed from the dorsal aspect of the ulna than volar or ulnar locations.
The conversion rate to DRUJ implant (Aptis Medical. Louisville, KY) was also low (10.4%) and was related to persistent, severe pain at the DRUJ. Few studies have reported this indication for DRUJ replacement. Beckers et al. reported 1 out of 12 patients (8.3%) converted to a DRUJ prosthesis after a new onset of DRUJ arthritis and instability.17 It is conceived by some authors than other options, like Darrach, wide ulna excision or Sauve-Kapandji arthrodesis, rather than DRUJ replacement will have similar indications and should be considered as alternative treatment,29 but none of them restore DRUJ stability and function. According to a systematic review, semi-constrained implants are the best option for function improvement, pain reduction and preservation of DRUJ mobility.21 To the best of our knowledge, this is the first study comparing the sigmoid notch type and its relationship with a previous US and the conversion to DRUJ replacement.20,30,31 US osteotomy with Rayhack’s technique is a safe procedure with an excellent healing rate when compared with other techniques.25 US is very helpful in reducing the progression of DRUJ arthrosis due to instability or early OA and may also alleviate symptoms related to ulnar abutment syndrome.9 Concerns about OA after ulnar shortening have been highlighted in literature. In their analysis, de Runz et al.27 suggested that a substantial ulnar resection could induce the appearance or worsening of DRUJ OA; however, data from this study suggests the shortening will reduce the pain and could delay the conversion to DRUJ arthroplasty. Chan et al. explored the possibilities of underreported US complications;26 however, in our review we found similar results to the published data. An external concern reported in the literature is the possibility of late radio-lunate arthritis,32 or avascular necrosis of the ulnar head following US. While these complications have not developed to date in this series of patients, we hypothesize they would be related to poor US indication, technical deficiencies of the surgical approach or altering the wrist blood supply during hardware placement.33
Regardless of the surgical technique used, one of the US main advantages is the possibility to address young patients with DRUJ pathology. If not treated, these patients will require further invasive surgery, such as DRUJ prosthetic replacement. Ulnar shortening can delay the progression of severe OA and thus the need for DRUJ replacement. Finally, the results obtained during this study suggest that there was an effect of sigmoid notch type 3 on the frequency of patients who needed a DRUJ replacement. The results shown in this study are limited by the absence of a control group, and the small number of patients that had conversion to DRUJ replacement. Nonetheless, possible trends found suggest further studies should be done to confirm the influence of sigmoid notch type 3 with the DRUJ replacement.











 nueva página del texto (beta)
nueva página del texto (beta)



