Introduction
The extensor tendons of the hand are in a relatively superficial position; consequently, they are highly susceptible to injury from lacerations, bites, burns, or blunt trauma. Extensor tendon injuries are more frequent than flexor tendon injuries1 and are very common (61%)2 as they are not protected as well as the flexor tendons due to their superficial location and lack of overlying subcutaneous tissue. Extensor tendon injuries may require operative intervention, depending on the complexity of the injury and the zone of the hand involved. Kleinert defined eight zones-four odd numbered zones overlying each of the joints and four even numbered zones overlying the intervening tendon segments.3
Extensor tendon injury can result from various injuries. The most common mechanisms are sharp object direct laceration, crush injury, avulsions, burns, animal or human bites, and deep abrasions.4 Spontaneous rupture of the digital extensor tendon has been described in patients following traumatic injuries, Vaughan-Jackson’s syndrome (VJS), Kienbock’s diseases (KD), and in patients with rheumatoid arthritis (RA). Tendon ruptures in VJS are primarily caused by gradual attrition of the tendons on the ulnar head, which, in RA, may subluxate or dislocate dorsally due to loss of the normal supporting structures. The process of tendon wear may be exacerbated by osteophytes and sharp prominences resulting from primary or secondary degenerative changes of the bone.5 KD is the necrosis of the lunate bone; this, though rare, is an important cause of spontaneous extensor tendon rupture.6 Indeed in the KD it is always present protrusion of the segmented lunate or the deformed lunate in all cases; these anatomical changes create friction to the normal sliding of the extensor tendons.7 Rupture of the extensor tendons of the fingers is a common and disabling complication of RA. It results from tenosynovial invasion of tendons or, more commonly, from their attrition on the ulnar head.8
No cases of rupture of the digital extensor tendons have been reported secondary to unrecognized carpal lunate fracture. In this case report, the authors describe a case of spontaneous rupture of digital extensor tendon in a patient with unrecognized lunate fracture. The purpose of this work is to describe the clinical case, paying attention on the pathogenesis, diagnosis and treatment.
Case report
The patient
A 73 years-old man with no significant medical problems was seen in Orthopaedic Department of the University of Chieti (Italy) for an inability to extend the IIIo, IV o and V o finger of his right, dominant hand.
Anamnesis, the patient denies direct trauma; he reported a sudden acute pain in his right wrist with functional impotence of the fingers, after a glass lift. No risk factor was present, no rheumatic disease or chronic joints diseases have been reported. The past medical history, the patient reported that he had done during his working life the mason work, but already five years he was retired.
The patient says mild pain on the 3nd, 4th and 5th finger of the hand for a few days, without functional impairment.
Clinical examination
On physical examination, not noted any signs of scars, bruises, burns on the skin of the wrist and hand. A rubber band, swollen and painful lump under the skin was present on the back of the wrist, in correspondence between the lunate bone and the space between the 3rd and 4th metacarpal bone. (sixth Kleinert zone) The patient was not able to extend the 3rd, 4th and 5th finger, which remained in a flexed position. The range of movement of the wrist was 45 degree of flexion and40 degree of extension. There was no limitation of this flexion-extension of the elbow and the pronation and supination of the forearm.
Instrumental tests
An ultrasound of the back of the wrist were performed.
We have not done a wrist X-ray projections with standards, because the patient refused a direct or indirect trauma. Ultrasound examination reported a complete lesion of the extensor tendons of the fingers with a gap of about 2 cm.
Blood chemistry tests exclude the presence of rheumatic disease or the presence of an elevated serum uric acid.
Intraoperative findings and surgical technique
Intraoperatively, extensor tendons were found to be disrupted near radio-carpical joint. Extensor digiti minimi (EDM), along with the third, fourth and fifth extensor digitorum communis (EDC) tendons, were ruptured with fraying of the tissue in the ruptured margin. No sign of inflammation was present (Figure 1). Through the synovium which was intact, the proximal and distal stump of the extensor tendons were visualized. The tendons appear white, not hyperemic and without a reactive synovitis. The lesion was clear, with the structure fibrillated. Grossly, there appeared to be significant attenuation and degeneration of the tendons with two adhesions between them. Under the synovium on wrist joint a swelling of 1 cm was noted. The edges of the tendon were debrided and sutured using a locked modified Kessler suture with a horizontal mattress suture (2-0 caliber).
Postoperative treatment
For the first four weeks after surgery, a dynamic wrist brace was modeled. We used a dynamic splinting program opposite to the one that is used for flexor tendon repair, with an outrigger splint holding the fingers in extension and allowing full active flexion. The wrist is maintained in 30 to 40 degrees of extension. Dynamic extension is applied to maintain the MP’s and IP’s in full extension allowing for flexion. There can be a flexion stop at MP 60 degrees. The patient has been followed by a physiotherapist who applies passive mobilization for the first 20 days and then switch to active mobilization assisted in the following 10 days. At 4-6 week post surgery, the patient is encouraged to work on wrist flexion, extension, scar massage and edema control. Progressive strengthening is initiated at eight weeks. The patient is back to full duties at 12 weeks. The patient’s postoperative course was uncomplicated.
Instrumental investigations in the post operative period
In the days following the surgery, radiographic examinations were performed aimed to observe the carpal bones. The tendon injury highlighted during surgery gave grounds for suspecting the possibility of friction with the bones of the carpus.
A wrist X-ray with standard projections was performed. At a later X-ray vision of the hand it showed a not clear profile of carpal bone (Figure 2), no lunate collapse. The suspect is a lunate carpal bone fracture. Computed tomography with reconstruction confirmed the clinical diagnosis and radiological findings (Figure 3). The lunate bone comes in two pieces; they are not detectable thickening of the bone or the presence of cysts. Patient did not want to remove the dorsal fragment because he had no pain and good functionality of the hand after 8 weeks from surgery.

Figure 2: The lateral view of the wrist X-ray shows an alteration of the cortical bone lunate with suspected fracture.
Discussion
Although spontaneous extensor tendon rupture often occurs in association with RA,9,10 with osteoarthritis of the distal radioulnar joint (DRUJ)11,12 and KD,13,14 extensor tendon rupture associated with carpal lunate fracture has not been reported.
RA is the most common cause of spontaneous rupture of the extensor tendons of the hand. In fact, this disease is characterized by an alteration of tendon tissue and the patient’s joint. Granulomatous rheumatoid tissue invades the tendon along the vincular vessels and in time softens the tendon, which finally ruptures with strain. Also rupture may occur from attrition over bony spurs.
In all non-rheumatic cases, there is a mechanical defect between the scroll of the tendon and the bone bed. When an acute or chronic illness alters the surface of the carpal bones, the tendon no longer flows in its normal place. An attrition between the bone and the tendon is created, and this defect can slowly wear out the tendon fibers and lead to rupture the tendon.15
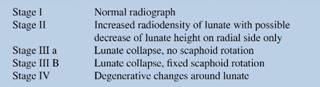
KD is an avascular necrosis with fragmentation and collapse of the lunate. It is characterized by sclerosis and flattening of the lunate. When flattening is marked, there is a rotation of the scaphoid which further adds to the stress on the lunate. Fragmentation of the lunate and secondary degenerative disease may develop later. A five stage radiographic classification system (Table 1) exists. Lichtman’s modification of Stahl’s classification is most widely used and divides the disease into five stages, from normal radiograph to degenerative changes around the lunate.16 The disease can result in deformities or bone fragmentation lunate, so attritional rupture of the extensor tendon to the index finger by a fragment of the lunate is possible.17
The lunate bone is well enclosed within the large lunate fossa of the distal radius. Fractures of the lunate are rare. Teisen and Hjarbaek18 classify the lunate fractures in 5 groups based on radiographic appearances: group I, volar pole fractures; group II, chip fractures; group III, dorsal pole fractures; group IV, sagittal fractures through the body; and group V, transverse fractures through the body. However, fractures of the lunate are controversial. It is difficult to determine whether a fracture of the lunate is acute or whether the fracture is pathologic and the result of repetitive trauma on a weakened osteonecrotic bone resulting from KD.19
In our case lunate fracture was suspected intraoperatively and investigated later. The patient reported that he had not a recent trauma to the hand and had not a history of wrist pain. Also he claims to have performed in the past a heavy and repetitive work with the upper limb (the patient was a mason). The suspect lunate bone abnormalities occurred only during surgery. In the days following surgery, X-ray and CT scan showed an outcome of the lunate bone fracture that occurred two fragments, dorsal and volar (group IV according to the Teisen and Hjarbaek classification). No signs of bone remodeling, thickening of bone, bone collapse, bone cysts were seen on CT, by excluding the KD.
In conclusion, in the hand attrition rupture of tendons is a well-known problem in absence of a clear etiology for rupture of the extensor tendons of the hand, carpal lunate fracture, can be an important cause of spontaneous extensor tendons rupture. What is certain is that we must rule out conditions such as KD, the AR, the VJS therefore an X-ray and CT examination must always run in the pre-operative diagnosis to better identify the problem.











 nueva página del texto (beta)
nueva página del texto (beta)