Introduction
Cementless fixation of femoral prosthetic components is the preferred procedure of many surgeons despite the fact that a certain percentage of the former may fail in the long term, resulting in events that alter periprosthetic bone turnover and changes that, at times, are unwanted. These changes have multifactorial causes and are mainly due to the elimination of trabecular systems that transmit mechanical stimuli and, therefore, lead to the devascularization of the proximal femoral endosteum. To the former we need to add the skeletal changes resulting from aging, the effects that certain comorbidities common in patients undergoing arthroplasty have on bone, and the use of certain medications that affect bone mineralization and metabolic turnover, with the resulting bone mass loss. New concepts in implant design have appeared as an attempt to diminish the above-mentioned changes; this is the purpose of short stems.
This relatively "new" design concept has a series of advantages. The most relevant ones include its bone-preserving features, the fact that it is less invasive and, since it is anchored mostly in the femoral head-metaphysis area, it may limit the defunctionalization of the proximal femoral bone. Other less important advantages have been described, some of which are questionable: 1) the possibility of minimizing or eliminating the difficulties that at times occur when trying to adapt a design to the anatomical geometric differences between the proximal and the distal femur; 2) some designs avoid the challenge of matching the medial implant geometry to the calcar femorale (Adam's arch); 3) they can be more easily fitted in cases of preexisting femoral bone deformities; 4) revision surgeries are easier; 5) they facilitate anterior approaches; 6) the theoretical improvement in proximal bone turnover reduces the chance of stress shielding or reactive bone changes; 7) less intraoperative bleeding is expected; 8) they require less instrumentation; 9) they help reduce inventory costs, and 10) they theoretically reduce the length of the postoperative rehabilitation period.1,2,3,4,5,6 Despite the above arguments, these and other possible advantages are valid only if one can prove that they are better than those offered by standard stems from the standpoint of survival and revision rates, clinical outcomes, and the preservation of good bone health.
The questions we should ask before making the decision of prescribing new implants are: Are their indications clearly defined? Are their clinical results better? Do they provide better or, at least equal, stability than standard stems? Are they equally or more durable? Do the different designs available offer the same advantages? To answer these and other questions one needs a clear strategy that analyzes how the different currently available short-stem designs function and what their clinical outcomes are. But before this, we need to face two fundamental problems on which, so far, no consensus has been reached: 1) define what we mean by short stem, and 2) make a standardized classification helping us group stems and compare their results as well as perform multicenter comparative analyses without mixing, to the extent possible, the various design philosophies.
The word "short" may have various meanings depending on the context where it is used. For purposes of this paper, "short" is something having little length or size. Short stems may be referred to as short hip stems, shorter hip stems or shortened hip stems. It is a fact that there is no consensus as to what the dimensions of a short stem are. It is therefore very important to reach an agreement as to what we mean by short endoprosthetic femoral implants.
Several authors have proposed stem classifications using various criteria in order to analyze their clinical outcomes.7,8,9,10,11 However, their drawback is that they mix various implant concepts, types and designs in such a way that they sometimes include even standard stems; this has led to confusion in the interpretation of results. For these and other reasons, we deem important to start a discussion that helps us better understand this type of stems.
In general, the design of short femoral implants is based on the following features: 1) anatomical region they occupy or invade, 2) basic geometric design, 3) main stress distribution zones, 4) bone resection level in the femoral head, neck or metaphysis, and 5) the orientation axes used for insertion. The purpose of this study was to review current cementless short stems considering the above-mentioned characteristics and propose a classification grouping them into families by means of a nomenclature that describes them accurately.
Material and methods
To collect data on current cementless short stems, we did an internet search in the PubMed and Scopus databases. We also consulted with various implant manufacturers, joint arthroplasty research foundations, organizations of independent experts in analyzing medical devices, and national arthroplasty registries. We excluded cemented stems and animal prototypes from this analysis. This study did not analyze clinical outcomes.
Some of the stems included are still in use, while others are part of clinical research trials, were developed only as a prototype, or have been recalled from the market. But the common denominator in all of them is that they have been implanted in human patients.
The following criteria were used to classify the designs included here in: a) the anatomical region they occupy or invade (Figures 1 and 2); b) the bone resection level (Figure 3); c) the main stress transmission areas (Figure 4); d) the relevant morphological and geometric design characteristics, and e) the orientation axes to introduce the implant in the femur depending on whether the stem is femoral neck sparing or not sparing.

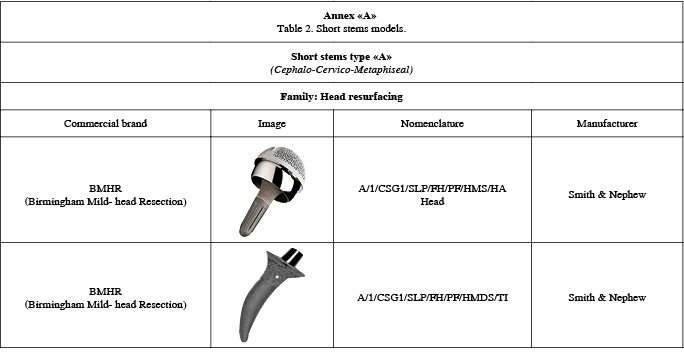
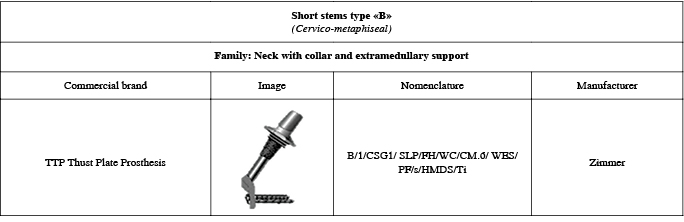
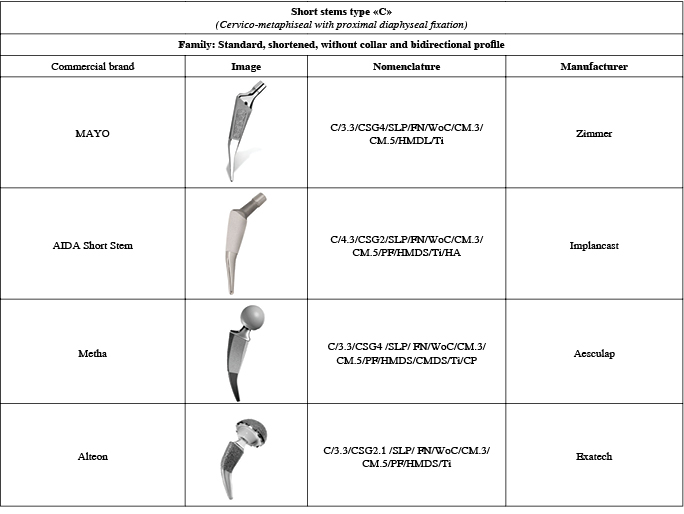
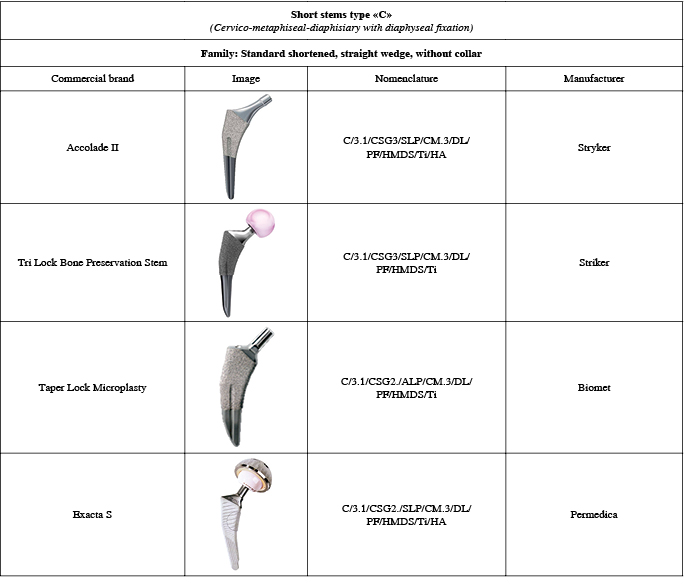
Figure 2: Classification of short stems according to the regions they occupy or invade. Type A) It occupies the head-collar-metaphysis regions. (E.g., Birmingham Mid-Head Resection) Type B) It occupies the collar-metaphysis regions. (E.g., Silent short stem).Type C) It occupies the collar-metaphysis-diaphysis regions. (E.g., TSI(tm) Neck Sparing Stem).

Figure 3: Short implants have various resection levels depending on their design philosophy, which include resurfacing implants, which are only cemented; Birmingham mid-head resection (BMHR), collum or collar implants, neck retaining implants, and standard short stems that may or may not invade the greater trochanter.

Figure 4: Load/stress transmission variables: 1) on the femoral head, 2) on all or part of the neck 3) on the calcar 4) on the metaphyseal cancellous layer, 5) on both metaphyseal cortices, 6) on the lateral metaphyseal-diaphyseal cortex, 7) on the diaphysis, and 8) some may have several simultaneous loading sites.
To determine which areas occupied by the implants in the proximal femur and their major stress transmission areas we considered the manufacturers' descriptions, the imaging analyses of the plain films published in different media, and, finally, an intuitive rationale based on the morphological analysis and the characteristics of each design. The loading/stress transmission sites may be: a) part of the femoral head, b) all or part of the neck with or without a collar, c) on the calcar, d) on the metaphyseal cancellous bone, e) on both metaphyseal cortices, f) on the lateral metaphyseal/diaphyseal cortex and g) on the shaft. All of them experience loading on several sites at a time (Figure 4), and their main morphological and design characteristics in order to define their anteroposterior, lateral and cross-sectional profiles; their overall, cross-sectional and lateral geometry, modularity, stem surface and type of primary anchoring (Table 1).
Given the huge diversity of stem models considering the above described variables, a nomenclature was designed to name them. It describes each one of them in an easy, unequivocal, unique and distinctive way, and allows classifying and grouping them in families. Most stems share several variables, but more than one of them may be present in some of the models. Table 2 describes the proposed nomenclature and its acronyms.
Results
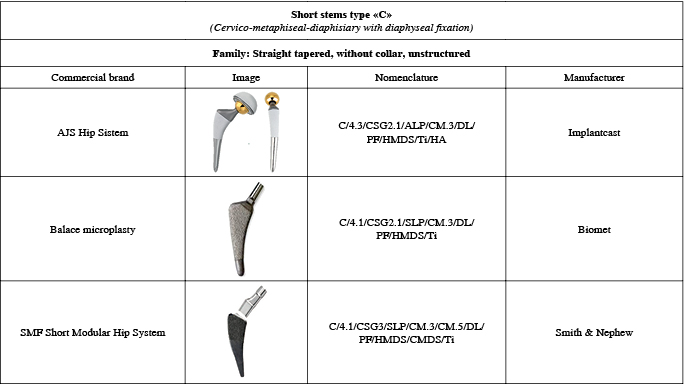
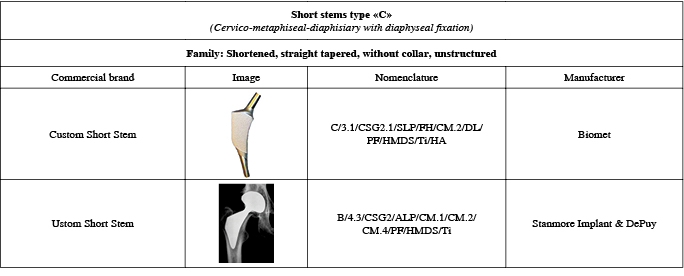
We identified 42 different models manufactured by 20 companies, which may be grouped into 3 types and 16 generic families (Table 3). Eighty-four design variables were identified in the stems analyzed (Table 4). The 42 models share several design variables.
The proposed classification in Table 5 only shows examples for each family to illustrate the methodology used for their identification, classification, and grouping. Annex "A" shows the full classification of all the stems identified in this paper (The annex is online only).
Discussion
Current short stems offer potential theoretical advantages that may exceed those offered by conventional ones. However, the former are only valid if they prove to be better from the perspective of their clinical results, long-term survival, less complications, and fewer unwanted reactions resulting from periprosthetic bone turnover. Proving their superiority involves facing two outstanding problems among many others: a) their definition, and b) their classification.
Some authors have made attempts to define them using various criteria, however: a) there is no clear definition of the numeric length that a short stem should have, b) the variable proportions between certain landmarks makes it difficult to establish correlation indices, and c) the border separating the metaphysis and the shaft is quite imprecise. Due to the above, the definition of short stem should not consider only a universal numerical value8 or the anatomical correlation indices.7
Regarding the possibility of adopting a universal numerical factor, Feyen et al.7 reported the lengths of some stems considered as short. Table 6 shows that the length range is quite broad, from 76 to 155 mm. Another attempt to name them considers their anatomical borders. Stulbergh12 states that a short stem should be less than 120 mm long, as the metaphysis-diaphysis junction is located precisely at that point. The objections to this proposal include, on the one hand, the fact that the same length cannot be used in an individual 1.85 m tall and in someone 1.60 m tall. On the other hand, although the accepted proximal limit of the metaphysis is the attachment of the hip joint capsule (at the border with the neck area), and the distal limit is located where the metaphysis ends; the problem is: where does the metaphysis end and where does the shaft start?
It is evident that the limits between the former regions are defined considering their anatomical and biomechanical features as well as the distribution of trabecular and cortical patterns in each region, which are clearly different in each of the proximal femur segments (Figure 5).
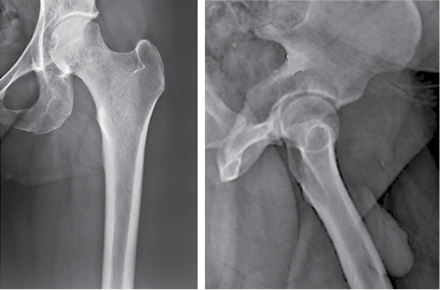
Figure 5: The morphologic features and trabecular patterns of the metaphysis are different than those of the diaphysis, as the latter is filled mainly by bone marrow with predominance of cortical bone.
We now recognize the correlation among the external dimensions of the femur (femoral head, total length, offset and external cortices). However, this does not apply to the medullary canal, as the latter has very variable endosteal characteristics that are not proportional to the outer dimensions of the femur.13
Reviewing the femur types proposed by Dorr et al.14 is very helpful to understand the problem of metaphyseal length variability. They classify them into three types. This typology shows that the variability in engaging and in the metaphyseal/diaphyseal limits results mainly from the type of femoral endosteum (Figure 6). The former suggests that metaphyseal length results mainly from the geometry of the femoral endosteum.

Figure 6: The distal limits between the metaphysis and the diaphysis are very variable and depend mainly on the characteristics of the femoral endosteum. It is evident that the extension of these regions is different depending on the type of endosteum.
Other authors7,15 have proposed other definitions of short stem using an anatomical correlation index. For instance, Feyen et al.7 have defined short stems as those whose total length (D2) is less than twice the vertical distance between the tip of the greater trochanter and the base of the lesser trochanter (D1) (Figure 7). The major objection to this proposal is that D2 is considered as part of the short stem territory, but it involves the overt invasion of the femoral shaft, where any "standard" shaft could be placed.

Figure 7: Feyen index. Short stems are those whose total length (D2) is less than twice the vertical distance between the tip of the greater trochanter and the base of the lesser trochanter (D1).3
As we have seen, several different proposals have been made to define a short stem. We did a search on the definitions of short stem, and although we did not find one that is objection-free, we agree with the one proposed by Gulow.11 The latter defines short stems are those that occupy the neck and the metaphysis, but we propose to also include those occupying the proximal borderline aspect between the metaphysis and the shaft, regardless of the type of endosteum present. If a stem overtly invades the shaft, then it should not be considered as short.
As regards the second problem, i.e., stem classification, several attempts have been made using various criteria. Some of them coincide on certain aspects, while others do not consider certain variables, but most of them mix different classification concepts and criteria (Table 7).1,7,16,17,18
Patent agencies have nomenclature systems that describe the distinctive characteristics of each element to be patented. However, up to now, there is no clinical nomenclature that can name them, so we designed a system that describes in an unequivocal, unique and distinctive way each of the stems. This system also allows us to group them in families. The final goal of such description is to propose a standardized classification that allows comparing the results of the stems. This makes it clinically useful and helps implant developers, manufacturers and analysts assess their results of stems. But it should do so in a rational, orderly way, without mixing concepts and philosophies.
The design of short femoral stems results from many factors, but they should have five basic characteristics defined by the following: the anatomical region they occupy, the geometric design characteristics, the areas where stress transmission occurs, the level at which the proximal femur osteotomy is performed, and the axes that guide their insertion depending on whether the femoral neck is spared or not.
Regarding the anatomical region occupied by stems (Table 3 and 6), only one model occupies part of the femoral head, the neck and part of the metaphysis (Birmingham Mid-Head Resection, by Smith & Nephew), but the rest of them occupy part of the neck (with several cut and angulation levels) and all or part of the metaphysis. Some also occupy part of the shaft, especially the "standard" shortened models.
Considering the geometric design characteristics, the 42 models share 84 design variables (Table 4) and transmit stresses according to their varied philosophy or design bases (Figure 4). This huge diversity of morphologic and geometric design features represents the greatest classification difficulty. It is, therefore, necessary to establish a nomenclature system that describes in an easy, unequivocal and distinctive way each of the stems, so that they can be grouped in families and their results can be more easily analyzed (Table 2).
Current short model designs establish a clear difference in the axes that guide their insertion, which is based on the preservation of the femoral neck. Femoral neck sparing stems have to adopt a more anatomical version angle than non-sparing stems. An example of this is the fact that the models with which the traditional resection osteotomy is used and that do not spare the neck are forced to correct the version with modular necks that adjust femoral version.
This communication does not intend to analyze the clinical results of the different short stems described herein, as this is the purpose of a future work that will be based on the scoring and nomenclature proposed.
Conclusions
Short stems are defined as those occupying the neck, the metaphysis and the proximal borderline aspect between the metaphysis and the diaphysis, regardless of the type of the endosteum present. If a stem overtly invades the shaft, then it should not be considered as short.
We identified 42 different models with 84 design variables, manufactured by 20 companies. This model diversity may be grouped into three types and 16 generic families.
To classify them, we propose a nomenclature that describes in an unequivocal, unique and distinctive way each short stem. This way, stems can be grouped in families and the analysis of their results can be made easier.











 nueva página del texto (beta)
nueva página del texto (beta)