Background
The recently developed technological advances in the field of urology pose a challenge, both for the residents in training as well as for the urologists responsible for training activities. The complexity of the surgical and diagnostic techniques, along with the development of new treatment plans for urological pathologies, make it necessary to maintain a commitment to continual updates, and to develop more innovative tools for the transmission of knowledge to future generations of urologists. This is evidenced by the growth and expansion of this clinical surgical specialty at a global level, with an increasing number of applicants registering to go through training. The American Confederation of Urology (CAU, by its initials in Spanish) is the third-largest urological society in the world, and it is responsible for the unification of twenty-four scientific societies, with around 12,000 active members from twenty-three countries in Latin America and Spain. Every year, around 700 doctors start a training program in the CAU environment, with a total of approximately 2,400 active residents. However, residency programs among the countries and scientific societies that comprise the CAU are heterogeneous. There are significant variations between these entities regarding the academic content, the duration, the educational pathways, and the accreditation of the educators in charge. Additionally, surgical opportunities, access to new technologies, and assessment systems are conditioned by protocols, normative availability, internal behaviors, and economic factors particular to each country and hospital due to the variability of their health national systems.
The CAU, through its educational offices, is committed to the goal of establishing programs that merge academic concepts with ongoing plan updates, research, fellowships, and permanent proposals to improve the quality of the training processes. To this end, it is important to know more about the reality of residencies in Ibero-America, to establish training schemes of excellence that are recognized at both national and international levels, through the implementation of numerous actions for the benefit of residents and young urologists.
This article aims to collect information from the different residency programs of the scientific societies that comprise the CAU regarding duration, requirements, accreditations, surgical education, academic training, research, and job opportunities, in order to obtain a situational analysis and promote the development of strategies for the training of future CAU urologists.
Materials and methods
A closed survey was conducted using the CAU EDUCACIÓN platform in Spanish and Portuguese with residents and young urologists. The survey included twenty-seven multiple-choice questions to assess the status of training, research, fellowship programs, training activities, and job opportunities at the CAU for resident urologists. Two hundred eighty-four surveys were obtained. The questions were related to country of residence, certification and duration of the residency, type of hospital, interest in making national and international publications, participation in the American Confederation of Urology Congress, urological rotation programs and fellowships, types of surgeries and technologies in hospitals, medical advice, and job opportunities to help create superior urologists.
The distribution of the survey was performed via email and the social media networks of the American Confederation of Urology between September 2019 and September 2020.
Results
Two hundred and eighty four surveys were obtained from the following Ibero-American countries: Argentina (19%), Colombia (15%), Peru (12%), Ecuador (12%), Brazil (11%), Spain (8%), Chile (6%), Mexico (5%), Venezuela (3%), Dominican Republic (2%), Uruguay (2%), Paraguay (1%), Honduras (1%), Costa Rica (1%), Bolivia (1%), Cuba (0.5%), and Panama (0.5%). One hundred and four respondents of the total were women, and the rest were men (180).
Urology Training
Regarding the type of hospital institution, 68% (193) of those surveyed completed their residencies in public hospitals, 21% (60) in private hospitals, and the remaining 11% (31) in semi-public institutions. Regardless of training site, 90% (256) noted that their residencies were accredited by medical colleges or urology societies.
The duration of residencies was variable, since 40% (113) of those surveyed stated that the length of their training was four years, 33% (94) said it was three years, and 27% (77) stated that it was five years.
Regarding the training period for general surgery, training was not compulsory in 23% (65) of the urology residencies, and only 10% (29) reported that their residencies were post-basic. In 30% (85) of the residency programs it was necessary to previously complete six months of general surgery, and for the remaining 37% (105), the requirement was twelve months. (Fig. 1)
With respect to the structuring of urology services, 55% (156) reported that their medical staff were not divided by specialty and that they performed activities on demand, while 45% (128) performed their activities by areas according to the subspecialties of urology.
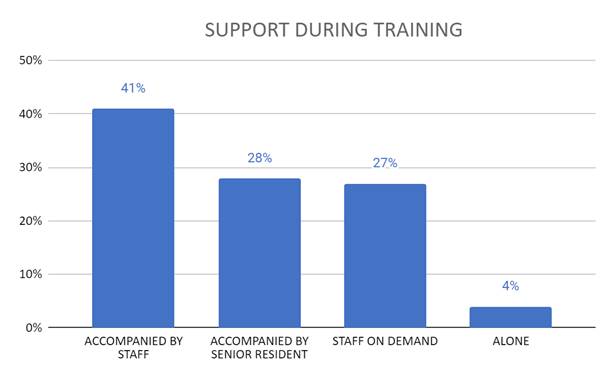
Regarding patient care, 41% (116) of the residents reported being accompanied and counseled by medical staff, 28% (80) reported being under the mentorship of a senior resident, and 27% (77) found themselves unaccompanied most of the time; but when faced with the need for a specialist, one was easily available. Finally, 4% (11) of those surveyed responded that they performed their activity alone most of the time, with little available access to expert opinions. (Fig. 2)
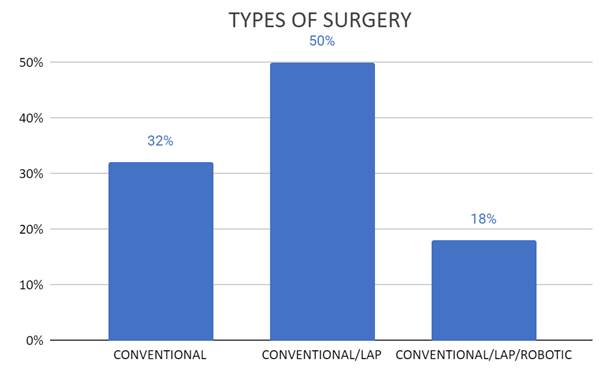
With respect to the types of surgeries performed, almost 50% (142) of the residencies included conventional and laparoscopic surgeries, while only 18% (51) of the residents were also trained in robotic surgeries. The remaining 32% (91) stated that they did not have any kind of technology in their training, performing only conventional open surgeries. (Fig. 3)
As for the type of endourological resources, 58% (165) of those surveyed were trained with flexible ureteroscopy associated with different laser energies for stone removal and prostate enucleation; while the remaining 42% (119) used a semi-rigid ureteroscope with pneumatic energy for stone fragmentation or resolved stone pathology with conventional open surgery. (Fig. 4)
Based on rotations during residency, 60% (170) responded that they had mandatory rotations in uropediatrics on a regular basis.
Concerning the perception of the quality of the academic program, 64% (182) of the residents would recommend their training to another colleague but considered it necessary to complement it with some subspecialty. In this sense, 86% (244) of all residents planned to do a fellowship. The most selected subspecialties were endourology (35%) and uro-oncology (31%).
Research
In the area of research, 76% (216) of the residents were required to produce and submit scientific papers for national conferences or journals during their formative years. However, only 33% (94) had the opportunity to make presentations or publications internationally. Forty-three percent (122) of the residents said they did not belong to an international urological society.
Fellowship programs and training activities of the CAU
All the residents surveyed were interested in the training activities of the CAU, either through courses or e-learning platforms. Ninety-seven percent of them (275) said that they were interested in doing some CAU rotation.
Job opportunities
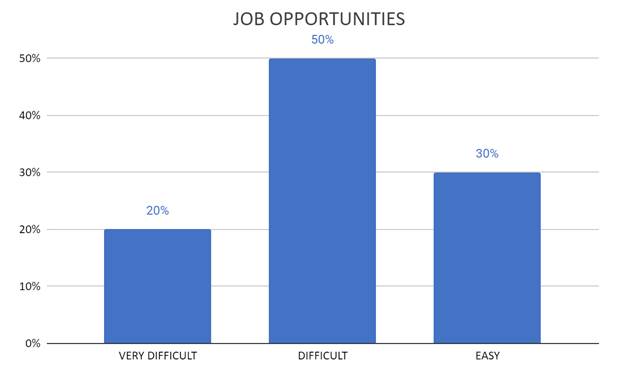
According to the survey, half of the residents (142) thought finding a position after completing their residency was to some extent difficult, and 20% (57) thought it was extremely difficult.
The remaining 30% (85) were confident that they would be able to find employment after completing their residency. (Fig. 5)
Discussion
Urology training occurs in a complex scenario due to the large number of subspecialties that comprise it. Also, CAU residency programs are different to health system programs regarding economic resources, access to technologies, and other characteristics. It is important to note that residency programs should provide the knowledge and skills that are required, so that future urologists feel confident and secure in their daily practice, before the usual urological procedures.
A 2018 study by Angulo et al. mentioned that there are significant variations in the period of residency training and the educational path. Some of the results that support this heterogeneity are related to the duration of the residencies, accreditations, the possibility of publication in scientific journals, and subsequent job opportunities.1
The data related to the duration of the training programs provided in said paper is like that of our series. With respect to the accreditation of residencies, Angulo states that CAU residencies generally maintain periodic recertification programs every 2-5 years. In our work, although the latter was not evaluated, most of the residencies were accredited by medical colleges or urology societies.
However, only a few residents showed interest in conducting research that generates publications and presentations at international congresses, although most universities try to promote the presentation of papers at national congresses. Residents need courses, workshops, symposiums, and congresses, where they can obtain knowledge, make observations, and practice the skills that are demanded in a specialty as technical as urology. The research, writing, and preparation of a scientific article are other aspects of training that should not go unnoticed.2 Support programs were initiated from the research office of the CAU, with various activities and fellowships to stimulate the development of quality scientific work.
When asked about the likelihood of finding a position, 70% of the respondents had a perception of it being difficult or partly difficult. According to García Sanz et al., the possibility of employing recently specialized urologists is high, reaching 100% six months after they complete their specialization. However, opportunities related to job quality are not so positive, as there is a vast instability associated with a high proportion of temporary contracts of less than six months.3
Many residency programs include laparoscopic training in their curricula. Nevertheless, most residents would prefer greater exposure to minimally invasive techniques and robotics throughout their residencies.4-6 In our series, almost half of the residencies performed conventional and laparoscopic surgeries, while only 18% of residents were also trained in robotic surgeries.
Meanwhile, according to Juan Gómez Rivas et al., the level of surgical participation in urology training in Europe is low, as is the level of training in models and attendance at courses.7 This data shows practically no differences from those described by residents trained in the US, due to their lack of involvement in endourological surgeries and training in this area.8 Concerning this lack of participation and opportunities during the residency program, in our series, 64% of the respondents thought that despite their training being effective, it needed to be complemented with some subspecialty. For that reason, they consider a fellowship. These programs consist of a temporary stay (generally one year) in a prestigious center that offers academic and practical training, with full integration into the activities of a specialized unit.9,10
Sánchez Margallo et al., stated that it is necessary to think about new models of surgical teaching based on structured programs, where learning includes the continuous acquisition of knowledge, the achievement and evaluation of skills, evidence-based competencies, and the training of surgical techniques outside the operating room in safe environments through tools based on simulation.11 Implementing high-quality simulations for training will be one of the significant challenges in pursuing therapeutic success and patient safety in the coming years. This certainly must be added to the current system of rotations by other centers that include many training hospitals. In this way, residents will be able to learn techniques, or become familiar with departments that they may not have access to at their centers of origin.12
The feeling of being well-trained is a strong predictor of burnout syndrome. This was recently demonstrated in a study in which a quarter of French urology residents were affected by the syndrome. About 33% of the participants thought that their training did not allow them to be competent in their work.13 In relation to burnout syndrome, Carrión et al. concluded that surgical exposure in Germany is low for residents and that work-related psychosocial stress is high, suggesting the need for structural improvements in programs. In Italy, 52% of residents reported working more than fifty hours per week, thus overall satisfaction with residency was moderate. Meanwhile, in Spain, around 83% of residents reported between four and six monthly twenty-four-hour shifts, and up to 68.8% continued with their normal daily schedule after a twenty-four hour shift.14
Over the past few years, women have had a greater role in the workplace, particularly in medicine. At the same time, a combination of their increasingly demanding professional roles, family responsibilities, and personal interests has adversely affected many women’s quality of life. As a result, they may experience stress, depression, anxiety, and marital problems more frequently, which may contribute to secondary somatic disorders and increased consumption of alcohol and tobacco.15
The inclusion of new technologies in the new training model, particularly e-learning, may decrease the dependence of residents on tutors in certain phases. A variety of platforms are available for acquiring knowledge, including the internet, apps, social networks, and online training.16
The same applies to telemedicine, which currently offers many potential advantages for both patients and specialists. However, its implementation entails a change in the organization of medical departments and individuals. Technology is a cornerstone of telemedicine, which is why we need to incorporate the available options of email, videoconferences, social networks, applications, telehealth platforms, and webinar platforms to help maintain good communication and patient privacy.17 A limitation of this study was the number of participants which is well below the number of active residents, which is approximately 2,400. Despite this, the number of participating countries, the distribution, and the obtained results give us a more complete picture of the situation of the current training of CAU residents.
Conclusion
Residency programs in the CAU environment are heterogeneous regarding the years of duration, accreditations, resources, and training modalities. A specific and uniform plan is necessary to ensure proper training, regardless of the unit where the residency is performed. The use of new technologies, the accreditation of tutors, the validation of acquired skills, and the use of simulations should be implemented to achieve more comprehensive and more homogeneous residential programs. New studies and efforts should be considered to standardize the acquisition of skills, guarantee access to surgical learning courses and fellowships, promote academic development, encourage residents’ participation in research, and achieve an objective evaluation of the specialty in pursuit of the training of the future urologist.











 nueva página del texto (beta)
nueva página del texto (beta)