Introduction
Urinary tract infections (UTIs) are among the most prevalent community-acquired and hospital-acquired infections.1 An estimated 1 million cases of nosocomial UTIs occur in the United States annually, accounting for considerable morbidity and healthcare costs.2 In Mexico, UTIs are the third cause of infectious diseases, surpassed only by upper respiratory tract infections and gastrointestinal infections.3 No structural or functional abnormalities in the genitourinary tract or relevant comorbidities are related to an uncomplicated UTI. A complicated UTI is associated with a condition of the genitourinary tract or the presence of an underlying disease, which increases the risk of a more serious outcome.1,4
The most common agent causing UTIs is Escherichia coli (E. coli). 1,4 However, complicated UTIs are caused by a greater variety of agents with higher antibiotic resistance rates, and a higher frequency of failure to empiric treatment.5,6 In recent years, increased drug resistance has been reported worldwide, including the emergence of extended spectrum β-lactamase (ESBL)-producing agents in Enterobacteriaceae, mainly E. coli and Klebsiella pneumoniae.7,8 ESBLs confer resistance to penicillins, cephalosporins, and aztreonam.9,10
Few studies have reported the risk factors associated with UTIs caused by ESBL-producing E. coli, such as diabetes, recurrent UTIs, urinary catheterization, genitourinary pathology, previous bacterial infection, intravenous antibiotic treatment, hospitalization, and previous antibiotic therapy.11-13
The prevalence of ESBL-producing bacteria in UTIs is heterogeneous and dependent on geographic region.14 Therefore, the aim of the present study was to determine the etiologic agents, antimicrobial resistance rates (including ESBL-producing bacteria), and risk factors associated with ESBL-positive UTIs at a tertiary care hospital in Northern Mexico.
Materials and methods
Setting and study population
A retrospective cohort study was performed at a tertiary care teaching hospital in Monterrey, Mexico. Approval by the Local Ethics Committee was previously established (UR14-004). Inclusion criteria included positive urine cultures with signs and symptoms of UTI from outpatients and hospitalized patients, within the time frame of March to October 2017. Asymptomatic bacteriuria, incomplete clinical records, and urine cultures with two or more causative agents were excluded. UTI classification was based on the European Association of Urology (EAU) criteria, as either complicated or uncomplicated, and hospital-acquired UTIs (HA-UTIs) or community-acquired urinary tract infections (CA-UTIs).4
Antimicrobial susceptibility and ESBL determination
Species identification of urine isolates was performed using MALDI-TOF mass spectrometry (Microflex, Bruker Daltonics). Drug resistance of E. coli isolates was determined by the microdilution plate method for all drugs except fosfomycin, which was established through the agar dilution method. The results were interpreted according to the Clinical and Laboratory Standards Institute (CLSI) criteria.15 The antibiotics tested were amikacin, gentamicin, amoxicillin-clavulanic acid, aztreonam, ceftriaxone, ertapenem, ciprofloxacin, levofloxacin, nitrofurantoin, fosfomycin, trimethoprim-sulfamethoxazole, and colistin. Carbapenem-resistant isolates were screened to detect carbapenemase production using the CarbaNP test.15 The production of ESBL in E. coli and Klebsiella spp. isolates was performed using the double-disc test, according to the CLSI.15
Statistical analysis
Categorical variables were expressed in frequencies and percentages. Numerical variables were expressed as a mean and standard deviation. Clinical and demographic characteristics were analyzed using the χ2 test for the categorical variables, and the T-test (or Mann-Whitney U test in the absence of normal distribution) for the continuous variables. Statistical significance was set at a p <0.05. The statistical analysis was performed utilizing SPSS version 20.0 software.
Results
Study population and UTI causative agents
A total of 353 patients were included. Their median age was 47.3 years, and females were the most affected (64.3%, n=227). CA-UTIs were the most frequently detected UTIs, accounting for 65.4% (n=231), and 34.5% (n=122) were HA-UTIs. Of the HA-UTIs, 91.8% (n=112) were complicated, and 8.2% (n=10) were uncomplicated. Regarding the CA infections, 73.6% (n=170) were complicated UTIs and 26.4% (n=61) were uncomplicated (Figure 1).
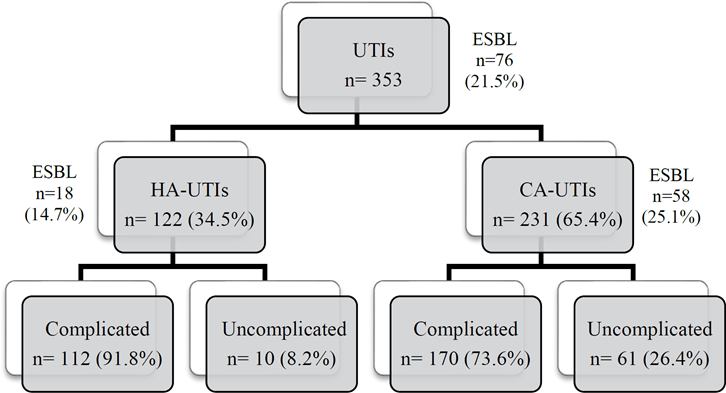
Figure 1 Classification of the HA-UTIs, CA-UTIs, and the complicated and uncomplicated UTIs in the study population, as well as the distribution of the ESBL-producing agents.
The clinical data of the study population are shown in Table 1. The most common underlying factors were previous use of antibiotics (41.6%, n=147), type 2 diabetes (32.3%, n=114), and chronic renal disease (18.1%, n=64). The most frequent agent was E. coli (57.2%, n=202), followed by Candida sp. (9.9%, n=35) and Klebsiella spp. (9.1%, n=32). ESBL-producing agents were isolated in 21.5% of the total UTIs (76/353), and 25.1% of the CA-UTIs were ESBL producers (58/231), compared with 14.7% of the HA-UTIs (18/122). A total of 37.1% (n=131) of the patients had a urinary catheter, and 35.1% (n=125) had a recurrent UTI. Complicated UTIs (p<0.001), males (p=0.027), previous antibiotic use (<0.001), immunodeficiency (p=0.015), and urinary catheter (p<0.001) were more frequent in the HA-UTIs, whereas E. coli (p<0.001), uncomplicated UTIs (p<0.001), pregnancy (p=0.008), recurrent UTIs (p=0.01), urosepsis (p=0.002), and lithiasis (p=0.041) were more frequent in the CA-UTI group. In addition, we detected an association between the presence of urinary catheter and Candida sp. infection (21.3%) (p<0.001, data not shown).
Table 1 Characteristics of the study population and HA-UTI and CA-UTI sub-classification.
| Characteristic | Total (n=353) | HA-UTI (n=121, 34.3%) | CA-UTI (n=232, 65.7%) | P value | OR (95% CI) |
|---|---|---|---|---|---|
| Causative agent | |||||
| E. coli | 202 (57.2) | 44 (21.8) | 158 (78.2) | <0.001 | 0.26 (0.16-0.41) |
| Klebsiella spp. | 32 (9.1) | 12 (37.5) | 20 (62.5) | 0.714 | 1.15 (0.54-2.44) |
| Other* | 180 (51.0) | 66 (36.7) | 114 (63.3) | ND | ND |
| Demographics | |||||
| Male | 126 (35.6) | 53 (42.1) | 73 (57.9) | 0.027 | 1.66 (1.06-2.62) |
| Age ≥ 60 years | 120 (34.0) | 41 (34.2) | 79 (65.8) | 0.911 | 0.97 (0.61-1.55) |
| UTI type | |||||
| Complicated | 282 (79.9) | 112 (39.7) | 170 (60.3) | <0.001 | 4.02 (1.98-8.17) |
| Uncomplicated | 71 (20.1) | 10 (14.1) | 61 (85.9) | <0.001 | 0.25 (0.12-0.51) |
| Underlying factors | |||||
| Previous use of antibiotics | 147 (41.6) | 66 (44.9) | 81 (55.1) | <0.001 | 2.18 (1.40-3.41) |
| Type 2 diabetes | 114 (32.3) | 37 (32.5) | 77 (67.5) | 0.576 | 0.87 (0.54-1.40) |
| Chronic renal disease | 64 (18.1) | 28 (43.8) | 36 (56.3) | 0.088 | 1.61 (0.93-2.90) |
| Arterial hypertension | 56 (15.9) | 15 (26.8) | 41 (73.2) | 0.183 | 0.65 (0.34-1.23) |
| Immunodeficiency | 29 (8.2) | 16 (55.2) | 13 (44.8) | 0.015 | 2.53 (1.18-5.46) |
| Pregnancy | 27 (7.6) | 3 (11.1) | 24 (88.9) | 0.008 | 0.22 (0.06-0.74) |
| Urologic alterations | |||||
| Catheter | 131 (37.1) | 81 (61.8) | 50 (38.2) | <0.001 | 7.15 (4.39-11.66) |
| Recurrent UTI | 124 (35.1) | 32 (25.8) | 92 (74.2) | 0.011 | 0.54 (0.33-0.87) |
| Urosepsis | 51 (14.4) | 8 (15.7) | 43 (84.3) | 0.002 | 0.31 (0.14-0.68) |
| Obstructive uropathy | 49 (13.9) | 12 (24.5) | 37 (75.5) | 0.110 | 0.57 (0.29-1.14) |
| Urologic surgery | 44 (12.5) | 15 (34.1) | 29 (65.9) | 0.944 | 0.98 (0.50-190) |
| Lithiasis | 29 (8.2) | 5 (17.2) | 24 (82.8) | 0.041 | 0.37 (0.14-0.99) |
| Neurogenic bladder | 28 (7.9) | 9 (32.1) | 19 (67.9) | 0.779 | 0.89 (0.39-2.02) |
| Benign prostatic hyperplasia | 25 (7.1) | 6 (24.0) | 19 (76.0) | 0.250 | 0.58 (0.22-1.49) |
| Tumor | 18 (5.1) | 4 (22.2) | 14 (77.8) | 0.259 | 0.53 (0.17-1.63) |
| Radiotherapy and/or chemotherapy | 10 (2.8) | 4 (40.0) | 6 (60.0) | 0.714 | 1.27 (0.35-4.59) |
*Other pathogens include: Candida sp. (n=35), Enterococcus sp. (n=27), Pseudomonas aeruginosa (n=18), Staphylococcus aureus (n=7), Proteus mirabilis (n=6), Acinetobacter baumannii (n=4), Providencia rettgeri (n=3), Pseudomonas sp. (n=3), Staphylococcus saprophyticus (n=3), Streptococcus sp. (n=3), Streptococcus agalactiae (n=2), Morganella morganii (n=2), Burkholderia cepacia (n=1), Citrobacter freundii (n=1), Enterobacter aerogenes (n=1), Enterobacter cloacae (n=1), Myroides odoratus (n=1) and Stenotrophomonas maltophilia (n=1).
ND, not determined; HA-UTI, hospital-acquired urinary tract infection; CA-UTI, community-acquired urinary tract infection.
Microbiologic characteristics and antibiotic susceptibility profile
The most common causative agent was E. coli (57.2%, 202/353) of both HA-UTIs and CA-UTIs, accounting for 36% (44/122) and 68% (158/231), respectively. The rest of the causal agents are shown in Figure 2. A greater variety of causative agents was observed in the HA-UTIs.
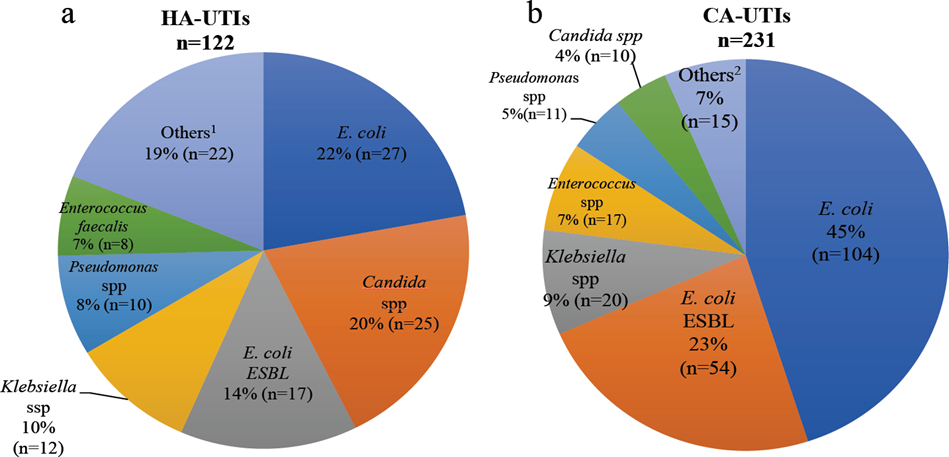
1 Staphylococcus spp, Enterobacter spp, Providencia rettgeri, Burkholderia cepacia, Citrobacter freundii, Myroides odoratus, Stenotrophomonas maltophilia, Acinetobacter baumanii, Proteus mirabilis, Streptococcus spp. odoratus, Stenotrophomonas maltophilia, Acinetobacter baumanii, Proteus mirabilis, Streptococcus spp.
2 Morganella morgagni, Proteus mirabilis, Enterobacter spp, Providencia rettgeri, Streptococcus spp, Staphylococcus spp. HA-UTIs: hospital-acquired urinary tract infections; CA-UTIs: community-acquired urinary tract infections.
Figure 2 Uropathogenic agents of HA-UTIs (a) and CA-UTIs (b) from 353 positive urine cultures
Antibiotic susceptibility patterns are described in Figure 3. The drugs with a high resistance rate (>50%) were amoxicillin-clavulanate (77%), fosfomycin (62%), ciprofloxacin (60%), trimethoprim-sulfamethoxazole (59%), levofloxacin (56%), and aztreonam (52%). Amikacin (1%), ertapenem (3%), colistin (4%), and nitrofurantoin (8%) were the antibiotics that presented the lowest resistance (<10%). Moderate resistance (10-50%) was observed with gentamicin (37%) and ceftriaxone (48%).
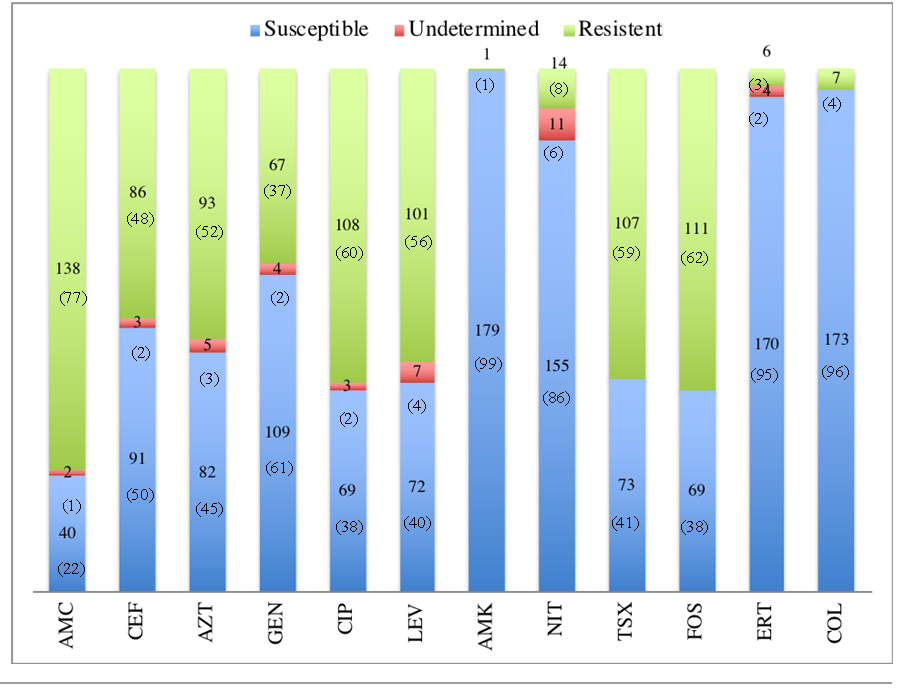
AMC=Amoxicillin-clavulanate, CEF=Ceftriaxone, AZT=Aztreonam, GEN=Gentamicin, CIP=Ciprofloxacin, LEV=Levofloxacin, AMK=Amikacin, NIT=Nitrofurantoin, TSX=Trimethoprim/Sulfamethoxazole, FOS=Fosfomicin, ERT=Ertapenem, COL=Colistin
Figure 3 Escherichia coli susceptibility pattern in UTIs by the plate microdilution method from 180 samples [n (%)].
Risk factors associated with ESBL-positive UTIs
ESBL-producing E. coli and Klebsiella spp. were detected in 21.5% of all UTIs (n=76); 76.3% (n=58) were CA-UTIs and 23.7% (n=18) were HA-UTIs. Infection by ESBL-producing Enterobacteriaceae was more frequent in patients with complicated UTIs (OR=3.65, 95% CI=1.69-7.90, p=0.001), previous use of antibiotics (OR=2.71, 95% CI=1.54-4.77, p<0.001), type 2 diabetes (OR=1.93, 95% CI=1.09-3.41, p=0.023), any immunodeficiency (OR=3.84, 95% CI=1.34-11.00, p=0.008), and radiochemotherapy (OR=5.49, 95% CI=1.04-29.00, p=0.025) (Table 2). Older patients (age ≥ 60 years) (OR=1.17, 95% CI=1.03-1.78, p=0.013) and patients with the presence of a catheter (OR=2.51, 95% CI=0.83-7.61, p=0.049) had a higher risk for acquiring an UTI caused by ESBL-producing Enterobacteriaceae in the community (data not shown).
Table 2 Demographic and clinical data of patients, according to ESBL production.
| Characteristic | Total (n=353) | ESBL (n=76, 32.5%) | non-ESBL (n=158, 67.5%) | P value | OR (95% IC) |
|---|---|---|---|---|---|
| Species | |||||
| E. coli | 202 (57.2) | 71 (35.1) | 131 (64.9) | ND | ND |
| Klebsiella spp. | 32 (9.1) | 5 (15.6) | 27 (84.4) | ND | ND |
| Demographics | |||||
| Male | 74 (21.0) | 29 (39.2) | 45 (60.8) | 0.136 | 0.65 (0.36-1.15) |
| Age ≥ 60 years | 89 (25.2) | 27 (30.3) | 62 (69.7) | 0.584 | 0.85 (0.48-1.51) |
| UTI type | |||||
| Hospital-acquired | 56 (15.9) | 18 (32.1) | 38 (67.9) | 0.951 | 0.98 (0.52-1.86) |
| Complicated | 173 (49.0) | 67 (38.7) | 106 (61.3) | 0.001 | 3.65 (1.69-7.90) |
| Underlying factors | |||||
| Previous use of antibiotics | 86 (24.4) | 40 (46.5) | 46 (53.5) | <0.001 | 2.71 (1.54-4.77) |
| Type 2 diabetes | 78 (22.1) | 33 (42.3) | 45 (57.7) | 0.023 | 1.93 (1.09-3.41) |
| Arterial hypertension | 48 (13.6) | 18 (37.5) | 30 (62.5) | 0.405 | 1.32 (0.68-2.57) |
| Chronic renal disease | 40 (11.3) | 16 (40.0) | 24 (60.0) | 0.265 | 1.49 (0.74-3.00) |
| Pregnancy | 20 (5.7) | 4 (20.0) | 16 (80.0) | 0.213 | 0.49 (0.16-1.53) |
| Immunodeficiency | 16 (4.5) | 10 (62.5) | 6 (37.5) | 0.008 | 3.84 (1.34-11.00) |
| Urologic alterations | |||||
| Recurrent UTI | 81 (22.9) | 27 (33.3) | 54 (66.7) | 0.839 | 1.06 (0.60-1.88) |
| Catheter | 58 (16.4) | 22 (37.9) | 36 (62.1) | 0.307 | 1.38 (0.74-2.57) |
| Urosepsis | 32 (9.1) | 9 (28.1) | 23 (71.9) | 0.320 | 0.79 (0.35-1.80) |
| Obstructive uropathy | 29 (8.2) | 8 (27.6) | 21 (72.4) | 0.548 | 0.77 (0.32-1.82) |
| Urologic surgery | 23 (6.5) | 10 (43.5) | 13 (56.5) | 0.236 | 1.69 (0.71-4.05) |
| Lithiasis | 20 (5.7) | 6 (30.0) | 14 (70.0) | 0.805 | 0.88 (0.33-2.39) |
| Benign prostatic hyperplasia | 19 (5.4) | 4 (21.1) | 15 (78.9) | 0.267 | 0.53 (0.17-1.65) |
| Tumor | 15 (4.2) | 7 (46.7) | 8 (53.3) | 0.225 | 1.90 (0.66-5.46) |
| Neurogenic bladder | 13 (3.7) | 4 (30.8) | 9 (69.2) | 0.892 | 0.92 (0.27-3.09) |
| Radiotherapy and/or chemotherapy | 7 (2.0) | 5 (71.4) | 2 (28.6) | 0.025 | 5.49 (1.04-29.00) |
ESBL, extended spectrum beta-lactamase; OR, odds ratio; UTI, urinary tract infection; ND, not determined.
Discussion
In the present study, we evaluated the epidemiologic characteristics of ESBL-producing agents in UTIs, acquired either in the hospital or the community, in patients at a tertiary care hospital. One-fifth of the UTIs were caused by ESBL-producing strains (21.5%), which is a higher incidence of ESBL-producing agents in UTIs, compared with the results of other published studies.11,13,16,17 Nevertheless, previous studies in Mexico have reported alarmingly high incidences of UTIs caused by ESBL-producing E. coli in the community (56.5%) and in complicated infections (59.8%).18,19 Infections caused by ESBL-producing bacteria were more frequent in the community than in our hospital setting (76.3% and 23.7%, respectively). Indeed, ESBL-producing enterobacteria have been reported to cause up to 41% of CA-UTIs and up to 26% of HA-UTIs.13,17,20,21 A notable increase in CA-UTIs caused by ESBL-producing E. coli was reported in Spain, from 50% in 2000 to 79% in 2003 (p < 0.001).11 The majority of UTIs detected in our study were CA infections (65.5%). E. coli was the most frequent causative agent, both in HA-UTIs and CA-UTIs, although it was more frequently detected in CA infections (p<0.001). The variety of causative agents of HA-UTIs was more diverse than those acquired in the community, as previously reported.7
Multiple studies have reported male sex,13,20,21 advanced age (> 65 years),20,21 previous hospitalization,13,20-23 previous antibiotic therapy,20-23 recurrent UTIs,13,22 urinary catheterization,23 diabetes,13 lithiasis, and immunosuppression as risk factors for ESBL-producing Enterobacteriaceae infections.17 In our study, complicated UTIs (p=0.001), previous antibiotic therapy administration (p<0.001), type 2 diabetes (p=0.023), any immunodeficiency (p=0.008), and radiotherapy and/or chemotherapy (p=0.025) were risk factors for infections by the ESBL-producers, E. coli or Klebsiella spp.
Gram-negative uropathogens are increasingly becoming resistant to currently available antibiotics, including aminoglycosides, sulfonamides and fluoroquinolones.(1, 8, 9) In our study, E. coli isolates exhibited high resistance to amoxicillin-clavulanic acid, and moderate resistance to gentamicin, aztreonam, and ceftriaxone. Interestingly, resistance levels to ciprofloxacin (complicated UTIs, 64.4% vs. uncomplicated UTIs, 46.7%), levofloxacin (complicated UTIs, 62.2% vs. uncomplicated UTIs, 37.8%), fosfomycin (complicated UTIs, 60.7% vs. uncomplicated UTIs, 64.4%), and trimethoprim-sulfamethoxazole (complicated UTIs, 59.3% vs. uncomplicated UTIs, 60.0%) were high. However, the Infectious Diseases Society of America (IDSA) guidelines for the treatment of uncomplicated UTIs recommend the administration of nitrofurantoin, trimethoprim/sulfamethoxazole, fosfomycin, and fluoroquinolones.24 Therefore, international guidelines seem to be inappropriate in our setting, which limits our therapeutic options.
Even though low resistance rates of uropathogens to fosfomycin are still being reported worldwide,25 decreasing susceptibility of ESBL-producing E. coli to fosfomycin has been described and limited data has been reported in Latin American countries.26,27 In addition, as part of the SENTRY Antimicrobial Surveillance Program, bacteria isolated from patients with CA-UTIs in Latin America showed surprisingly high resistance rates to orally administered antimicrobials, especially for trimethoprim/sulfamethoxazole and fluoroquinolones.28 Those results highlight the need for specific CA-UTI guidelines, based on local susceptibility patterns in geographic regions where elevated antimicrobial resistance may influence prescribing decisions. This situation requires intervention both in the community and in the hospital setting: government regulation strategies are required to minimize the use of antibiotics without a medical prescription and control pharmaceutical industry propaganda and the self-regulation on the part of health professionals,29 to avoid the unnecessary use of new antibiotics. Within the hospital setting, the surveillance of the prescription of antibiotics to both outpatients and inpatients should also be implemented.
Complicated UTIs caused by E. coli exhibited higher resistance to several antimicrobial agents, including gentamicin (p=0.042), aztreonam (p=0.028), ceftriaxone (p=0.035), ciprofloxacin (p=0.041), and levofloxacin (p<0.001). A high percentage of ertapenem, colistin, amikacin, and nitrofurantoin susceptibility was found in our study (100%, 100%, 99.4%, and 92.2%, respectively). The use of those antibiotics is a good option for the empiric treatment of UTIs in the Mexican population.24
Our study has several limitations. The clonal relationship of isolates, especially of E. coli, was not analyzed. Therefore, we could not establish whether there was a high level of genetic diversity between the isolates or whether independent acquisition or cross-transmission occurred. Given the unusually high resistance to fosfomycin detected in the E. coli isolates, further analyses should be performed to characterize those strains and the mechanism of resistance, e.g. the search for fosfomycin-associated genes.
Conclusion
The emergence of ESBL-producing bacteria in UTIs is a serious health problem, in both our community and our hospital settings. Approximately one out of every five UTIs was caused by ESBLs in our study population. An alarmingly high resistance to antibiotics recommended as first-line empiric therapy in UTIs (fosfomycin, fluoroquinolones, and trimethoprim-sulfamethoxazole) was recognized. Consequently, international guidelines are not suitable for our population, limiting our therapeutic options. The results of our study highlight the need for developing specific guidelines, based on our local susceptibility patterns in geographic regions where elevated antimicrobial resistance may influence therapeutic decisions.











 nueva página del texto (beta)
nueva página del texto (beta)



