TAKE-HOME MESSAGES
Penile Doppler ultrasound is one of five specialized diagnostic tests for erectile dysfunction, grade B recommendation.
Patients that undergo surgery can expect to experience significant postoperative changes, and erection is one of the most important health-related quality of life outcomes.
Current evidence does not support the systematic use of penile Doppler ultrasound, but it must be included in the management algorithm of the patient undergoing radical prostate surgery for the proper evaluation of erectile function.
INTRODUCTION
Changes in sexual function after radical prostatectomy in patients with prostate cancer are unpredictable and impossible to avoid.1,2 Patients who undergo surgery (open, laparoscopic, or robotic) can expect to experience significant changes post-surgery, and erection is one of the most important health-related quality of life outcomes influencing patient choice of treatment and post-surgery satisfaction. Numerous articles have been published in the literature on post-radical treatments, but inexplicably there is little information on diagnostic options. Penile Doppler ultrasound is a common method for diagnosing erectile dysfunction. The response to intracorporeal injections of vasoactive substances during that procedure is useful in the evaluation of arterial and venous-occlusive function.3,4 Sexual rehabilitation after radical prostatectomy requires a complex process in which the diagnosis is refined and an accurate treatment program is chosen. 5 Sexual function, mainly erectile dysfunction, after radical prostatectomy, is an obvious challenge for the urologist.6,7 Part I of the present review paper provides a comprehensive inventory of the available guidelines; Part II addresses the ítems that are necessary for performing an optimal ultrasound examination as part of the complex process of post-radical prostatectomy erection recovery; and Part III is aimed at defining sharable recommendations.
EVIDENCE ACQUISITION
A literature search was conducted using Google and the National Library of Medicine’s PubMed databases to identify original and review articles, either published or e-published, on the uses of penile Doppler ultrasound in post-radical prostatectomy evaluation or post-surgery rehabilitation, up to February 2018. The search terms included: Erectile dysfunction post-radical prostatectomy, sexual function post radical prostatectomy, Penile evaluation post-prostatectomy, Diagnosis of erectile function after radical surgery, Penile Doppler ultrasound AND prostatectomy, Penile Doppler ultrasound AND sexual rehabilitation. The reference list of the articles retrieved, as well as relevant reviews, were also studied. The initial search produced 415 articles and, after applying additional filters, 46 studies were included in the present review.
BACKGROUND
The recommendations of the most relevant guidelines are cited with respect to the use of penile Doppler ultrasound after radical prostatectomy. Unfortunately, urologic guidelines are conflicted in terms of recommendations.8
Standard practice in sexual medicine (Seftel 2006): Penile Doppler ultrasound is an optional part of examination. There is no specifically mentioned post-radical prostate evaluation.9
Standard operating procedure (2013): Penile Doppler ultrasound is an objective and reliable diagnostic method for documenting penile hemodynamics. It requires skilled personnel and modern equipment that may be cost-prohibitive in certain settings. Objective vascular testing that provides a physiologic diagnosis may help direct appropriate therapy (Sikka, et al).10 Penile Doppler ultrasound is not mentioned in the chapter about preservation of erectile function outcomes after radical prostatectomy (Mulhall, et al.).11
International Consultation on Sexual Medicine (2015): Color duplex Doppler penile ultrasonography (CDDPU) is one of five specialized diagnostic tests for erectile dysfunction, grade B recommendation (Dennerstein, et al.),12 (Salonia, et al.).6 Diagnostic penile Doppler ultrasound is not specifically mentioned for post radical prostate evaluation (Incrocci, et al.).13
EAU guidelines (Hatzimouratidis et al., 2016):14 Erectile dysfunction is common after radical prostatectomy, irrespective of the surgical technique used. LE: 2B. Specific diagnostic tests should be included in the initial evaluation only in the presence of: primary erectile dysfunction; young patients with a history of pelvic or perineal trauma that could benefit from potentially curative revascularization surgery; patients with penile deformities that might require surgical correction; patients with complex psychiatric or psychosexual disorders; and patients with complex endocrine disorders. Specific tests may be indicated at the request of the patient or his partner, or for medicolegal reasons (e.g., implantation of penile prosthesis to document end-stage erectile dysfunction, sexual abuse). LE: 4B.
AUA Guidelines (Board of Directors 2012; 2017 reaffirmed): 15 The Consensus Statement on indications for a penile ultrasound examination include but are not limited to: evaluation of erectile dysfunction; evaluation of Peyronie’s disease; others. Penile Doppler ultrasound is not mentioned in the chapter about preservation of erectile function outcomes after radical prostatectomy.
PREOPERATIVE ULTRASOUND EVALUATION
The preoperative assessment of a candidate for radical prostatectomy is the first compulsory step in preventing postoperative ED. That recomendable attitude has been called "the good start".16 Patient factors (including age, baseline erectile function, personal antecedents, and status of comorbid conditions), evaluation of the clinical and pathologic characteristics of the prostate cancer (e.g., Gleason and NMR findings), nerve-sparing selection (unilateral vs bilateral nerve sparing), type of surgery (e.g., intrafascial vs interfascial vs extrafascial surgeries), surgical techniques (e.g., open, laparoscopic, and robotic-assisted radical prostatectomy), and surgeon factors (e.g., surgical volume and surgical skill). The evaluation of each of those items contributes to achieving a better long-term result and they are the key significant contributors to erectile function recovery.17 Penile shortening and/or deformities may appear or become aggravated after radical surgery. The patient should be informed of that potential side effect. 1 The literature reviewed does not support the recommendation of the systematic use of preoperative ultrasound evaluation with respect to radical prostate surgery, but there are at least three situations in which its performance is recommended:
The patient has a preoperative condition that justifies the evaluation with ultrasound. (e.g., Peyronie’s disease).
There is a risk of legal problems (e.g., related to the job or social position of the patient).
The patient claims to have excellent erections and you have doubts (e.g., due to advanced age or comorbidities).
POSTOPERATIVE ULTRASOUND EVALUATION
Penile evaluation
Nodules, plaques, penile shortening, and de novo deformities (hourglass and other), have been described after radical surgery.18 Although penile Doppler ultrasound enables the intracavernosal evaluation of each of those lesions, it is essential to first observe the penis in flaccidity and then in erection to describe the anatomic findings. An important component of this phase is to measure the penis in a flaccid state and then in erection. That first phase of external inspection and response to vasoactive medication has been called the 'erection test'. During that part of the examination, whoever performs it can make note of the different penile findings, unrelated to ultrasound, which can be very useful in the prognosis and treatment proposed post radical prostatectomy.
Arterial evaluation
Normal reference values during penile Doppler ultrasound are: Peak systolic velocity (PSV: 25 cm/ sec or more), End diastolic velocity (EDV: 5 cm/sec or less), Acceleration time (AT: 0.11 sec or less), and Resistance index (RI: 0.85 or more).19-21 Abnormal arterial findings after radical prostatectomy have two possible origins:
Abnormal findings prior to surgery: A less tan 75% increase in baseline cavernosal artery diameter, abnormal PSV (less than 25 cm/ sec), and AT (more than 0.11 sec), usually bilateral, are suggestive of arterial disease, but those findings could also be related to arteriosclerosis or other common arterial pathologies, prior to surgery. In some cases, congenital arterial malformations (aneurysms, fistulas) may be found, of which the patient was previously unaware, affecting his erectile recovery.
Abnormal findings after surgery: Penile Doppler ultrasound is a direct and indirect method for diagnosing vascular lesions acquired after radical prostatectomy. To decrease the risk of false positives, it is necessary to verify arterial flow at the perineal level, when penile flows are persistently low. In addition to measuring flow, the asymmetry between the arteries should be verified.
Venous evaluation
Veno-occlusive disease is suggested by abnormal EDV (more than 5 cm/ sec) and RI (less than 0.85). Regardless of the surgical technique, the removal of the prostate may result in an almost obligatory period of dormancy of the nerves that govern the functional aspects of erection. That situation may lead to a loss of daily and nocturnal erections associated with persistent failure of cavernous oxygenation and secondary erectile tissue damage resulting from the production of pro-apoptotic factors and pro-fibrotic factors within the corpora cavernosa.22,23 Those changes are coupled with postoperative erectile dysfunction of varying degrees and the development of venous leakage, which indicates a poor prognosis for erectile function recovery.24,25
Venous leakage was first described in the nineteenth century (Raymond and Duncan, 1895)26,27 and more than one hundred years later, venous leakage diagnosis still needs to mature, even though it is key to the functioning of the penis as a three-chamber pump. Trost et al.28 mention the difficulty of finding relevant literature about venous surgery and how data analyses cannot be carried out due to the lack of standardization in patient selection, hemodynamic testing, surgical technique, follow-up, and surgical outcome. The text mentions the articles of Florez and Mulhall (2011),29Cayan (2008),30 and Rao and Donatucci (2001),31 with their respective and highly variable results. Other theories and surgical techniques for venous leakage have been proposed by the Korean urologist GL Hsu (2006, 2010).32-34 Despite the heterogeneity in the data, there is sufficient clinical evidence supporting ultrasound evaluation, even though venous leaks acquired post fibrosis are considered part of the physiopathology of post-radical prostate erectile dysfunction and are mentioned by different authors in their algorithms. Perhaps the best known is that described by Hatzimouratidis,35 presented below (Figure 1):
The incidence of venous leakage increases in proportion to the time interval after surgery, supporting those pathophysiologic mechanisms as the cause of disturbance and providing the rationale for early penile rehabilitation before penile fibrosis occurs. Penile Doppler ultrasound can identify two different types of venous leakage:
Previous leaks: usually congenital, that make the erectile recovery of the patient after radical prostatectomy difficult.
Acquired leaks: intracavernous leaks, usually associated with areas of cavernous fibrosis. They are the most frequent type after radical prostatectomy.
Fascial and cavernous tissue evaluation
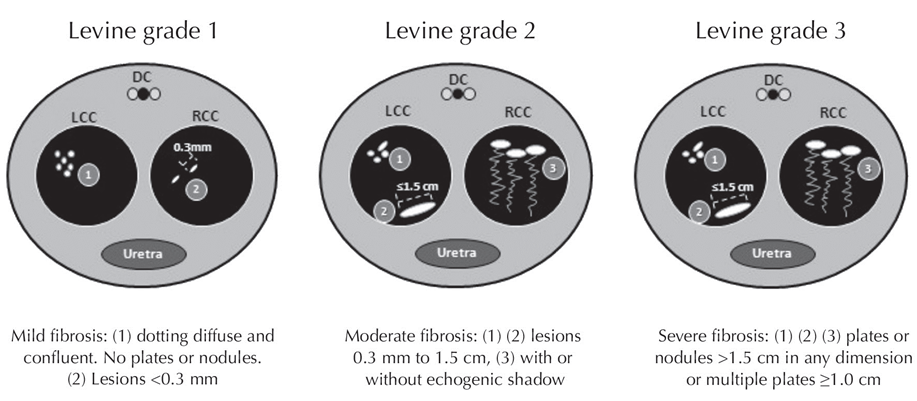
The evaluation of the fascia and the cavernous tissue after radical surgery is fundamental due to the concepts of the venous leakage/fibrosis relationship previously expressed36,37 and because there may be a peak in the prevalence of Peyronie's disease post radical prostatectomy. That pathology includes a variety of states of severe penile fibrosis that compromise the tunica albuginea, but they, alone, do not cover the wide range of other types of penile fibrosis.38-41 To clarify the panorama of what post-radical prostatectomy Penile Doppler ultrasound can find in the intracavernous tissue, it is necessary to consider another fibrous pathology called Chronic Traumatic Cavernosophaty (CTC), which, unlike Peyronie’s disease, does not compromiso the tunica albuginea.I,42-46 An echographic classification grade of calcification was published by Laurence Levine47,48 and revised in Campbell’s Urology 11th ed. (2016).49 Calcification areas were defined as hyperechoic regions with the presence of acoustic shadows using Levine’s three echographic grades: Grade 3 (plates > 1.5 cm in any dimensión or multiple plates ≥1.0 cm); Grade 2 (lesions 0.3 mm to 1.5 cm); and Grade 1 (lesions <0.3 mm). In accordance with the Levine classification, Grade 1 is mild, Grade 2 is moderate, and Grade 3 is severe) (Figure 2).50 Other classifications have been used according to ultrasonographic patterns: a formed, solitary, hyperechoic lesion with no acoustic shadow (group A), moderately hyperechoic multiple scattered calcified lesions with acoustic shadows (group B), dense calcified hyperechoic plaque with acoustic shadow (group C).51
Neurologic evaluation
Penile erection is a neurovascular event requiring intact neural and vascular pathways. Most surgeries are supposed “nerve-sparing” surgeries. That type of surgery spares the cavernous nerves that run bilaterally along the prostate. Despite nerve-sparing surgery, the cavernous nerves are stretched and bruised intraoperatively and may take 18 to 24 months post-surgery to heal. Men may fail to have natural erections during that period of time, which can lead to penile tissue atrophy, fibrosis, structural alterations, and venous leak, as cited above.52 Penile Doppler ultrasound is not the appropriate test for evaluating neurologic status after radical surgery.6 However, it is possible to obtain indirect data of potential damage to the neurovascular bundle. A finding that should always be included in the report is the appearance of acute pain in the suprapubic region, after the use of a vasoactive drug related to severe damage of the unilateral or bilateral neurovascular bundle.
COST ANALYSIS
The greater reluctance to including penile Doppler ultrasound as a routine item in the postoperative evaluation protocol of radical prostatectomy patients is the increase in cost, together with the assumption of few benefits from its systematic use. The cost of treatment of radical prostatectomy-related erectile dysfunction can be projected to increase but, compared with the technology used to manage prostate cancer (Robotics, PET scan, etc.), the cost of penile Doppler ultrasound is actually modest.
RECOMMENDATIONS
— Use the appropriate ultrasound equipment (the correct transducer, and ideally, HD resolution).
— Select the appropriate patient.
— Complete all the steps: Penile, arterial, venous and tissue evaluation.
— Use a classification to report penile fibrosis (we recommend the Levine classification).
— If you are an expert in penile Doppler ultrasound and receive patients from other colleagues: give a thorough report and provide generous recommendations.
CONCLUSIONS
Sexual rehabilitation after radical prostatectomy requires a complex process. There is great inconsistency in the literature as to the definition of what is considered normal erectile function before surgery and what a man may consider normal erection after radical prostatectomy. One possibility is to use validated psychometric instruments with recognized cutoff points for normalcy and severity during the preoperative and postoperative evaluations.17 Although there is no consensus, our analysis confirmed that penile Doppler ultrasound after radical prostatectomy can be a diagnostic alternative. Current evidence does not support the systematic use of penile Doppler ultrasound, but it must be included in the management algorithm of the patient undergoing radical prostate surgery for the proper evaluation of erectile function. Further studies with adequate follow-up and larger samples should be conducted to reach a comprehensive conclusion.53











 nueva página del texto (beta)
nueva página del texto (beta)