INTRODUCTION
Most testicular lesions are currently diagnosed at earlier clinical stages and the detection of incidental focal lesions has increased due to the widespread use of testicular ultrasound imaging. [1]. Benign pathology is found in up to 10-20% of testicular tumors[2]. Recent studies have shown that testicular frozen section examination (FSE) is a useful and reliable method for evaluating testicular lesions of uncertain origin. [3, 4]. The finding of benign pathology through FSE can prevent unnecessary radical orchiectomy and its associated complications. Despite the recent evidence, this procedure continues to be underperformed.
The aim of our study was to retrospectively review our experience in the performance of testicular FSE in lesions of uncertain origin and its diagnostic accuracy.
OBJECTIVE
To evaluate the diagnostic accuracy of FSE in equivocal malignant testicular masses (EMTMs), as well as its associated short and long-term complications.
MATERIALS AND METHODS
Study design
A retrospective study was conducted within the time frame of 2005 to 2015 at the Instituto Nacional de Ciencias Médicas y Nutrición “Salvador Zubirán” in Mexico City. The study was approved by our institutional ethics committee, based on the Helsinki Declaration. The study design was carried out following the STARD (Standards for Reporting of Diagnostic Accuracy) recommendations [5].
Participants
Selection criteria: patients ≥ 18 years of age that underwent FSE in EMTMs. EMTMs were defined as palpable or incidentally-identified testicular lesions, accompanied by systemic or genitourinary comorbidities that could suggest a benign etiology, with normal levels of serum tumor markers and no evidence of metastatic disease. Potential participant data were obtained from the surgery database of the Urology Department. The patients included in the study were those that had undergone testicular exploration with FSE within the time frame of 2005 and 2015. Paratesticular FSE was excluded from the analysis.
We collected the demographic variables, comorbidities, signs and symptoms, presence of preoperative testis atrophy, laterality, ultrasound characteristics (color Doppler enhancement, diameter, and echo-structure), serum tumor marker levels, short and long-term complications according to the Clavien-Dindo classification, and later malignant development in patients with a benign histology report.
Diagnostic Method
The index test was the FSE in EMTMs and the reference standard was the definitive histopathologic report or radical orchiectomy specimen analyzed at the Pathology Department.
The FSE and definitive histopathology reports were classified as benign lesions (infection, benign tumors, atrophy, inflammation and/or normal tissue) or malignant lesions (seminomatous germ-cell tumor, non-seminomatous germ-cell tumors, lymphoproliferative diseases, or other malignant neoplasia). The FSE result was available to the pathologist that provided the definitive histopathology result.
Surgical technique
Testicular exploration was performed through inguinal incision. The spermatic cord was clamped with a vessel loop and cold ischemia of the testis was performed. Once the tunica vaginalis was opened and the EMTM was exposed, incisional or excisional biopsy was carried out, according to tumor location and size. If malignancy was reported in the FSE, a radical orchiectomy was performed.
FSE technique
In the Pathology Department a fresh sample was received and then embedded in a compound for cryosectioning (Tissue-Tek ® O.C.T.), to provide a matrix, freezing the tissue after its placement in the Cryostat microtome (< - 35°C). Once the sample was frozen, it was sectioned into slices of 3-4 micrometers and stained with hematoxylin and eosin for light microscopic analysis. A standard paraffin-embedded analysis was then performed, and all samples were stained with hematoxylin and eosin for the definitive diagnosis.
Statistical analysis
The descriptive analysis was reported through mean and standard deviation (SD). Medians were described through interquartile range or proportion, based on data type and distribution. The categorical variables were compared using the X2 test or Fisher’s exact test and parametric and nonparametric tests were used for the continuous variables.
Sensitivity, specificity, negative predictive value (NPV), and positive predictive value (PPV) were calculated to evaluate FSE accuracy, using the definitive histopathology report as the gold standard. We calculated the degree of concordance between malignant FSE reports and malignant definitive histopathology reports using Cohen’s Kappa coefficient. Statistical significance was set at a p < 0.05. All reported p values were two-sided. The statistical analyses were performed using the IBM SPSS Statistics version 22 program.
RESULTS
Population characteristics
Twenty-six patients underwent FSE, 3 of whom were excluded due to paratesticular lesion, leaving a total of 23 patients in the study. Mean patient age at disease presentation was 37 years (SD: 13) with a median follow-up period of 10 months (IQR: 60 months). The main comorbidities reported were diabetes mellitus in 4 patients (17.3%), HIV infection in 2 (8.6%), systemic lupus erythematosus in 3 (13%), systemic hypertension in 2 (8.6%), and tuberculosis in 1 (4.3%) patient. The clinical characteristics and ultrasound findings are described in Tables 1and2.
Table 1 Clinical characteristics of the patients with equivocal malignant testicular masses.
| Clinical characteristics | Total | Definitive malignant | Definitive benign | P |
|---|---|---|---|---|
| Palpable mass - n (%) | 13 (56) | 4 | 9 | 0.6 |
| Pain - n (%) | 10 (43.5) | 2 | 8 | 0.6 |
| Testicular atrophy - n (%) | 5 (21.7) | 2 | 3 | 1.0 |
| Fever - n (%) | 2 (8.6) | 0 | 2 | 1.0 |
| Weight loss- n (%) | 1 (4.3) | 0 | 1 | 1.0 |
| Fatigue - n (%) | 1 (4.3) | 1 | 0 | 1.0 |
Table 2 Ultrasound characteristics of the equivocal malignant testicular masses.
| Ultrasound characteristics | Total | Definitive malignant | Definitive benign |
|---|---|---|---|
| Echo structure - n (%) | |||
| Hypoechoic | 6 | 3 | 3 |
| Normal | 3 | 1 | 2 |
| Hyperechoic | 1 | 0 | 1 |
| Anechoic | 1 | 0 | 1 |
| Heterogeneous | 10 | 2 | 8 |
| Not reported | 2 | - | - |
| Diameter - mean (SD)* | 2.3 (2.04) | 2.0 (1.4) | 2.4 (2.2) |
| Enhancement with color Doppler - n (%) | 5 (21.7) | 1 (4.3) | 4 (17.3) |
*Diameter not reported in 7 cases.
Surgical treatment and complications
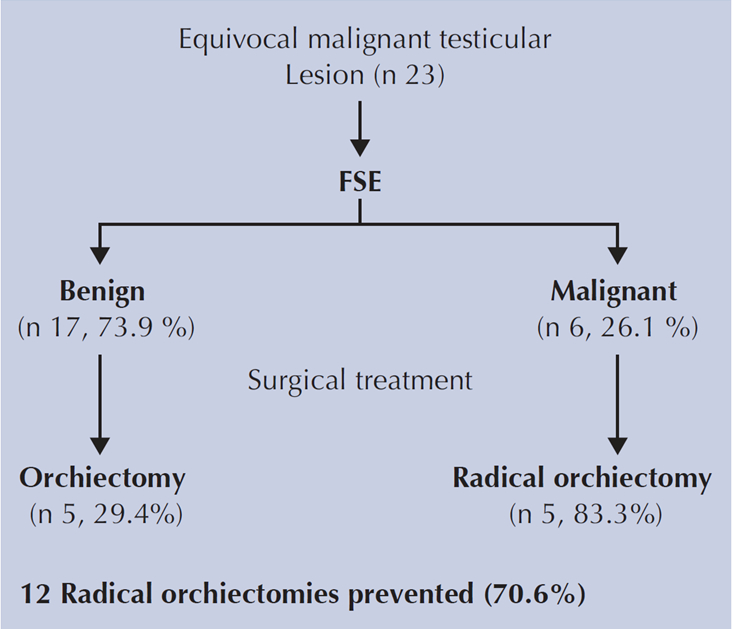
For the FSE, 17 (73.9%) excisional biopsies and 6 (26.1%) incisional biopsies were performed. Malignancy through FSE was reported in six cases (26.1%), (Figure 1). The definitive histology reports are summarized in Table 3.
Table 3 Definitive histopathology reports of EMTM.
| Definitive histopathology reports | n (%) | |
|---|---|---|
| Benign Lesions | ||
| Normal tissue | 1 (4.3) | |
| Tuberculosis | 1 (4.3) | |
| Vasculitis | 2 (8.7) | |
| Nodular Leydig cell hyperplasia | 2 (8.7) | |
| Serous cystadenoma | 1 (4.3) | |
| Chronic orchitis | 1 (4.3) | |
| Adenomatoid tumor | 2 (8.7) | |
| Atrophy | 4 (17.4) | |
| Old infarction | 1 (4.3) | |
| Obstruction | 1 (4.3) | |
| Necrosis | 1 (4.3) | |
| Total | 17 (73.9) | |
| Malignant Lesions | ||
| Seminomatous germ cell tumor | 3 (13) | |
| Lymphoma | 2 (8.7) | |
| Non-Seminomatous germ cell tumor | 1 (4.3) | |
| Total | 6 (26.1) | |
In total, 10 radical orchiectomies were performed (43.5%). Of the 6 malignant FSE reports, 5 of those patients (83%) underwent radical orchiectomy and 1 patient with lymphoma did not. In addition, 5 patients with a benign FSE report (29.4%) underwent orchiectomy due to chronic orchitis associated with syphilis (n = 1), fibrosis and ischemia (n = 2), extensive necrosis (n = 1), and an adenomatoid tumor with associated ischemia (n = 1). Radical orchiectomy was performed in those patients because of the greatly compromised testicular condition. A total of 12 radical orchiectomies (70.6%) were prevented, as a result of the benign FSE report.
Regarding the early complications of FSE, 3 patients (12.5%) had grade I complications (two hematomas and one seroma). No patients presented with grade II complications, or higher. In the long term, 2 patients presented with testicular atrophy.
There were no malignant formations during follow-up (median: 9 months) in any of the patients that did not undergo radical orchiectomy as a result of the benign FSE report.
FSE diagnostic value
There were no diagnostic changes made in relation to the FSE reports and the definitive pathology reports. Table 4 summarizes the sensitivity, specificity, and predictive values of FSE for malignant lesions. The degree of concordance between the FSE reports and the definitive malignant reports was statistically significant (κ = 1.0, p < 0.05).
DISCUSSION
Radical orchiectomy is the standard treatment for a suspicious malignant lesion, but testis-sparing surgery (TSS) can be an alternative approach for benign lesions. FSE could help identify those patients suitable for TSS. In our study, FSE demonstrated high sensitivity and specificity. Our findings were similar to those reported in previous series [1, 4]. In 2006, Connolly et al. described a PPV, NPV, sensitivity, and specificity of 94.2, 92.6, 96.1, and 89.3%, respectively[6]. Table 5summarizes the testicular FSE diagnostic accuracy found in different studies. Complete concordance between the FSE and definitive pathology reports for malignant lesions was found in the present analysis, similar to that of other studies with reported kappa values of 0.76 to 1[3, 7].
Table 5 FSE diagnostic accuracy results from different studies evaluating testicular masses.
| Authors, Publication year | N | Benign / Malignant (%) | Sn | Sp | PPV | NPV |
|---|---|---|---|---|---|---|
| Elert et al. [2], 2002 | 354 | 10.5 / 89.5 | 100 | 100 | 100 | 100 |
| Leroy et al.[8], 2003 | 15 | 73.3 / 26.6 | 100 | 100 | 100 | 100 |
| Connolly et al.[9], 2006 | 80 | 35 / 65 | 96.1 | 89.3 | 94.2 | 92.6 |
| Subik et al.[10], 2012 | 45 | 57.7 / 42.2 | 100 | 95 | 96 | 100 |
| Silverio et al.[11], 2015* | 159 | 23.8 / 76.1 | 95 | 100 | 95 | 100 |
| Matei et al.[3], 2017 | 144 | 43.1/ 52.1 | 93 | 98 | 99 | 91 |
| Current study, 2018 | 23 | 73.9 / 26.1 | 100 | 100 | 100 | 100 |
Sn, Sensitivity; Sp, Specificity; PPV, Positive Predictive Value; NPV, Negative Predictive Value.
*Sn, Sp, PPV, NPV are calculated including 11 paratesticular lesions
In our study, 26.1% of the EMTMs were malignant, whereas other authors report frequencies of 0% to 89.5% [2, 6, 12, 13]. No false negative results were seen in the present study. In 2015, Silverio et al. described a 3.5% tumor identification failure rate; of 6 false negatives, 3 were due to an inadequate sample and the other 3 were most likely associated with small tumor size, frozen section artifacts, or pathologist experience [11]. Even though our institution does not have a specialized uropathologist, FSE reliability was high, lending support to its regular use at other centers in similar situations.
Radical orchiectomy was not performed on most of our patients with benign pathology (70.6%), which was similar to the results of other series, in which 74.5 to 88.2% of patients did not require radical surgery because of benign results [10, 11]. Nevertheless, orchiectomy can be necessary in benign lesions when there are conditions of total testicular necrosis, testicular atrophy, questionable viability, extended lesions with significant testicular destruction, or non-functional testis.
We found no significant associations between clinical or ultrasound characteristics and a malignant FSE report. In other series, malignant lesions were associated with greater tumor size [3, 6, 10]. The ultrasound finding of a low-volume testicular lesion can suggest the difference between benign and malignant lesions, but diagnostic accuracy is low [14, 15].
The complication rate in our study was 12.5% and all were Clavien-Dindo grade I complications. To the best of our knowledge, the present study is the first to use the Clavien-Dindo classification for complications of testicular FSE. A few studies have reported complication rates in patients with benign pathology that vary from no complications [6] up to 8.1% for testicular atrophy and hematomas and 2.7% for orchitis/epididymitis [2].
No malignant neoformations were observed during follow-up in our patients that had a benign FSE report. Similar findings are reported in other studies, in which no malignancy development was seen at mean follow-up times of 77.8 months and 105 months [2, 6].
Limitations of our study include its retrospective design, data taken from a single center, and the small number of patients. However, FSE in EMTMs appears to be a useful tool for clinical practice, with excellent diagnostic accuracy and a low probability of complications. FSE can potentially prevent unnecessary radical orchiectomies in selected patients.











 nueva página del texto (beta)
nueva página del texto (beta)