Introduction
Since the publication of the Diagnostic and statistical manual of mental disorders DSM-5 (5ed.; DSM-5; American Psychiatric Association, 2013), those known as feeding and eating disorders have undergone important modifications. One of these is that feeding disorder of infancy or early childhood is replaced by avoidant/restrictive food intake disorder (ARFID). However, since this modification, the disorder has gained relevance, for instance, the PubMed database from 2013 to 2020 have increased the number of published articles from six to 232, while in the PsyInfo database there were two articles published in 2013, and in 2020 were 135.
ARFID is mainly characterized by food restriction, however, it has some qualities that make it a disorder with a complex clinical presentation, for this reason, some authors (Bryant-Waugh, et al. 2010) mention that three subtypes converge within it: 1) lack of interest in eating, 2) fear of the aversive consequences of eating, such as vomiting or choking and 3) the sensitive type where food is avoided because of its organoleptic characteristics. Suffering this disorder brings important consequences such as: significant loss of body weight, nutritional deficiency, dependence on nutritional supplements or enteral feeding, deterioration in psychosocial functioning and in the case of children, growth impairment according to their age (5ed.; DSM-5; American Psychiatric Association, 2013).
Its incidence in children and adolescents is known to be 8.4% (Cooney et al., 2018), its prevalence is estimated to range from 5% to 22.5% (Fisher et al., 2014; Nicely et al., 2014; Norris et al., 2014)using a diagnostic algorithm, compared all cases with ARFID presenting to seven adolescent-medicine eating disorder programs in 2010 to a randomly selected sample with anorexia nervosa (AN, and concerning its comorbidity, the disorders with which it is most associated are anxiety disorders, autism spectrum disorder, and attention deficit hyperactivity disorder (ADHD; Kambanis et, al., 2019). However, these data are preliminary because of their recent study.
As for its etiology there is little data, according to Brigham, et al. (2018), this disorder may be due to biological factors such as sensory sensitivity, anxiety state, and the presence of low homeostatic and hedonic appetite. Also, they point out that it could be associated with environmental factors such as family patterns in meals, availability of fruits or vegetables, and exposure to healthy eating patterns.
Regarding it treatment, clinical interventions have mainly been reported in case studies, which shows the need for more studies in the area, in addition analyzing the significance of the data already reported. Case studies are important for decision-making when no studies are available with high standard levels of evidence (Murad, et al. 2018). In addition, provide information regard symptomatology of a little-known pathology and a novel approach to clinical treatment, pointing out the benefits or harmful effects of interventions (Vanderbroucke, 2001), and finally they are a didactic guide when combining research and clinical practice (Roussos, 2007).
In pathologies like ARFID, case studies are valuable, because provide a detailed procedure of interventions, as well as abundant data on patient’s clinical characteristics. Case studies published under the Case Report (CARE) guidelines are relevant because capture useful clinical information with high quality and strict methodology (Riley, et al. 2017). Therefore, the aim of this study was to analyze clinical characteristics and clinical interventions reported in case reports and case series studies of avoidant/ restrictive food intake disorder (ARFID) from a systematic review of the literature.
Method
The review was performed according to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA; Moher, Liberati, Tetzlaff & Altman, 2009). The search was conducted from March 30th, 2020 to September 29th, 2021, through PubMed and PsycINFO databases, these were chosen because are specialized in health and behavioral sciences respectively. The MeSH terms used were: <<ARFID>>, <<avoidant restrictive food intake disorder>> and <<case report>> in combination with the AND boolean term. Another search was also performed through the Scielo database with the MeSH terms <<Trastorno de evitación/restricción de la ingesta de alimento>> and <<Avoidant restrictive food intake disorder>>. It should be noted that the MeSH terms <<reporte caso>> or <<case report>> were not added because this way no results were obtained (see Table 1).
Table 1 Search criteria and articles obtained
| Data base | Search area | Search terms | Limits | Results |
|---|---|---|---|---|
| PubMed | All fields | “ARFID” AND “avoidant restrictive food intake disorder” AND “case report” | 2012-2021 | 53 |
| PsycINFO | All fields | “ARFID” AND “avoidant restrictive food intake disorder” AND “case report” | 2012- Current | 278 |
| Scielo | All fields | “Trastorno de evitación/restricción de la ingesta de alimentos” | Unlimited | 1 |
| “Avoidant/restrictive food intake disorder” | Unlimited | 4 |
Eligibility criteria
We only include a) case reports or case series studies, b) published from 2012 to 2020, c) in English or Spanish language. We exclude a) theoretical articles and reviews, b) empirical studies, book or encyclopedia chapters, lecture or poster summaries, thesis dissertation, commentaries and letters to the editor, c) articles that address topics such as orthorexia, selective feeding, other FEED, emetophobia, neophobia, functional dysphagia, emotional disorder of food avoidance and articles that discuss changes in DSM-5 diagnostic criteria.
Analysis of Results
As it proposed Murad, et al. (2018), the methodological quality of the case reports was analyzed based on the Case Report Guidelines (CARE) [Riley, 2017]. Subsequently, some of the proposed categories of these guidelines were selected as axes of analysis to respond to the objective of this study (Table 2), which are mentioned below:
Results
Study selection
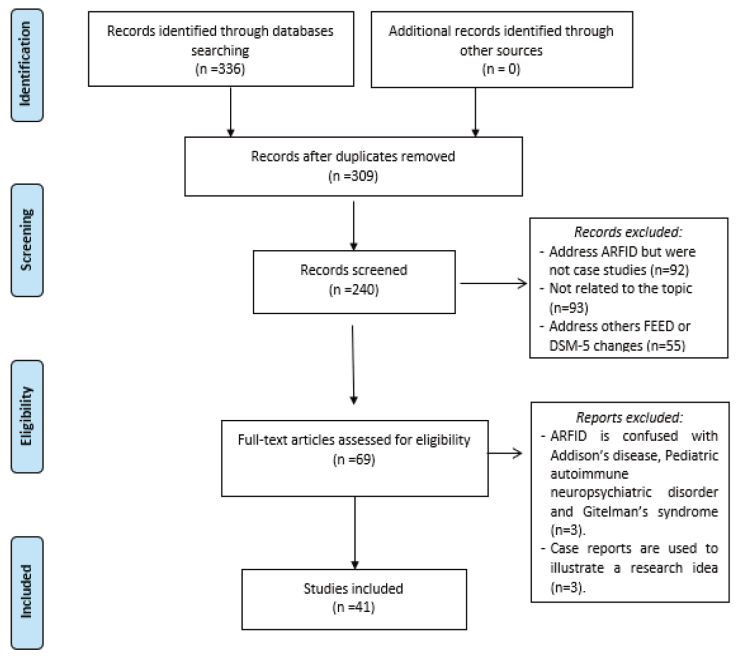
From three databases, 291 articles were obtained, 24 were eliminated because they were duplicate citations. The remaining 267 articles were examined according to the eligibility criteria mentioned above for possible selection; 220 articles were eliminated. Finally, 47 articles were chosen for analysis, nevertheless, six articles were excluded because three of them provided a diagnosis other than ARFID (Lazare, et al., 2017; Toufexis, et al. 2015; Wassenaar et al., 2018) and the remaining three articles were used to exemplify characteristics or research ideas and/or did not apply clinical intervention (Kreipe & Palomaki, 2012; Lucarelli, et al., 2017; Menzel, et al., 2018). Figure 1 presents the flowchart of the screening process.
Table 2 Axes for the analysis of results
| Analysis axes | Content |
|---|---|
| Patient Information |
|
| Clinical findings |
|
| Diagnostic evaluation |
|
| Therapeutic intervention |
|
| Monitoring and results |
|
Evaluation of the methodological quality of case reports and case series
Thirty-nine articles met more than 50% of the proposed CARE criteria, the least reported information was: diagnostic problems (12.29%), and no study reported historical and current information on the disorder organized as a timeline.
Characteristics of case studies and case series
In 2018 and 2019, 53.66% of the case reports and case series analyzed were published, the journal with the most publications was the International Journal of Eating Disorders with 19.51%, it is worth noting the role of childhood and adolescence journals such as: Journal of Child and Adolescent Psychopharmacology, Clinical Practice in Pediatric Psychology, Clinical Child Psychology and Psychiatry, Clinical Pediatrics, Journal of Adolescence y Journal of the Canadian Academy of Child and Adolescent Psychiatry which published 19.51% of the articles. Regarding the country of origin, the United States published 43.90% of case reports on this disorder.
Patient information
Demographic data
In total 66 patients were reported in the studies and case series, however, one case in the study by Alten, et al. (2020) was disregarded because did not receive the diagnosis of ARFID. In total, data from 65 participants were analyzed, where 46.15% were female and 53.85% male, ages ranged from 2 to 56 years (M = 14.80, SD = 8.85). The age ranges with the highest presence of this disorder were: from 10 to 13 years with 29.23%, from 14 to 16 years with 23.08%, and from 2 to 9 years with 21.54%, while the ranges with the lowest percentage of cases were from 17 to 19 years with 10.77%, from 20 to 27 years with 9.23% and finally the range from 41 to 56 years with 6.15% of cases.
Family medical history
The presence of family psychiatric history was evaluated showing that 70.73% of the studies did not report this information, 12.20% mentioned that their participants did not have psychiatric history, and 17.7% indicated its presence. The most common were anxiety, depression, bipolarity, and schizophrenia.
Psychosocial problems
In addition, the psychological problems of the participants were examined; the most informed aspects were social withdrawal with 32.31% (not being able to share meals with others or avoid eating in public places) and school problems with 20.0% (poor academic performance, teasing about their appearance, absenteeism or dropping out of school...). The youngest patients showed eating behavior problems when feeding with 10.77% (hiding, spitting, or playing with food, delaying eating…) and fear of maturing (difficulty separating from parents, overprotective parents...) 9.23%. Some patients reported dysfunctional family dynamics and couple problems (financial problems, parent fights, divorce, marital tension...) (13.85%), abandonment of activities that he previously carried out (4.62%) and self-harm (1.54%).
Past interventions
It was observed that 75.61% of the participants in the studies reported several previous medical consultations with specialists including pediatricians, psychologists, gastroenterologists, nutritionists, psychiatrists, endocrinologists, and geneticists, among others. In addition, 34.15% reported previous hospitalizations, however, none of the participants had been previously diagnosed with ARFID.
Clinical findings
Main sings, symptoms and medical conditions
The signs and symptoms most frequently reported by the participants were underweight 66.15% and short height 26.15%. On the other hand, it can be observed that 13.85% of the cases reported abdominal pain during feeding with no apparent organic cause.
In the physical examination, medical conditions were blood disorders (16.92%), gastrointestinal disorders (10.77%), food allergies (12.31%) and 18.86% of the participants reported no medical conditions. (Table 3).
Table 3 Main sings, symptoms and medical conditions.
| n | % | |
|---|---|---|
| Signs and Symptoms | ||
| Low weight | 43 | 66.15 |
| Growth impairment | 17 | 26.15 |
| Nausea/Vomiting | 13 | 20.00 |
| Consumption of pureed or soft-textured foods. | 11 | 16.92 |
| Abdominal (epigastric) pain | 9 | 13.85 |
| Lack of appetite | 8 | 12.31 |
| Lethargy | 7 | 10.77 |
| Constipation | 7 | 10.77 |
| Dysphagia (feeling a mass in the throat) | 7 | 10.77 |
| No liquid consumption | 5 | 7.69 |
| Pallor | 4 | 6.15 |
| Not passing your saliva | 4 | 6.15 |
| Early satiety | 4 | 6.15 |
| Reflux | 3 | 4.62 |
| Dizziness | 3 | 4.62 |
| Insomnia | 3 | 4.62 |
| Consumption of foods with high caloric intake | 2 | 3.08 |
| Overweight | 2 | 3.08 |
| Abdominal inflammation | 1 | 1.54 |
| Medical conditions | ||
| Blood (B thalassemia, anemia, macrocytic anemia, venous sinus thrombosis, hyperbilirubinemia, hypoglycemia, microcytosis, hypertension) | 11 | 16.92 |
| Food allergies (gluten intolerance or celiac disease) | 8 | 12.31 |
| Gastrointestinal (chronic peptic duodenitis, esophageal reflux, irritable bowel syndrome, Crohn’s disease) | 7 | 10.77 |
| Hormonal (Hypomenorrhea, uterine fibrosis, growth hormone deficiency) | 5 | 7.69 |
| Vitamin deficiency (A, D, E, K, B12 and folate; C scurvy) | 5 | 7.69 |
| Electrolyte abnormalities (hypocalcemia and hypomagnesia) | 4 | 6.15 |
| Bone (Osteoporosis, subacute combined degeneration of the spinal cord) | 4 | 6.15 |
| Respiratory (asthma, laryngomalacia) | 2 | 3.08 |
| Optic neuropathy due to malnutrition | 1 | 1.54 |
| Testicular cancer | 1 | 1.54 |
Diagnostic evaluation
Diagnosis: ARFID subtypes and clinical criteria of severity
The most frequent subtype of ARFID was the fear of aversive consequences of feeding with 36.92% and the presence of combined subtypes such as sensory sensitivity plus fear of feeding due to aversive consequences with 15.38%. On the other hand, the presence of clinical criteria of severity such as tube feeding was evaluated, where 39.02% of the studies reported its use and 48.78% reported consumption of food supplements.
Psychiatric comorbidities
In 26.15% of the cases, no other disorder was reported. However, some participants reported the presence of two or more disorders in addition to ARFID. Anxiety disorders were the most common (38.46%), nevertheless, although most studies reported anxiety linked to food consumption, no formal diagnosis of the presence of this disorder was reported (Table 4).
Table 4 ARFID subtypes and comorbidity
| n | % | |
|---|---|---|
| Type of ARFID | ||
| Fear of the aversive consequences of feeding (F) | 24 | 36.92 |
| Lack of interest in feeding (LI) | 12 | 18.46 |
| Sensory sensitivity + Fear of the aversive consequences of feeding | 10 | 15.38 |
| Sensory sensitivity (SS) | 7 | 10.77 |
| Lack of interest in feeding + Fear of the aversive consequences of feeding | 4 | 6.15 |
| The subtype is not specified (little information to classify) | 4 | 6.15 |
| Lack of interest in feeding + Sensory sensitivity | 3 | 4.62 |
| Sensory sensitivity + Fear of the aversive consequences of feeding + Lack of interest in feeding | 1 | 1.54 |
| Comorbidity | ||
| Anxiety Disorders (generalized, separation, social...) | 25 | 38.46 |
| Depressive Disorders (Dysthymia) | 8 | 12.31 |
| Autism Spectrum Disorder (Asperger’s) | 9 | 13.85 |
| Attention Deficit Hyperactivity Disorder ADHD | 5 | 7.69 |
| Internet gaming disorder | 3 | 4.62 |
| Substance use disorder (Alcoholism, marijuana) | 3 | 4.62 |
| Obsessive Compulsive Disorder | 2 | 3.08 |
| Neurological disorders (chorea and chronic tic disorder, sensory integration disorder) | 2 | 3.08 |
| Oppositional Defiant Disorder | 1 | 1.54 |
| Down syndrome | 1 | 1.54 |
| Panic Disorder | 1 | 1.54 |
Diagnostic test: Laboratory and cabinet studies.
The most frequently performed tests were blood tests (23.08%), which were used to identify the degree of malnutrition and vitamin deficiency. Also, tests were performed to rule out that the lack of appetite or fear of eating was due to organic causes such as endoscopies (10.77%) and imaging studies such as X-rays, ultrasounds, and MRIs (4.62% respectively).
Diagnostic tests: psychiatric/psychological assessment instruments and interviews
Assessment instruments and interviews were used as auxiliary to provide a diagnosis and identify symptoms of some associated disorders. However, only two interviews developed specifically for the diagnosis of this disorder were used Eating Disorders Assessment (EDA; Sysko, et al., 2016) and Pica, ARFID and Rumination Disorder Interview (PARDI; Bryant-Waugh, et al., 2019)
Treatment characteristics
Treatment
The most frequent treatment modality was inpatient with 46.34%, followed by outpatient with 41.46%, and finally the combination of inpatient and outpatient with 12.20%. On the other hand, 65.85% of the articles reported multidisciplinary/interdisciplinary treatment, 21.95% psychological interventions, and 12.20% medical or psychiatric.
Therapeutic Interventions
Almost 22% of the studies did not report psychological therapies as part of the treatment, however, the psychological models most used were Cognitive Behavioral Therapy (CBT) with 21.95%, Family Therapy (FT) or Family-Based Therapy (FBT), and Behavioral Therapy (BT) with 9.76%, respectively. As for the combined therapies, the most used was Cognitive Behavioral Therapy + Family or Family-Based Therapy.
Duration
Sessions and follow-ups
The number of sessions reported for CBT was from 10 to 16 with follow-ups from 2 to 24 months; FT or FBT covered from 17 to 29 sessions with follow-ups from 5 to 8 months, BT from 9 to 28 sessions with follow-ups from 1 to 9 months and in the medical interventions the hospitalization time was from 2 to 6 months with follow-ups from 2 to 5 months. In the case of combined interventions: CBT + BT was carried out in 11 sessions with follow-ups from 1 to 3 months and CBT + FT or FBT sessions were 20 with follow-ups from 4 to 12 months. It is worth mentioning that 24.39% and 43.90% of the studies did not report the number of sessions or follow-ups, respectively.
Table 5 Psychological therapeutic interventions models used.
| Therapies | N | % |
|---|---|---|
| TCC | 9 | 21.95 |
| TBF or TF | 4 | 9.76 |
| TC | 4 | 9.76 |
| TCC+TF or TBF | 3 | 7.32 |
| CBT+Pharmacological treatment | 2 | 4.88 |
| CBT+CT | 2 | 4.88 |
| TC+Teleconsultation | 1 | 2.44 |
| Parent-facilitated CT scan | 1 | 2.44 |
| TBF+ Treatment of diagnosis of emotional disorders | 1 | 2.44 |
| TBF for the three types of TERIA | 1 | 2.44 |
| TF + Pharmacological Treatment | 1 | 2.44 |
| Parent Therapy + Drug Treatment | 1 | 2.44 |
| CBT+TBF+Pharmacological | 1 | 2.44 |
| CBT + Eye Movement Desensitization and Reprocessing | 1 | 2.44 |
| Interoceptive exposure therapy | 1 | 2.44 |
Note: TC= Behavioral Therapy, CBT= Cognitive Behavioral Therapy, TF=Family Therapy and TBF= Family-Based Therapy.
Drugs administrated
During the interventions 58.53% of the studies used drugs, the most used were antipsychotics olanzapine 19.51%, antidepressants such as sertraline 12.19%, fluoxetine 9.75%, and mirtazapine 7.31% (Table 11).
Intervention outcomes
The results achieved from the interventions of the case reports and case series are shown in Table 13, with results at the physical, psychological, and social levels. However, the most frequently reported data at the physical level was weight gain (61.54%), at the psychological level, the decrease in anxiety symptoms (40%), and at the social level, the decrease in social withdrawal (10.77%).
Table 7 Intervention outcomes
| Results | n | % |
|---|---|---|
| Weight gain | 40 | 61.54 |
| Food stability and flexibility (increase in the variety of foods consumed) | 36 | 55.38 |
| Decrease in anxiety symptoms. | 26 | 40 |
| Height gain | 13 | 20 |
| Reduction of scores in psychometric instruments. | 9 | 13.84 |
| Decreased social retraction (being able to share meals with others and avoid eating in public places) | 7 | 10.77 |
| Improvement in blood parameters and vitamin restoration | 6 | 9.23 |
| Decreased feeding behavior problems (hiding, spitting, or playing with food; delayed eating) | 6 | 9.23 |
| Mastery of food techniques (parents). | 5 | 7.69 |
| Return to activities I used to do | 4 | 6.15 |
| Improvement in family dynamics | 3 | 4.62 |
| Perform activities without their parents(sleeping alone, assuming an adult role...). | 3 | 4.62 |
| Decrease in symptoms of depression | 3 | 4.62 |
| Improvement in school activities (doing sports activities and participating in class) | 2 | 3.08 |
Follow-up diagnosis and clinical improvement
Six studies (14.63%) indicated completed remission of ARFID, and one changed its diagnosis to another specified eating and food intake disorder, while 34 articles (82.92%) did not report follow-up diagnosis. However, in 22 of these articles, clinical improvement was observed, in the remaining three articles, no relevant changes were achieved due to: stigmatization of mental illness in males (Schembrucker, et, al. 2017), presence of addictions such as alcoholism (Steen & Wade, 2018), and diseases such as testicular cancer and pudendal nerve entrapment (Tsai, Singh & Pinkhasov, 2017).
Discussion
The present study aimed to analyze clinical characteristics and clinical interventions reported in case reports and case series studies of avoidant/restrictive food intake disorder (ARFID). A total of 65 cases were analyzed, concerning the demographic characteristics of the patients, it was found that the percentage by sex was similar in males (53.85%) and females (46.15%), which coincides with retrospective studies of medical records, where it is shown that the percentages by sex are not consistent (Nicely, et al. 2014; Eddy, et al. 2015; Nakai, et al., 2016).
Likewise, the age of cases was evaluated, which ranged from 4 to 56 years old. The ranges corresponding to the adolescent stage, from 10 to 13 and from 14 to 16 years old, were those with more cases reported. Although this disorder was previously only diagnosed in childhood (DSM-IV-TR, APA, 2000), it is relevant to study it throughout the different stages of human development, especially in adolescence, since, as in the present review, a study by Ducombe, et al. (2019), it was found that it was more frequent in adolescents aged from 12 to 18 years old.
Regarding the diagnostic evaluation, each of the cases was classified into subtypes of ARFID. It was obtained that the subtype fear of aversive consequences of feeding was the most reported with 36.92%, also combined subtypes such as sensory sensitivity + fear of aversive consequences of feeding were obtained with 15.38%. The above highlights the heterogeneity of the disorder and the need to tailor treatments to the different subtypes, since in these there are different symptoms that maintain eating restriction (Zickgraf, et al., 2019).
Some clinical criteria of severity of ARFID were also evaluated, such as the consumption of food supplements where 48.78% of the studies reported their use, as well as tube feeding which was used in 39.27% of the studies, although the percentage is high and some authors (Lenz, et al., 2018) point out that this type of feeding could prolong the symptoms and consequences of the disease, so early intervention by mental health providers is essential, as this could delay nasogastric tube placement.
Likewise, within the severity criteria, deterioration in the psychosocial functioning of the patient was assessed, such as social withdrawal (23.31%), school problems (20%), and fear of maturing (9.23%). This last trait is very frequent in the personality of patients with anorexia nervosa; however, it has been found that patients with ARFID also present fear of maturing (Zanna, et al. 2020).
On the other hand, as expected, the signs and symptoms most reported by participants were: low weight 66.15% and short height 26.15%. Moreover, 13.85% of the cases reported abdominal pain, although in some cases it was mentioned that the pain had no apparent organic cause, in the evaluation of this disorder it is suggested to rule out the presence of functional gastrointestinal disorders since sometimes the symptoms of these are similar to those of ARFID (Murray et al. 2019).
Regarding medical history, 75.61% of the patients in the studies evaluated reported several previous visits to a specialist and 34.15% of the patients reported previous hospitalizations. These data point out the low awareness of this disorder among health professionals, for such reason, it is necessary to give greater visibility to this disorder, so that people with this condition receive timely care and treatment (Cooney, et al. 2018; Lai, Chee & Kwok, 2019). And regarding family history, the presence of family psychiatric history was evaluated and 17.07% indicated its presence. A study by Kurotori, et al. (2019) reported that patients with ARFID have more antecedents of family mental disorders of patients with anorexia nervosa, the above should be further investigated because psychopathology in relatives could be related to the development of this disorder.
Among the clinical findings most frequently reported in the studies and case series are blood disorders (16.92%), gastrointestinal disorders (10.77%), and food allergies (12.31%). Likewise, comorbidity with other psychiatric disorders such as anxiety disorders, depressive disorders, autism spectrum disorder, and attention deficit hyperactivity disorder (ADHD) is reported, which is consistent with the findings of Kambanis, et, al. (2019).
In terms of diagnostic tests, laboratory and cabinet studies were used, among which blood tests (23.08%), endoscopies (10.77%), and radiographs (4.62%) stand out; as well as diagnostic instruments and interviews, however, despite having instruments for the evaluation of symptoms associated with this disorder such as the Eating Disturbances in Youth-Questionnaire EDY-Q (Kurz, et al., 2015) and Nine Item Avoidant/ Restrictive Food Intake Disorder Screen NIAS (Zickgraf & Ellis 2018), those were not used.
About the treatment, the most used modality was inpatient with 46.34%, however, it should be remembered that the choice of the type of treatment should be applied taking into consideration the medical, behavioral, and dietary needs of the patient (Bloomfield, Fischer, Clark & Dove 2018). Furthermore, in 65.85% of the studies, a multidisciplinary group of specialists participated, which coincides with other authors who suggest that a multidisciplinary treatment is necessary for patients with ARFID, which includes psychological care, nutritional and medical monitoring (Bryant-Waugh, 2013; Chiarello, et al., 2017).
The therapy model most used was Cognitive Behavioral Therapy (21.95%), followed by Behavioral Therapy and Family Therapy (9.76%). The number of sessions ranged from 9 to 29, and follow-up ranged from one month to 24 months. The reason why these therapeutic models are the most widely used could be due to the fact that the Cognitive Behavioral Therapy (CBT) focuses on reducing restrictive eating practices and/or selective feeding, as well as decreasing associated symptoms such as low weight, nutritional deficits and interference with daily life, through different strategies like psychoeducation, self-monitoring, behavioral experiments, systematic desensitization for the management of fear of consuming new foods (neophobia) or fear of vomiting (emetophobia), cognitive restructuring to observe the connection between thoughts, emotions, and behavior; techniques for managing anxiety such as progressive relaxation and to decrease psychosocial interference are proposed to share meals with others in different contexts (Dumont, et al. 2019). While the Family Based Therapy (TBF) proposes to empower family members to support the patient’s recovery, starting with education about the disorder, dealing with guilt, highlighting the seriousness of the disease, externalizing the disorder as the enemy and encouraging parents in refeeding strategies. Lock, et al. (2018), applied Family-Based Therapy for all three ARFID presentations, this therapy has specific targets for each of the presentations/subtype of ARFID which is suitable because takes into consideration the heterogeneity of the disorder.
Also, an important fact is that 58.53% of the studies used drugs such as fluoxetine, olanzapine, and sertraline; in this regard, Naviux (2019), mentions that selective serotonin reuptake inhibitors (fluoxetine and sertraline) have side effects that could exacerbate the difficulties in patients with ARFID, so the use of mirtazapine is recommended.
Finally, the most frequently reported treatment outcomes were weight gain (61.54%), increased eating stability and flexibility (55.38%), and decreased anxiety symptoms (40%). The foregoing demonstrates that the treatments used are adequate to attack the central symptoms of this disorder, however, early intervention is necessary to avoid the chronicity of symptoms, because, as has been seen, this disorder can remain in adulthood and malnutrition can cause serious health effects (Chiarello, et al., 2018; Alten, et al., 2020).
In conclusion, the review of studies and case series of ARFID was relevant since the main clinical characteristics of patients with ARFID and its association with other disorders were compiled and presented. In addition, important clinical findings of treatments that are little known and analyzed in the literature were known and together allowed us to know their effectiveness and possible complications or alternatives.











 nueva página del texto (beta)
nueva página del texto (beta)