Introduction
Muscle dysmorphia (MD) is an obsessive-compulsive disorder (OCD) characterized by the constant concern of insufficient muscle mass. In the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association [APA], 2013), MD is defined as a subcategory of body dysmorphic disorder (BDD). Nine percent of men with BDD have MD. However, the frequency of MD is increasing in people with and without BDD (Dos Santos, Pasarelli, Stefano, Touyz & Medeiros, 2016; Olivardia, 2001). MD affects young men concerned about their muscle mass, while women were found to be more conscious about losing weight than gaining muscle mass (Baile, González, Ramírez & Suárez, 2011; Cuzzolaro, 2018; Dos Santos et al., 2016). A study with Western men described the lack of body image satisfaction and BDD tendencies (Pope et al., 2000).
Latin American studies assessed the prevalence of MD symptomatology (MDS) on risk populations such as weightlifters in Brazil (Lima, Moraes & Kirsten, 2010) and gym users in Ecuador (González, 2015). These studies found 17% and 35% MDS, using the Muscle Appearance Satisfaction Scale and the Drive of Muscularity Scale, respectively. A Mexican study used the Adonis Complex Questionnaire, yielding a prevalence of 43% of MDS in weightlifters (Escoto, Camacho, Alvarez, Díaz & Morales, 2012). An Italian study on university students associated the increased risk of MD with the faculty they belong to, using the Muscle Dysmorphic Disorder Inventory (Bo et al., 2014).
MD is related to specific characteristics executed as part of the obsessive-compulsive spectrum. Previous studies associated MD with a hypercaloric and hypoproteic diet, besides consuming protein supplements (Cuzzolaro, 2018; Martínez-Segura, Cortés, Martínez-Amorós & Rizo-Baeza, 2015; Murray, Maguire, Russell & Touyz, 2012;). MD is also associated with a strict long-hour regime, including intense physical activity (PA) to increase muscle mass faster (APA, 2013; Murray & Touyz, 2013; Phillips, 2015; Sardinha, Oliveira & Araújo, 2008). MD is related to body dissatisfaction in male university students and weightlifters, as has been determined in several studies (Behar & Molinari, 2010; Cafri, Olivardia & Thompson, 2008; Devrim, Bilgic & Hongu, 2018; Lin & DeCusati, 2016; Peixoto, 2002).
MD is an emerging mental disorder (APA, 2013; Lopez, Pollack, Gonzales, Pona & Lundgreen, 2015; Pope et al., 2000). Mental issues are a health priority to the National Peruvian Health Institut since little research has been done in Peru (Alarcón, 2015; Caballero et al., 2010; Rondón, 2006). By studying a general population such as university students, we can determine the prevalence of MDS and factors associated. Latin American studies found focused on vulnerable populations (Caballero et al., 2010; González, 2015; Lopez et al., 2015; Pritchard, Parker & Nielsen, 2010), therefore it is necessary to understand the magnitude of the problem to propose strategies and solutions that may improve the quality of life of this population (Caballero et al., 2010). Therefore, the aim of this study was to determine the prevalence of MDS and related factors at a private university in Lima, Peru.
Method
Study design
A cross-sectional study was carried out during the first academic semester of 2015 at a private university in Lima (Peru), with over 30,000 undergraduate students, divided into four campuses.
Participants
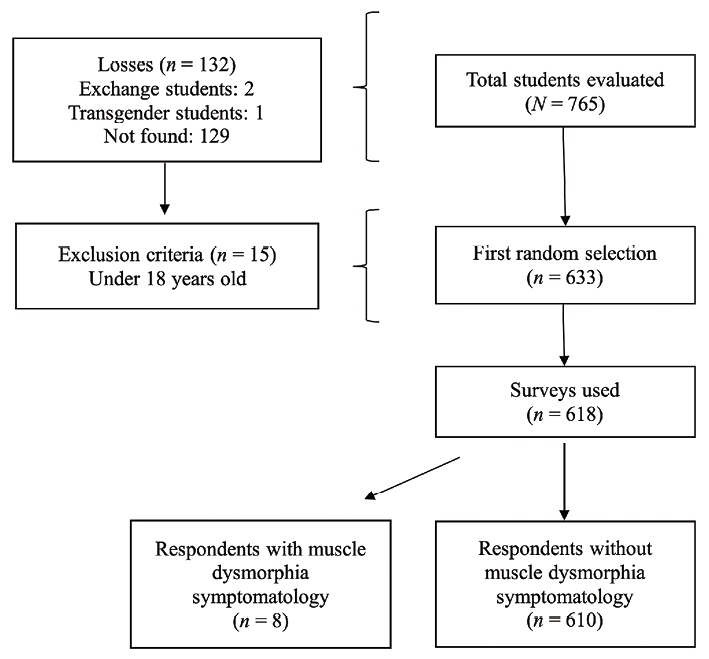
This study included male students over 18 years old. Exchange and transgender students were excluded from this study. The sample size was calculated considering a MD prevalence of 5% (Bo et al., 2014), a confidence level of 95%, an absolute accuracy of 2%, and a sample correction factor of 1.32. We considered an additional 15% to the sample size consisting of 618 students excluding eight surveys (Figure 1).
A multistage probabilistic sampling was carried out. The first phase comprised stratified by faculties and the second phase was to consider each classroom as a cluster. We randomly selected classrooms among every major. All male students were invited to take part of the study.
Ethical considerations
The study was approved by the Ethics Committee of the University and follows all the principles of the Declaration of Helsinki (World Medical Association, 2013). This study was performed with the written consent of all participants before the assessment.
Measures
Muscle dysmorphia symptomatology (MDS). We measured MDS with the Peruvian version of the Muscle Appearance Satisfaction Scale (MASS; Cook-del Aguila, Sanchez-Castro, Yacila, Bossio & Mayta-Tristán, 2016), which was adapted of the Mexican version used in a previou study (López, Vázquez, Ruíz & Mancilla, 2013). It has 19 graded items in the Likert scale from 1 (“strongly disagree”) to 5 (“strongly agree”), with a maximum score of 95. This questionnaire has five sub-scales which include Bodybuilding dependence, Muscle checking, Substance use, Injuries, and Muscle satisfaction (Mayville, Williamson & White, 2002). A cut-off score of 63 point was consideras as it has a sensitivity of 89% and a specificity of 98% for MDS (Babusa, Czeglédi, Túry, Mayville & Urbán, 2015; López, Vázquez, Ruíz & Mancilla, 2013). The cut-off total score is used to describe MDS but cannot diagnose a disorder. For the analysis of related factors, MDS was categorized in tertiles. The MASS questionnaire has a Cronbach’s alpha of .82.
Obsessive-compulsive disorder (OCD). The Peruvian version of the Yale-Brown Obsessive-Compulsive Scale Modified for Body Dysmorphic Disorder (BDD-YBOCS) was used to determine OCD (Yacila, Cook-del Aguila, Sanchez-Castro, Bossio & Tejada, 2016). This scale has 10 items with five answer options, ranging from 0 (“no symptoms”) to 4 (“extreme symptoms”). The categories for the total score are (Phillips, Hart & Menard, 2001; Steketee, Frost & Bogart, 1996): “without clinical manifestations” (0-7), “mild” (8-15), “moderate” (16-23), “severe” (24-31), and “extreme” (32-40). For this study, moderated cases or over were grouped into one category. The BDD-YBOCS questionnaire has a Cronbach’s alpha of .90.
Physical activity. To classify PA, the participants were asked about gym frequency (yes/no), type of PA, and time spent in minutes of said activity. The time was categorized in tertiles.
Diet. We applied a modified consumption frequency questionnaire (Mazzeo, 2009). This questionnaire describes the frequency of consumption per week of 18 food items (milk, yogurt, cheese, red meat, chicken, fish, eggs, protein supplements, cereals, bread, jam, butter, dressing, oil, creams and sauces, sugar, sweeteners, and desserts). The response categories for each item were “always”, “almost always (5-6 times per weeks)”, “sometimes (3-4 times per week)”, “once a week (1-2 times per week)”, and “never”, and the number of times each food consumed per day. The questionnaire has a Cronbach’s alpha of .86.
A hyperproteic dieting was considered when any kind of protein source was consumed over four times a day (18 g of protein each time) or over 1.20 g/kg/day, considering an average weight of 60.60 kg (American Dietetic Association, 2009; Instituto Nacional de Salud, 2012; Rodriguez, Di Marco & Langley, 2009). A hypercaloric dieting was considered when carbohydrates (CHOs) were consumed over six times a day (62g of CHOs each time) or exceeding 60% of the total caloric value, based on a 2488 kilocalorie dieting (Instituto Nacional de Salud, 2012; Vargas-Zárate, Becerra-Bulla & Prieto-Suárez, 2010), or when high-fat foods were consumed over three times a day (Lázaro & Domínguez, 2014). The frequency of protein supplements consumption was tested as a qualitative variable.
Other variables. We also considered general information such as age (divided into tertiles), school faculty, and academic semester year.
Procedure
Students who agreed to be part of the study signed the written consent form; afterward, they filled a 75-question survey for 10 to 15 minutes. All surveys were verified to be filled appropriately.
Data analysis
A database was created by double counting. We used STATA 14.0 program after the respective quality control, considering a value of p ≤ .05 as significant. MDS prevalence was calculated with a confidence interval of 95%. Numerical variables were expressed in mean and standard deviation and then categorized by tertiles. Categorical variables were described with relative and absolute frequencies. Variables associated with MDS were assessed with the Chi-squared test or Fisher’s exact test, as appropriate. Adjusted and crude prevalence ratios were calculated based on Poisson regression models with robust variance, assessing MDS in two ways, one with a cut-off score of 63 points, and comparing the upper tertile with the two lower tertiles. The adjusted model included all related variables in the bivariate analysis.
Results
Mean age was 21.0 years (SD = 2.3), most of the sample was part of the Engineering Faculty, and most of the students were in their fifth semester. The most practiced PA was aerobic, for example: running (excluding athletics), cycling, and water-related sports. Thirty-three percent of the surveyed population had a high-protein diet. Of all students, 31.6% consumed protein supplements one or more times a week. Additionally, 10.2% had a moderate or severe risk of having OCD (Table 1).
Table 1 Characteristics of the population under study
| Characteristics | N (%) |
|---|---|
| Age* (years) | 21.0 (2.3) |
| Faculty | |
| Business | 129 (20.9) |
| Engineering | 268 (43.4) |
| Heath sciences | 56 (9.06) |
| Other | 165 (26.7) |
| Semester | |
| 1-5 | 416 (67.3) |
| ≥ 6 | 202 (32.7) |
| Type of physical activity | |
| Aerobic | 107 (25.0) |
| Soccer | 87 (20.3) |
| Gym users | 78 (18.2) |
| Team sports | 24 (5.6) |
| Martial arts | 12 (2.8) |
| Calisthenics | 10 (2.3) |
| Cross-fit | 3 (0.7) |
| Capoeira | 1 (0.2) |
| Strength and potency | 1 (0.2) |
| More than one | 77 (18.0) |
| Other | 28 (6.5) |
| Hyperproteic diet | |
| Yes | 202 (32.7) |
| No | 416 (67.3) |
| Hypercaloric diet | |
| Yes | 415 (67.1) |
| No | 203 (32.9) |
| Obsessive-compulsive disorder | |
| No clinical manifestations | 366 (59.2) |
| Mild | 189 (30.6) |
| Moderate or severe | 63 (10.2) |
Note. * Mean (SD).
Based on the cut-off score of 63 points, 1.29% of male students of a Peruvian private university had MDS (CI 95% = 0.40-2.20%). MDS associated factors had similar results based on the two assessments applied (Table 2). A hyperproteic diet and physical activity frequency were associated with MDS considering a cut-off score of 63 points. No association with age, faculty, academic semester, hypercaloric diet, gym frequency or OCD presence (p > .05) were found in the bivariate analysis. With the MASS upper tertile, faculty, hyperproteic diet, physical activity frequency and OCD was associated with MDS. No association with age, semester, and hypercaloric diet were found in the analysis.
Table 2 Variables associated with muscle dysmorphia symptomatology with a cut-off point of 63 in the MASS and the upper tertile.
| Variable | MDS (≥ 63) | MDS (upper tertile) | |||||
|---|---|---|---|---|---|---|---|
| n | (%) | p * | n | (%) | p ** | ||
| Age | |||||||
| < 21 years | 4 | 1.4 | .99 | 94 | 33.8 | .75 | |
| 21-22 years | 2 | 1.0 | 61 | 30.5 | |||
| > 22 years | 2 | 1.4 | 45 | 32.1 | |||
| Faculty | |||||||
| Engineering | 2 | 1.6 | .99 | 96 | 35.8 | .001 | |
| Business | 4 | 1.5 | 52 | 40.3 | |||
| Health Sciences | 0 | 0 | 8 | 14.3 | |||
| Other | 2 | 1.2 | 44 | 26.7 | |||
| Semester | |||||||
| 1-5 | 3 | 1.2 | .99 | 87 | 33.5 | .62 | |
| ≥ 6 | 5 | 1.4 | 113 | 31.6 | |||
| Hyperproteic diet | |||||||
| Yes | 7 | 3.5 | .002 | 86 | 42.6 | .001 | |
| No | 1 | 0.2 | 114 | 27.4 | |||
| Hypercaloric diet | |||||||
| Yes | 5 | 1.2 | .72 | 124 | 29.9 | .06 | |
| No | 3 | 1.5 | 76 | 37.4 | |||
| Frequency of physical activity | |||||||
| >5 hours | 6 | 4.3 | .003 | 73 | 52.5 | .001 | |
| 2.1-5 hours | 1 | 0.7 | 44 | 31.7 | |||
| <=2 hours | 1 | 0.3 | 83 | 24.4 | |||
| Gym users | |||||||
| Yes | 3 | 3.9 | .07 | 50 | 64.1 | .001 | |
| No | 5 | 0.90 | 150 | 27.8 | |||
| Obsessive-compulsive disorder | |||||||
| No | 5 | 1.4 | .88 | 93 | 25.4 | .001 | |
| Mild | 3 | 1.6 | 75 | 39.7 | |||
| Moderate or Severe | 0 | 0 | 32 | 50.8 | |||
Notes. MASS = Muscle Appearance Satisfaction Scale, MDS = Muscle dysmorphia symptomatology * Fisher’s exact test, ** Chi-squared test.
We found an association between MDS and a hyperproteic diet (PRa = 9.8; CI 95% = 1.1- 86.7; p = .04) and performing PA over five hours a week (PRa = 9.5; CI 95% = 1.1-84.4; p = .04) in the adjusted model (Table 3). Considering the MASS upper tertile, we found an association of MDS with performing PA over five hours a week (PRa = 1.8; CI 95% = 1.4-2.3; p = .001), gym frequency (PRa = 1.9; CI 95% = 1.5-2.3; p = .001), hyperproteic diet (PRa = 1.3; CI 95% = 1.1-1.6; p = .01), studying in a Engineering (PRa = 1.5; CI 95%: 1.1-1.9; p = .005) or Business faculty (PRa = 1.4; CI 95% = 1.0-1.9; p = .03), and presenting moderate-severe (PRa = 2.2; CI 95% = 1.6-2.9; p = .001) or mild OCD (PRa = 1.4; CI 95% = 1.1-1.8; p = .002).
Table 3 Variables associated with muscle dysmorphia based on a crude and adjusted model according to a cut-off point of 63 and the upper tertile.
| Crude model | Adjusted model | ||||||
|---|---|---|---|---|---|---|---|
| PRc | (95% CI) | p | PRa | (95% CI) | p | ||
| Cut-off point of 63 points | |||||||
| Frequency of physical activity | |||||||
| > 5 hours | 14.68 | (1.78-120.99) | .01 | 9.51 | (1.07 -84.45) | .04 | |
| 2.1-5 hours | 2.45 | (0.15-38.92) | .53 | 2.13 | (0.14-33.58) | .59 | |
| ≤ 2 hours/Not performs | 1.00 | Reference | 1.00 | Reference | |||
| Hyperproteic diet | |||||||
| Yes | 14.42 | (1.78-116.58) | .01 | 9.83 | (1.11-86.75) | .04 | |
| No | 1.00 | Reference | 1.00 | Reference | |||
| Upper tertile | |||||||
| Frequency of physical activity | |||||||
| > 5 hours | 2.15 | (1.68-2.75) | .001 | 1.78 | (1.37-2.31) | .001 | |
| 2.1-5 hours | 1.30 | (0.95-1.76) | .10 | 1.19 | (0.88-2.31) | .26 | |
| ≤ 2 hours/Not performs | 1.00 | Reference | 1.00 | Reference | |||
| Gym users | |||||||
| Yes | 2.31 | (1.86-2.86) | .001 | 1.86 | (1.48-2.35) | .001 | |
| No | 1.00 | Reference | 1.00 | Reference | |||
| Hyperproteic diet | |||||||
| Yes | 1.55 | (1.24-1.94) | .001 | 1.32 | (1.07-1.65) | .01 | |
| No | 1.00 | Reference | 1.00 | Reference | |||
| Faculty | |||||||
| Engineering | 1.34 | (1.00-1.81) | .05 | 1.48 | (1.13-1.95) | .005 | |
| Business | 1.51 | (1.09-2.10) | .01 | 1.40 | (1.03-1.90) | .03 | |
| Health Sciences | 0.54 | (0.27-1.07) | .08 | .63 | (0.32-1.24) | .18 | |
| Other | 1.00 | Reference | 1.00 | Reference | |||
| Obsessive-compulsive disorder | |||||||
| Moderate or severe | 2.00 | (1.45-2.70) | .001 | 2.16 | (1.61-2.90) | .001 | |
| Mild | 1.56 | (1.22-2.00) | .001 | 1.45 | (1.14-1.84) | .002 | |
| No | 1.00 | Reference | 1.00 | Reference | |||
Notes. PRc = Prevalence ratio from de crude model, PRa = Prevalence ratio from de adjusted model.
Discussion
The prevalence of MDS in the present study was 1.29% in men students of a private university in Lima. We have not found similar studies in Peru; however, a Mexican study reported a 1.3% of sedentary men have MDS, without being university students (Baile et al., 2011). The low prevalence of MDS found in male university students is specific to a group related to the faculty and PA frequency. Likewise, other studies used different instruments to measure MDS (e.g., Muscle Dysmorphia Inventory), including other criteria for its diagnosis. Different studies using MASS used other cut-off points to determine MDS in specific populations rather than general ones (Cella, Iannaccone & Cotrufo, 2012; Chaney, 2008; Martínez, Cortés, Rizo & Gil, 2015). A research carried-out on university men students in non-vulnerable careers, such as Medicine, or susceptible careers, such as Exercises and Sports Science, show a prevalence of 0% and 11%, respectively (Bo et al., 2014; Escoto et al., 2012).
A hyperproteic diet is associated to MDS. This result is similar to a previous study where a hyperproteic diet (> 2g/kg/day) and a normocaloric diet where associated to MDS using a 24 h food consumption frequency assay (Martínez et al., 2015). The same study also mentioned a normal intake of lipids. We also analyzed the protein supplementation, which is not associated with MDS in this study. However, people with MD often consume protein supplements. A study of weightlifters showed that 90% who had MD consumed protein supplements, 49%, carbohydrates, and 49% creatine, which are popular supplements to build muscles (Martínez-Segura et al., 2015). Our results confirm that on a general population of college students consuming a hyperproteic diet is associated with MDS not considering the consumption of protein supplements.
An association between MDS and the frequency of PA over five hours a week was found. This finding supports a Mexican study showing that 68% of people with MDS went to the gym five or six days a week and 27% exercised two or three hours every day (Zepeda, Franco & Valdés, 2011). It resembles our findings of association between gym users and MD in our adjusted model. Researches described the practice of activities such as high-intensity weightlifting sessions and monitored walks to consume calories without affecting muscle mass (Murray et al., 2012; Murray, Rieger & Touyz, 2011). Our results show that MDS is associated with PA frequency in university men students.
By the analysis by tertiles, MDS and OCD are associated. This variable has been associated with body dissatisfaction. This last result supports a study which determined that 8% of weightlifters presented body dissatisfaction (Behar & Molinari, 2010), a characteristic also found in university students (Grieve & Shacklette, 2012). However, a study found no association between MDS and OCD in a population similar to ours (Grieve & Shacklette, 2012). MD has been associated with a sense of threat by a body-related negative comment in men university students (Menees, Grieve, Mienaltowski & Pope, 2013), therefore body dissatisfaction may lead to a depressive disorder (APA, 2013). MD is a BDD where the creation of habits and routines develop muscle mass. Persons with MD are unaware of their condition, unlike a person with OCD. Although, MDS and OCD are not associated in our study (considering a cut-off score of 63 points), it is important to note it is a risk factor for men university students since body dissatisfaction might lead to the desire to make physical changes (Menees et al., 2013).
This study measured the prevalence of MDS using a self-applied assessment in a general university student population, regardless of the gym frequency and low-risk careers. The use of an assay instead of a clinical interview limits identifying MD as a clinical diagnosis and focuses only on symptomatology. Therefore, we recommend as a first step to screen potential candidates for clinical diagnosis in future studies. However, this survey is feasible to use for the general aim of the study. A self-applied instrument can bias by the presumed social desirability of what it is expected of them to be answered. However, this limitation has not invalidated our results since the questionnaire was anonymous.
This study did not measure the association between MDS and other factors such as the use of steroids or other psychosocial variables (e.g., depression, family environment, experiences and weight in childhood, and media). Further, we propose that future studies analyze the general population to determine MDS prevalence beyond specific populations, such as university students. We recommend using a detailed log of food consumption over a 24 h to analyze the diet of the assessed participants and the exact daily consumption of macronutrients. Research on dietary practices will allow formulating strategies for adequate future nutritional counsel for this group of people.
In conclusion, this study showed that 1.3% of men students in a private university displayed MDS. Also, there is an association between the practice of PA over five hours a week and a hyperproteic diet with MDS. MD is a frequent disorder, and it is present in the general population and needs to be investigated in depth to face this emerging problem.











 nueva página del texto (beta)
nueva página del texto (beta)