Introduction
Adherence to health recommendations has been an issue of social concern for many decades (Martos, & Pozo, 2011a; Serrano-Castro, Pozo-Muñoz, Alonso-Morillejo, Martos-Méndez, & Bretones-Nieto, 2011; Turk, & Meichembaum, 1991; Zeber et al., 2013). Advances in medicine, improved nutritional guidelines, improved quality of life in general, hygiene practices in particular, and the development of effective preventive and curative measures, such as vaccines and antibiotics, have made it possible to win the battle against most infectious diseases. However, these changes have increased the number of people with long-term illnesses, functional limitations, and physical and psychological disabilities; that is, chronic patients (Smith, Anderson, Salinas, Horvatek, & Baker, 2015). Once again, this raises the issue of quality of life, although from a different perspective.
There is evidence that health habits have a direct impact on the individual's health (Jackson, Tucker, & Herman, 2007). One of the most-studied health behaviors is treatment adherence or adherence behavior. This can be defined as the extent to which a person's behavior (taking medication, following a diet, making lifestyle changes, etc) coincides with the advice received regarding health and prescriptions (Epstein, & Cluss, 1982; Rosner, 2006). Similarly, according to Meichenbaum and Turk (1991), the term adherence is used to refer to the increased involvement and voluntary collaboration of the patient in a course of behavior accepted by mutual agreement with the health provider to produce a desired preventive or therapeutic result. The World Health Organization (2004) refers to adherence as a multidimensional phenomenon determined by the interplay of five sets of factors: the health system or healthcare team, the disease, socioeconomic aspects, the treatment, and the patient.
Adherence to medical recommendations is vital to patients with a chronic illness. Once a patient has been diagnosed as having a chronic illness, major lifestyle changes need to be implemented. Such patients need to follow a strict drug regimen, take medications several times a day, or even self-administer daily insulin injections in the case of diabetic patients (Gross et al., 2003). In addition, maintaining a good quality of life has increased the importance of diet and daily exercise (Hayes, 2002). Patients with chronic diseases should adopt behaviors that promotes or protects health. That is, they are recommended to change their lifestyle: they ought to follow a healthy diet, take physical exercise, and should not smoke or drink alcohol (Ferrer, 1995). Therefore, the extent to which the patient feels able to carry out these changes will be crucial to developing these healthy behaviors and, ultimately, to their adhering to treatment (Bandura, 1999; Granados, Roales-Nieto, Moreno, & Ybarra, 2007).
Self-efficacy and Health Behavior
One of the cognitive variables with the most influence on people's behavior appears to be self-efficacy. Several models include self-efficacy as a determining factor in adherence. The Attitude, Social influence, and Self-efficacy (ASE) psychosocial model suggests that an adherent patient should have a positive attitude toward drug compliance, social influence that encourages adherence, and sufficient self-efficacy to perceive herself/himself as being able to take the medication as prescribed (Fernández López, Comas, García, & Cueto, 2003). In addition, the well-known Health Belief Model (HBM) (Becker, & Mainman, 1975; Rosenstock, 1974) also incorporates the construct of perceived self-efficacy to explain health protective or preventative behavior (Strecher, & Rosenstock, 1997). Nevertheless, Bandura's Self-efficacy Theory, set within Social Cognitive Theory (Bandura, 1977), provides the greatest support for the relationship between self-efficacy and health behaviors (Bandura, 2005).
Self-efficacy refers to the belief or beliefs a person holds in terms of their own ability to successfully perform the behavior required to produce certain outcomes (Bandura, 1999). In relation to the present study, a chronic patient who feels able to successfully fulfill medical recommendations regarding medication, diet, and physical exercise will be more likely to successfully perform appropriate health behaviors. A person's beliefs concerning self-regulation and their ability to implement this type of behavior will be decisive. People will be more motivated if they perceive that their actions can be completed; that is, if they are convinced that they have the personal abilities to allow them to govern their actions (Connolly, Aitken, &Tower, 2013). In this way self-efficacy can influence a person at the affective, cognitive, and motivational levels. A specific vulnerability or resistance to stress may exist depending on the level of self-efficacy and therefore this can affect their ability to adapt to the environmental and social demands (Bandura, Pastorelli, Barbaranelli & Caprara, 1999), as well as to the demands imposed by the experience of living with a chronic disease (Avendaño, & Barra, 2008).
In this sense, treatment adherence behavior has been positively associated with perceived self-efficacy (Chen et al., 2013); specifically, self-efficacy has received considerable attention as a predictor of treatment failure (Álvarez, & Barra, 2010).
The self-efficacy model has been successful in predicting health behaviors (Bandura, 1999). This model tends to significantly correlate with the health actions investigated in this study, and is therefore a relevant element that contributes to the development of health actions, whether healthy or unhealthy. However, self-efficacy and health beliefs typically determine only some of the variations in health behavior. Thus, beyond the direct links between self-efficacy and adherence to treatment, other potential mechanisms have been hypothesized through which the patient's beliefs on their capacity to act effectively could improve treatment adherence and thus health and wellbeing.
One of these mechanisms is social support (Raggi, Leonardi, Mantegazza, Casale, & Fioravanti, 2010). In fact, Bandura (1977) already suggested that human behavior was the result of interactions between the self-system (personal variables such as self-efficacy) and external sources of influence (such as social support and interpersonal relationships in general), since the individual operates within a set of socio-cultural influences. Thus, interpersonal relationships, as well as self-efficacy, can play a relevant role in the health behavior of chronic patients. Although self-efficacy has a direct effect on health and treatment adherence, it seems reasonable to assume that interpersonal relationships can influence this cognitive variable, such that the influence of self-efficacy beliefs on adherence behavior may be mediated by the perceived social support.
Interpersonal Relationships and Health Behavior
A large number of studies have shown that interpersonal relationships have a direct significant impact on health and wellbeing (Cohen, Gottliebb and Underwood, 2000; Martos, & Pozo, 2011a; Martos, Pozo, & Alonso, 2008; Uchino, 2004). Hence, health problems are more likely to occur and are more pronounced among people who lack these relationships or social support (Hoth, Christensen, Ehlers, Raichle, & Lawton, 2007).
Regarding health behavior, social support has a decisive influence on treatment adherence, particularly in the case of chronic patients. Low levels of social support may lead to the failure to adopt a healthy lifestyle and to poorer compliance with medical recommendations (Kara, Caglar, & Kilic, 2007; Marín-Reyes, & Rodriguez-Moran, 2001), whereas perceived social support has a positive association with treatment adherence in various conditions and diseases, including hypertension, diabetes, cardiovascular disease, and HIV (Bosworth, Oddone, & Weinberger, 2006; Molassiotis et al., 2002). In other words, social support can buffer the stress of chronic disease and enable the individual to engage in more adaptive and healthier behavior leading to improved treatment adherence.
The presence of an intimate partner can directly or indirectly influence patient health behavior, thereby facilitating adherence through the internalization of norms and the provision of sanctions when behavior is not conducive to health (social control hypothesis: Lewis, & Rook, 1999; Umberson, 1987). On the other hand, a social network composed of individuals who do not offer support to the chronic patient may be a hindrance to practicing healthy habits, limit the time and energy available to engage in healthy behavior, or lead to stressful situations that compromise the attitudes and behavior needed to achieve treatment adherence in these patients (Revicky, & May, 1985).
The novelty of this study is based on the hypothesis that social support acts as a mediating variable between self-efficacy and adherence behavior. That is, self-efficacy will have an increased or decreased impact on health and adherence according to the level of perceived social support and other support-related variables.
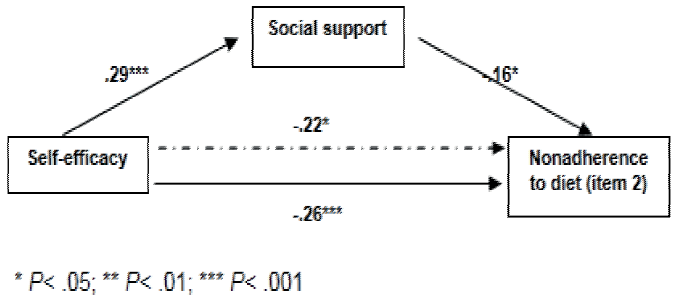
Thus, interpersonal relationships have a two-way influence (direct and indirect) on health, wellbeing, and healthy behaviors in chronic patients. It has been shown that social support directly affects health behavior (Ladero, Orejudo, & Carrobles, 2010). However, some authors have also shown that social support has a mediating role between the patient's specific beliefs, health, and behavior in relation to their disease (Fernández et al., 2001; Rodríguez-Marín, 2006; Vinaccia et al., 2005). This indicates that there is a sufficient basis to investigate the role of social support as a mediator apart from the known direct associations between health beliefs, social support, and health behavior (treatment adherence). Based on the above, the aim of this work is to test a mediational model to investigate novel associations between self-efficacy, interpersonal relationships among chronic patients, and treatment adherence (healthy behavior). Figure 1 shows the mediating model used in this study.
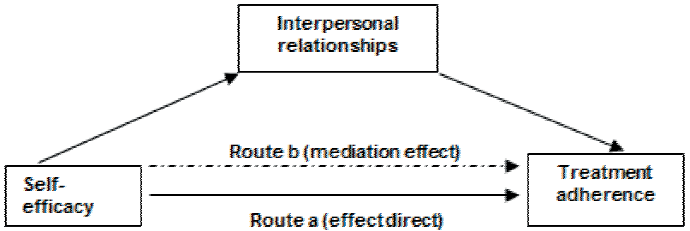
Figure 1 Model of interpersonal relationships as variables mediating self-efficacy and treatment adherence
Taking into account previous findings, we first examine the relationships between self-efficacy, social support, and treatment adherence (medication, diet and physical exercise) in a sample of chronic patients. Second, in line with the proposed mediational model, we investigate whether social support mediates self-efficacy and treatment adherence. Thus, it is hypothesized that self-efficacy is positively correlated with social support and satisfaction with support, and negatively with nonadherence to treatment. In addition, it is predicted that there is a significant association between interpersonal relationships and adherence to treatment. Finally, in line with the mediational model, it is hypothesized that the relationship between self-efficacy and nonadherence is mediated by the levels of perceived social support among chronic patients and their level of satisfaction with it.
Method
Sample
The sample was composed of 202 chronic patients living in Spain. Ages ranged from 21 years to 65 years, with a mean of 56.23 years (SD = 8.98). Of the total sample, 68% were women and 32% were men. Of the participants, 40% had hypertension, 29% had dyslipidemia, 18% had diabetes, and 13% had Chronic Obstructive Pulmonary Disease (COPD).
Instruments
Self-efficacy
Perceived self-efficacy was measured using an adapted version of the Chronic Pain Self-Efficacy Scale with Spanish people (Martín-Aragón et al., 1999), consisting of 10 items. In this instrument the patient values the capacity to manage different situations related to the disease. Responses range from 1 "completely unable" to 5"completely able". The higher the score, the higher the self-efficacy. Cronbach's alpha was .78.
Social support
Social support was measured using the translated and validated Spanish version (Martos, & Pozo, 2011b) of the Scale of Perceived Social Support Specific to the Illness (Revenson, Schiaffino, Majerovitz, & Gibofsky, 1991), which consists of three 20-item subscales related to partner, family, and friends. This scale measures positive and negative (non-functional) support from these three sources. This study only used the part of the questionnaire related to functional social support, which consists of 16 items on social support, for example, "Listened to you", "Made you feel you have something positive to contribute to others", and "Did small favours for you". Responses range from 1 "never" to 5 "always" (the higher the number, the greater the perceived social support). The original scale had an overall internal consistency of .90 in the case of positive support. Internal consistency was .94 for the sample of chronic patients analysed in this study.
Satisfaction with social support
Satisfaction with the social support received by chronic patients was measured using three items developed specifically for this study, one for each of the three sources considered (partner, family, and friends). Cronbach's alpha was .75.
Non-adherence to treatment
Nondherence was measured using an adapted version of the Haynes-Sackett test (Haynes, Sackett, Taylor, & Show, 1979), which was originally composed of two items. Responses on one of the items follow a dichotomous format in which the interviewee indicates whether he/she has ever failed to comply with treatment for their chronic disease (item 1), preceded by instructions which recognize the difficulties most people experience in following the doctor's advice. In this case, this item is subdivided into three items focusing on nonadherence to medication, physical exercise, and the diet recommended by the doctor. The other item has an open-response format in which the patients record the number of times they have forgotten to take their medication during the last 7 days (item 2), or the number of times they have not followed the exercise plan or diet recommended by their doctor.
Procedure
Stratified random sampling was used to select participants based on the variables age group (patients more than 65 years were excluded to avoid bias due to the presence of multiple disease, etc) and type of disease (COPD, diabetes, dyslipidemia, and hypertension). An appointment was made with the patients by telephone. They voluntarily attended their usual Health Center, where they were informed of the aims of the study, that the interview was anonymous, and that it would last approximately 2 hours.
Data Analysis
After all the chronic patients had been interviewed, the data were entered into a database and coded for subsequent statistical analysis using the SPSS software package (version 22.0 for Windows).
After conducting the descriptive analyses, a series of correlation analyses and corresponding regression analyses were performed with the aim of assessing the potential mediating role of social support in self-efficacy and treatment adherence. The principles outlined by Baron and Kenny (1986) were taken as a reference framework for all relevant analyses. According to these authors, the central idea of a mediation model is that the effects of the independent variable on behavior (dependent variable) are mediated by different transformation processes or variables. In general, a given variable can be said to function as a mediator to the extent that it represents the relationship between the predictor and the criterion.
Results
Descriptive Analyses
The participants had medium- to high self-efficacy regarding their disease (M = 3.92; SD = .73). In terms of social support, the mean was 3.39 with a standard deviation of .72, although satisfaction with social support was higher (M = 4.18; SD = .78). The descriptive analysis showed that 47% of the participants stated that they had sometimes not complied with their prescription, 76% had not followed the recommended diet, and 77% had not followed their exercise plan. Despite these high percentages of nonadherence, 82.4% of the patients stated that they had not forgotten to take their medication during the last 7 days. Regarding diet, 50% stated they had followed it during the last 7 days and 44.7% stated they had completed the exercise plan during the last 7 days. Table 1 shows the results of the correlation analysis. As shown, self-efficacy was positively associated with social support and satisfaction with received support, and negatively associated with nonadherence to diet and physical exercise during the last 7 days (item 2). On the other hand, increased levels of social support and satisfaction with support were negatively associated with nonadherence to treatment during the last 7 days. As measured by item 1 "Sometimes you did not comply with the medication, diet or exercise plan", no significant correlations were found between nonadherence and any of the social support variables or self-efficacy. For this reason, the subsequent analysis of mediation addressed the extent of nonadherence in terms of the number of times the patients did not take medication, follow the diet, or take physical exercise during the last 7 days (item 2).
Table 1 Correlational analysis of the measures evaluated
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | ||
|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Self-efficacy | ----- | ||||||||
| 2. | Social support | .29** | ----- | |||||||
| 3. | Satisfaction with support | .28** | .78** | ----- | ||||||
| 4. | Nonadherence to medication (item 1) | -.06 | -.10 | -.08 | ----- | |||||
| 5. | Nonadherence to diet (item 1) | -.10 | -.13 | -.11 | .21** | ----- | ||||
| 6. | Nonadherence to exercise (item 1) | -.09 | -.06 | -.00 | .01 | .42** | ----- | |||
| 7. | Nonadherence to medication (item 2) | -.04 | -.08 | -.11 | .37** | .06 | -.09 | ----- | ||
| 8. | Nonadherence to diet (item 2) | -.23** | -.18* | -.11 | .16* | .38** | .11 | .28** | ----- | |
| 9. | Nonadherence to exercise (item 2) | -.33** | -.23** | -.21** | .09 | .19* | .39** | .11 | .36** | ----- |
* P< .05; ** P< .01
Mediational Analysis
In line with the mediation framework presented by Baron and Kenny (1986), a series of regression analyses were conducted to determine whether social support plays a mediating role between health beliefs and treatment adherence in patients. For a mediator effect to be present, certain requirements must be met regarding the regression analysis: 1) The independent variable (self-efficacy) and the mediating variable (social support) are actually related; 2) The mediating variable (social support) has a unique and significant effect on the dependent variable (nonadherence); 3) The independent variable (self-efficacy) has an effect on the dependent variable (nonadherence) in the absence of the mediating variable (social support); and 4) The inclusion of the mediating variable (social support) to the model decreases the effect of the independent variable (self-efficacy) on the dependent variable (nonadherence). In this case, self-efficacy may disappear from the regression equation when including social support in the analysis (which would mean that the effect of mediation would be clearer and more obvious) or self-efficacy may decrease its effect on nonadherence when including social support in the regression (see Table 2).
Table 2 Mediational analysis of the effect of social support and satisfaction with social support on self-efficacy and treatment adherence
| Independent variable (IV) Self-efficacy |
Dependent Variable 1
(DV) Nonadherence to medication |
Dependent Variable 2
(DV) Nonadherence to diet |
Dependent Variable 3
(DV) Nonadherence to physical excercise |
|||
|---|---|---|---|---|---|---|
| Mediators | Social support |
Satisfaction with Support |
Social support |
Satisfaction with Support |
Social support |
Satisfaction with Support |
| Effect of IV on mediators | β=.29; t=4.18*** |
β=.28; t =4.09*** |
β=.29; t =4.18*** |
β=.28; t =4.09*** |
β=.29; t =4.18*** |
β=.28; t =4.09*** |
| Effect of mediators on DV | No effect | No effect | β=-.16; t =-2.26* |
β=-.19; t =-2.70** |
β=-.23; t =-2.91** |
β=-.21; t =-2.75** |
| Direct effect of IV on DV (route a) | No effect | No effect | β=-.26; t =-3.68*** |
β=-.26; t =-3.68*** |
β=-.33; t =-4.43*** |
β=-.33; t =-4.43*** |
| Effect of mediation (route b) | No effect | No effect | β=-.22; t =-3.16** |
No effect | β=-.29; t =-3.95** |
β=-.29; t =-3.92** |
* P< .05; ** P< .01; *** P< .001;
The analyses show that social support and satisfaction with social support functioned as mediators of perceived self-efficacy regarding the patients managing their disease and adhering to treatment. Specifically, nonadherence to the physical exercise plan (during the last 7 days) is the variable that confirms the mediating effect of social support (β = -.29; p <.005) and satisfaction with social support (β = -.29; p <.005). That is, by including both social support and satisfaction with support in the regression analysis, the direct influence of self-efficacy (β = -.33; p <.000) on nonadherence decreases, showing that interpersonal relationships function as mediators. In this case, although self-efficacy does not disappear from the regression model, its effect is reduced (Figure 2).
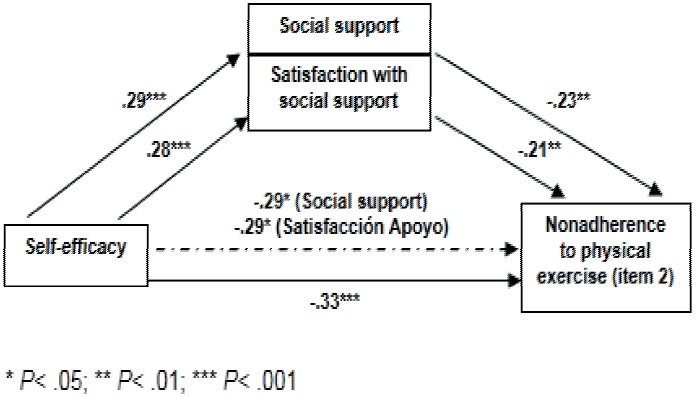
Figure 2 Social support and satisfaction with social support as mediators (self-efficacy -nonadherence to physical exercise)
On the other hand, social support also mediates the effect of self-efficacy on nonadherence to the dietary recommendations. In other words, patients who perceive more support from the three sources referred to may feel more able to follow a recommended diet, whereas those with low levels of social support may not do so, as these circumstances may lower their perceived level of self-efficacy (β = -22, p <.005). Thus, the direct influence of self-efficacy on nonadherence to diet (β = -.26; p <.000) is less when perceived social support is included in the regression model (Figure 3). Finally, no significant association was found regarding the role of interpersonal relationships as mediating self-efficacy and adherence to medication.
Conclusions
This study investigated the role of social support and self-efficacy on adherence to treatment in chronic patients. It was found that social resources function as a mediating mechanism that explains the relationship between self-efficacy and adherence behavior. In line with previous studies (Kronish, & Ye, 2013; Luszczynska et al., 2010), it was found that low perceived self-efficacy was associated with nonadherence to health recommendations among the participants. Individuals who have a sense of self-efficacy will be able to adhere more easily to the medication, recommended diet or exercise plan prescribed by their doctors.
The results confirm that perceived social support and satisfaction with support have a negative association with nonadherence to treatment, corroborating the results of other studies (Bosworth et al., 2006; Molassiotis et al., 2002). Similarly, it was also found that patients with higher levels of self-efficacy stated that they had more social resources available and were satisfied with them. These results confirm previous findings that interpersonal relationships can positively influence patients (Acuña-Gurrola, & González-Celis-Rangel, 2010), who thus feel more prepared and willing to comply with the recommended treatment; that is, they feel more self-efficacious.
On the other hand, the mediational analyses indicated that social support and satisfaction with support have both a direct and indirect impact on treatment nonadherence. Social support changes the degree to which the patient feels able to perform health behaviors. Chronic patients receiving social support from family and friends are in a better position to see themselves as being able to fulfil treatment such that their health and wellbeing improve. These interpersonal relationships directly help the patient to engage in the desired health behavior (e.g., by providing them with information on the importance of their disease, which another member of the family may have, or serving as role model of good health habits, thereby helping the patient to more easily practice them). Thus, patients with increased levels of social support will feel more self-efficacious in terms of adhering to healthy behavior; this attitude is important to achieving treatment success and, in general, improving the health of patients (Serdá, Del Valle, & Marcos-Gragera, 2012).
Specifically, the results indicate that interpersonal relationships act as mediators when adhesion behavior is associated with non-compliance with recommended physical exercise or diet plans (Anderson, Winette, Wojcik, & Williams, 2010). It appears that nonadherence to medication is not affected by the mediating effect of social support and satisfaction with perceived support. These results may be due to the fact that taking physical exercise and following a diet are health behaviors that may require more support from relatives in order to be implemented, whereas taking medication is a more personal activity that the patient may have more deeply internalized as part of their set of healthy behaviors. On the other hand, family support regarding taking physical exercise and following a diet is essential to these patients (Martín et al., 2007). Moreover, several authors have confirmed that adherence to treatment is worse regarding exercise and diet than taking medication (Froján, & Rubio, 2005; Martos et al., 2008; Sarafino, 2006).
In short, perceived self-efficacy, i.e. the belief in one's ability to organize and implement the actions required to manage future situations (in this case, that patients believe they can do something to manage their adherence behavior and, more importantly, health behavior) is modified by variables related to social support, which is key to future interventions. In this respect, when the self-efficacy model is applied as a psychological model in the setting of healthcare, one of the main problems is the assumption that we are normally trying to teach people what they should do or need to do to engage in healthy behavior. In this regard, Bandura (1994) has suggested that people should be taught skills that promote self-efficacy, such as the self-regulation skills that would enable them to exercise control over themselves and avoid the negative influence of others in the practice of healthy behavior (Brassington, Atienza, Perczek, DiLorenzo, & King, 2002). In this line, the findings of this study may be of interest not only in relation to developing theoretical models or to better understand the associations between the variables analysed, but particularly to developing intervention programs that promote patient self-efficacy and therefore treatment adherence, while taking into account the important mediating role of social support (Anderson et al., 2010).
Finally, attention should be drawn to the limitations of this study. First, we used a self-report measure to collect information on nonadherence to treatment (Haynes-Sackett, 1979). Although this measure has been fully assessed in the literature and applied in practice (Amado, Pujol, Pacheco & Borras, 2011; Epstein, & Cluss, 1982), future studies could include a physical measure of taking medication, such as blood insulin levels in the case of diabetic patients, given that no significant relationships were found between nonadherence to medication and other variables in this study. This aspect should be investigated in more detail to better understand the relationship between medication adherence, self-efficacy, and perceived social support.
Moreover, the chronic diseases of the participants are among the most common in the world, some of which are responsible for very many deaths each year (Roglic, & Unwin, 2010; WHO, 2004). Nevertheless, the variables analysed in this study may have a greater impact on patients with other chronic diseases; thus, this study could be extended to include patients with other diseases, such as epilepsy or cancer, with the further aim of investigating whether there are significant differences between the diseases studied.
Although this study investigated the mediating role of social support in self-efficacy and treatment adherence, a very important question remains for future studies to investigate: can self-efficacy mediate the positive association between social support and treatment compliance? Moreover, could other health beliefs, such as perceived vulnerability or perceived severity, be mediating this important association?.











 nueva página del texto (beta)
nueva página del texto (beta)