Introduction
COVID-19 has caused more than 2.5 million of deaths among more than 100 million cases around the world (World Health Organization, 2021) since its appearance in Wuhan, China in late 2019. It reached Mexico in early 2020 after it caused many casualties in western Europe. Mexico is now one of the countries with the largest death rate due to COVID-19, with about 150 official deaths per 100,000 inhabitants (Johns Hopkins Coronavirus Resource Center, 2021) although excess of mortality statistics (INEGI, 2020) implies this number could be three times higher. Mexico City is not only the largest city in Mexico with almost 9 million inhabitants, but one of the largest in the world. Fortunately, its data regarding COVID-19 patients is publicly available and can be analyzed to obtain information that may guide public policy and personal decisions.
Romero-Zavala M. and Despeguel L. (2020) have done extensive research based on death certificates in Mexico City to keep track of excess of mortality, a very effective method to account for the death of people that were not diagnosed with COVID-19, unfortunately their reports do not include detailed information about the three causes analyzed in this study.
This work reports the findings of a descriptive study based on data retrieved July 28th, 2020 from the Mexico City government. Results show the relative effect of these three causes in COVID-19 patients, concluding that all three causes are related to death increase among patients.
Method
This is a descriptive study based on public information about suspected COVID-19 cases retrieved July 28th, 2020 from the web site of CDMX government´s Sistema Nacional de Vigilancia Epidemiológica (2020). Data was retrieved immediately after learning of such web site in an article published July 24th (Flannery, 2020). Original data includes information about suspected COVID-19 cases; since one data field indicated if the suspected case had been confirmed by a COVID-19 test, it was decided that only confirmed cases were to be analyzed in this study and those cases that were not confirmed were to be excluded.
The number of deaths among American and western European population by age range was obtained from a graph published by The Economist (2020) in June of 2020 and death rate was calculated using population age distribution published by populationpyramid.com (2020).
To calculate the proportion of cases and deaths by age range in Mexico City, the 2015 population pyramid of Mexico City was used (Gobierno de la CDMX, 2017). To obtain the proportion of cases and deaths relative to population, they were first adjusted to match the number of cases and deaths reported July 30th by CONACYT (2020). Sistema Nacional de Vigilancia Epidemiológica (2020) reported data of 24,497 confirmed cases whereas CONACYT reported 71,296 cases, 2.9 times as many. Among these confirmed COVID-19 patients, Sistema Nacional de Vigilancia Epidemiológica (2020) reported that 2,552 had died, whereas CONACYT reported 7,136 deaths, 2.8 times as many. Both proportions are very similar and are consistent with the proportion of 2.87 between excess of mortality of 184,917 reported by INEGI (2020) for the period January to august, 2020 and 64,414 reported deaths due to COVID-19 reported by Secretaría de Salud de México on august 31st 2020 (Angel, 2021). It is assumed that confirmed cases and deaths reported by Sistema Nacional de Vigilancia Epidemiológica (2020) are a sub-set of those reported by CONACYT (2020).
Case and death frequency by gender, age range and previous health condition were calculated using the OpenOffice spreadsheet program by using conditional, sorting, and counting commands. Tables and graphs were obtained using copy and graphing commands in the same spreadsheet program.
Results and discussion
As mentioned before, three possible causes of death of COVID-19 infected people were studied: age, gender, and previous health condition.
The effect of age
In an article published by Forbes, Flannery (2020) argues that Mexicans who got COVID-19 were dying at a much younger age than people in developed countries. Fig. 1 (Sistema Nacional de Vigilancia Epidemiológica, 2020 and The Economist, 2020) supports his findings by showing that Mexicans with COVID-19 between 41 and 80 years old are much more at risk of dying than Americans and western Europeans who have the same age and condition. Novosad et al. (2020) also find a larger death rate among middle-age Indian COVID-19 patients than among British COVID-19 patients. The findings of both studies suggest that the difference in death rate due to age might be found when comparing developed to less developed countries.

Source: Elaborated by the author with data from Sistema Nacional de Vigilancia Epidemiológica and The Economist.
Fig. 1 Death/Population ratio by age range of COVID-19 patients in Mexico City, the United States and Western Europe.
However, the proportion of Americans and western Europeans over 80 years old that died having COVID-19, is twice as high as that of Mexicans who have their same age and condition. One possible reason of such a difference in mortality among older people in different countries is that the proportion of cases is also much larger. Case proportion is more difficult to compare between Mexico and developed countries because much less testing has been done in Mexico (Roser et al., 2021), so that more cases might go undetected. Nevertheless, one way to compare the increase in case proportion with age in different countries was found: as of the first quarter of 2021, case/population proportion in Mexico increases only 5% for men older than 80 years old when compared to men 60 to 64 years old, whereas in Spain the proportion of cases for men 80 years and older increases 44% compared to that of men 60 to 69 years old; in France the increase is 23% and in the United States it is 10% (Global Health 50/50, 2021). Although there is some relation between death proportion and case proportion among people older than 80 years in different countries, other reasons, such as the proportion of elder people living in nursing homes, might be relevant (Mallapaty, 2020).
Death rate difference between men and women of different ages will be discussed in following sections.
The number of cases relative to population in Mexico City peak at patients who are 51- to 60-year-old and then decreases, as shown in Table 1. It is noteworthy that proportion of COVID-19 cases is very low for people who are 20 years old or younger. Nevertheless, deaths relative to population increases steadily with age, peaking at patients 71- to 80-year-old. Although there is a lower-case proportion among older people, there is a higher death proportion among them. Therefore, death to case ratio is very much age related; while less than 1% of COVID-19 patients in Mexico City under 20 had died, 42% of patients older than 80 had died. Studies about European COVID-19 patients (Ahrendfelt et al., 2020; Mallapaty, 2020) agree with the finding that older people are at higher risk than younger people.
Table 1 Case/population, death/population, and death/case ratio by age range of COVID-19 patients in Mexico City.
| AGE RANGE | CASES/ 100,000 INHABITANTS |
DEATHS/ 100,000 INHABITANTS |
DEATHS/ CASES | ||
| 0-20 | 146 | 1 | 1% | ||
| 21-30 | 734 | 9 | 1% | ||
| 3"0 | 1,099 | 28 | 3% | ||
| 41-50 | 1,206 | 77 | 6% | ||
| 51-60 | 1,271 | 166 | 13% | ||
| 61-70 | 1,071 | 279 | 26% | ||
| 71-80 | 981 | 336 | 34% | ||
| 81-100 | 761 | 320 | 42% |
Source: Elaborated by the author with data from Sistema Nacional de Vigilancia Epidemiológica
The effect of gender
Men and women do not get sick and die from COVID-19 in the same proportion, according to information available and displayed in Table 2. It shows that proportion of men older than 20 that get infected from COVID-19 is larger than the proportion of infected women with their same age, as seen in left side columns. This finding is opposed to the meta-analysis of COVID-19 cases around the world (Peckham et al., 2020) that concludes that men and women have the same infection rate.
Table 2 Case and death proportions by gender and age range of COVID-19 patients in Mexico City.
| CASES/100,000 INHABITANTS |
DEATHS/100,000 INHABITANTS |
DEATH/CASE RATIO | ||||||||
| AGE RANGE |
MEN | WOMEN | AGE RANGE |
MEN | WOMEN | AGE RANGE |
MEN | WOMEN | ||
| 0-20 | 143 | 149 | 0-20 | 1 | 1 | 0-20 | 1% | 1% | ||
| 21-30 | 764 | 706 | 21-30 | 13 | 5 | 21-30 | 2% | 1% | ||
| 3"0 | 1,227 | 983 | 3"0 | 39 | 17 | 31-40 | 3% | 2% | ||
| 41-50 | 1,373 | 1,064 | 41-50 | 119 | 42 | 41-50 | 9% | 4% | ||
| 51-60 | 1,513 | 1,069 | 51-60 | 269 | 80 | 51-60 | 18% | 8% | ||
| 61-70 | 1,389 | 823 | 61-70 | 420 | 168 | 61-70 | 30% | 20% | ||
| 71-80 | 1,266 | 768 | 71-80 | 512 | 205 | 71-80 | 40% | 27% | ||
| 81-100 | 1,058 | 590 | 81-100 | 498 | 217 | 81-100 | 47% | 37% | ||
Source: Elaborated by the author with data from Sistema Nacional de Vigilancia Epidemiológica.
Death among men as proportion of male population is even larger than that of women, as shown in central columns of Table 2. Indeed, male COVID-19 patients die at a higher proportion than women for all ages above 20 years old as proportion of cases, such difference being larger than 10% among their own gender for all age ranges over 50 years old, as shown in right side columns of Table 2. The strong increase in death proportion is in correspondence with age as discussed before. Such trend and the strong difference in death proportion between men and women is clear and should be considered to implement the appropriate public policies and personal decisions. Studies about European COVID-19 patients (Ahrendfelt et al., 2020; Mallapaty, 2020) also find that men are at higher risk than women. Data about U.S. COVID-19 patients (Harvard GenderSci Lab, 2021) and the meta-analysis made by Peckham et al. (2020) of a large number of studies around the world, also support the finding that male patients have higher mortality than female patients. One study of COVID-19 patients in India (Dehingia y Raj, 2020) reports a higher mortality among women than among men.
There are several hypotheses for such difference in death proportion between men and women. The first hypothesis is that the difference is biological since testosterone in men reduce their immune response whereas estrogen in women have a protective effect (Peckham et al., 2020; Capuano et al., 2020). Another hypothesis is that mortality difference is due to habits, for example, that men wash their hands less frequently (Peckham et al., 2020) and that men smoke and drink more than women (Capuano et al., 2020). A third hypothesis, being that men have a higher frequency of previous health conditions (Ahrendfelt et al., 2020; Capuano et al., 2020; Peckham et al., 2020), will be discussed below.
The effect of previous health conditions
In an article published by Forbes, Flannery (2020) tries to minimize the effect of previous health conditions on death rate among COVID-19 patients in Mexico. However, according to the available information, 70% of those who died had a previous health condition. It is difficult to measure accurately the relationship between previous health conditions and death rate because available data does not include the severity of health conditions, for example, glucose level is unknown for diabetic patients and body mass index is unknown for obese patients.
Fig. 2 shows that proportion of COVID-19 patients with previous health condition increases steadily with age from 20% for patients 0 to 20 years old to more than 70% for patients above 70 years old. However, the proportion of COVID-19 patients with a previous health condition that die starts at 50% for patients 0 to 20 years old, growing to 70% or more for patients over 50 years old. This means that a previous health condition is quite an important cause of death among younger patients but becomes almost irrelevant for those over 70 years old.
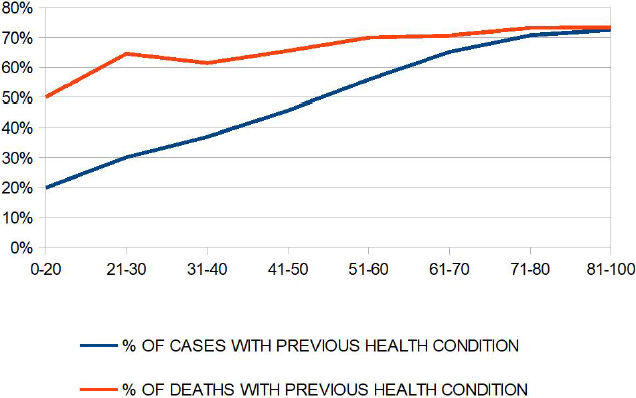
Source: Elaborated by the author with data from Sistema Nacional de Vigilancia Epidemiológica
Fig. 2 Proportion of cases and deaths with previous health condition of COVID-19 patients in Mexico City.
As discussed before, the proportion of people that get COVID-19 and die is larger for men than for women at almost any age. Such difference persists when accounting for previous health condition, as shown in Table 3. Men over 20 years old have a much higher death rate than women, both for people with previous health conditions and for those without them. It is noteworthy that male patients over 50 years old without any previous health condition have a higher death ratio than female patients their same age who do have some previous health condition. This finding is contrary to the hypothesis by Ahrendfelt et al. (2020) that male European COVID-19 patients have a higher mortality rate than female patients because men have a higher proportion of previous health conditions than women.
Table 3 Death/case ratio by gender, age range and health condition of COVID-19 patients in Mexico City.
| AGE RANGE | MEN
WITH PREVIOUS HEALTH CONDITION |
MEN WITHOUT PREVIOUS HEALTH CONDITION |
WOMEN WITH PREVIOUS HEALTH CONDITION |
WOMEN WITHOUT PREVIOUS HEALTH CONDITION |
| 0-20 | 1.5% | 0.6% | 2.6% | 0.4% |
| 21-30 | 4% | 0.7% | 1.3% | 0.5% |
| 31-40 | 5% | 2% | 3% | 1.1% |
| 41-50 | 12% | 6% | 6% | 2% |
| 51-60 | 22% | 12% | 10% | 5% |
| 61-70 | 33% | 26% | 23% | 16% |
| 71-80 | 42% | 37% | 28% | 23% |
| 81-100 | 50% | 41% | 36% | 40% |
Source: Elaborated by the author with data from Sistema Nacional de Vigilancia Epidemiológica
Not all previous health conditions affect COVID-19 patients the same way. Left side columns of Table 4 show the percentage of COVID-19 cases that had a previous health condition, right side columns show the percentage of these COVID-19 cases with a previous health condition that died. It can be observed that diabetes, hypertension, obesity, and smoking are the most frequent previous health conditions among COVID-19 patients. From the public policy point of view, it is clear that these most common health conditions require more attention, nevertheless, it is important that patients suffering from less common conditions know of their individual risk of death if they get COVID-19.
Table 4 Case proportion and death/case ratio by gender and previous health condition of COVID-19 patients in Mexico City.
| CASE PROPORTION | DEATH/CASE RATIO | ||||
| BY GENDER AND PREVIOUS HEALTH CONDITION | |||||
| PREVIOUS
HEALTH CONDITION |
MEN | WOMEN | MEN | WOMEN | |
| OBESITY | 18% | 21% | 17% | 10% | |
| HYPERTENSION | 16% | 18% | 28% | 18% | |
| DIABETES | 15% | 14% | 29% | 18% | |
| SMOKING | 13% | 7% | 12% | 6% | |
| NON
SPECIFIED CONDITION |
2% | 3% | 27% | 11% | |
| ASTHMA | 2% | 3% | 10% | 6% | |
| HEART DISEASE | 2% | 2% | 28% | 21% | |
| CHRONIC
KIDNEY FAILURE |
2% | 2% | 39% | 30% | |
| IMMUNOSUPPRESSED | 1% | 2% | 34% | 17% | |
| CHRONIC
OBSTRUCTIVE PULMONARY DISEASE |
1% | 1% | 36% | 23% | |
| PREGNANCY | 1% | 1% | |||
| HIV/AIDS | 1% | 0% | 14% | 5% | |
| SOME
PREVIOUS HEALTH CONDITION |
46% | 46% | 19% | 11% | |
| NO PREVIOUS
HEALTH CONDITION |
54% | 54% | 8% | 3% | |
Source: Elaborated by the author with data from Sistema Nacional de Vigilancia Epidemiológica.
Obesity is the most frequent previous health condition among COVID-19 patients and has a high proportion of deaths to cases. Onorato et al. (2020) found four studies regarding the effect of obesity on mortality of COVID-19 patients in the United States and the United Kingdom, all of them concluding that obesity is related to the risk of death.
Hypertension and diabetes are two previous health conditions that appear with high frequency among COVID-19 patients that are a greater death risk. For example, 16% of male COVID-19 patients have hypertension and 28% of them died.
A meta-analysis made by Du et al. (2021), that included 24 studies from China, United States, Mexico, and Israel, indicates that 46% of COVID-19 patients that died had hypertension while 22% of COVID-19 patients that survived did. They conclude that hypertension is an independent risk factor for COVID-19 mortality.
A meta-analysis made by Wu et al. (2020), that included 9 studies in China, concludes that diabetes increases the mortality of COVID-19 patients.
Noteworthy, COVID-19 patients with some less common previous health conditions have an even higher death rate, the top being chronic kidney failure (CKD) with 39% death rate for male patients, followed by chronic obstructive pulmonary disease (COPD) with 36% death rate for male patients and by those who have been immunosuppressed with 34% death rate, also for male patients. A meta-analysis by Cai et al. (2021) agrees with the finding that death risk is higher for COVID-19 patients with chronic kidney failure. Likewise, a study in South Korea (Lee et al., 2021) agrees with the finding that chronic obstructive pulmonary disease is an independent cause of death among COVID-19 patients. However, a press release by the Johns Hopkins School of Public Health (2021) regarding American immunosuppressed patients, is opposite to this study´s finding that immunosuppressed COVID-19 patients have a higher death risk.
Fortunately, a very low death rate among pregnant COVID-19 patients is observed.
The percentage of male patients that smoke is about twice as large as that of female patients and the death rate is also about twice as large. This evidence supports the hypothesis that a higher percentage of male COVID-19 patients die because they smoke more than women (Ahrendfelt et al., 2020) but also shows evidence of the combined effect of gender and smoking as death risks.
Combined effect of age, gender, and previous health conditions
It must be considered that age is still a very important factor of death among patients the same gender and with the same previous health condition, as exemplified in Figs. 3 a) and 3 b) which show the effect of the three factors for the most common previous health conditions for male and female COVID-19 patients. The shape of the curves for the same previous health condition is very different for men and women: for men, mortality rate grows steadily for each age range but, for women, the rate stays almost flat for patients up to 60 years old, but then climbs steeply. It is observed that:
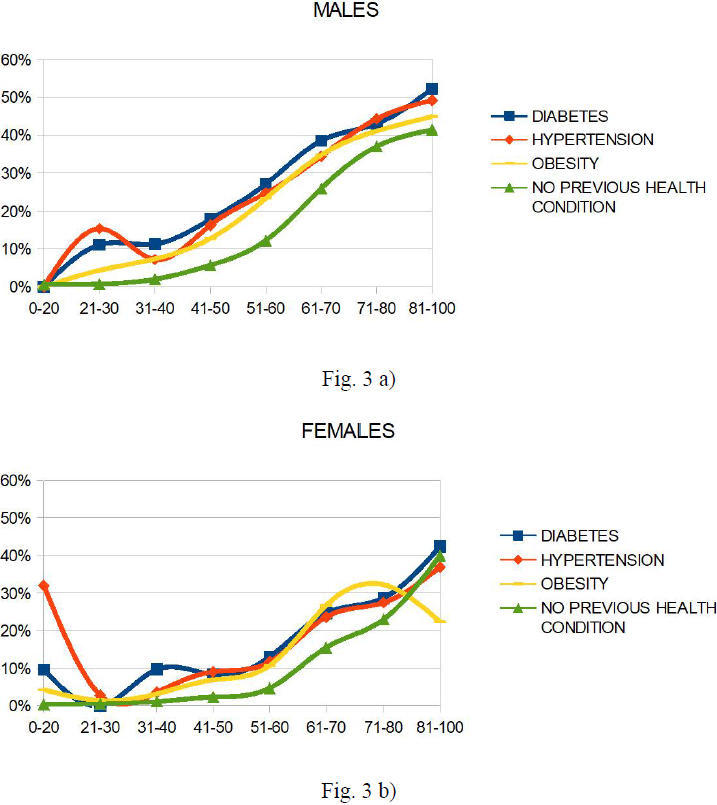
Source: Elaborated by the author with data from Sistema Nacional de Vigilancia Epidemiológica
Figs. 3 a) y b). Death/case rate for 3 a) males and 3 b) females by age range and most common previous health condition of COVID-19 patients in Mexico City.
The risk of dying for people with or without previous health conditions, increases with age with very few exceptions, such as: males 21 to 30 years old with hypertension have an unexpectedly high mortality rate and, very young women with hypertension have an even higher mortality rate than women with hypertension who are 71 to 80 years old.
The risk is higher for men than for women at almost all age ranges for all diseases shown. For example, while 43% of COVID-19 male patients 51 to 60 years old with diabetes died, 29% female patients the same age with diabetes did.
Patients with any of the most common previous health conditions have a much higher probability of dying than those without previous health conditions; for example, while 25% of COVID-19 male patients 51 to 60 years old with hypertension died, 12% male patients the same age without any previous health conditions did.
A study made with data from Mexican patients at Instituto Mexicano del Seguro Social (Escobedo-de la Peña, Rascón-Pacheco et al., 2020) surprisingly found a much lower difference in the percentage of patients that die between those with a previous health disease and those without it. An analysis of their results combining hospitalized and non-hospitalized patients, finds for example, that while 23% of COVID-19 male patients 50 to 59 years old with hypertension died, 20% male patients the same age without any previous health conditions did. Their result for death rate among patients with hypertension is similar to that found in this study, but their result for patients without a previous health condition is much lower than that found in this study. Further research could be done to explain disparities between data from Sistema Nacional de Vigilancia Epidemiológica and from Instituto Mexicano del Seguro Social.
Conclusion
Outcome of COVID-19 patients among Mexico City population depends of several causes, so that knowing their effect is fundamental in order to suggest and implement the right public policies. According to the information available and analyzed in this work, age, gender, and previous health condition are important causes for death rate among COVID-19 patients. The older the patient the higher its risk, this finding is consistent with studies in Europe. Men with COVID-19 have a much higher death risk than women, which is consistent with studies in Europe and data from the United States for reasons suspected to be biological or due to habits, but not because of gender difference in the prevalence of previous health conditions. COVID-19 patients with hypertension, diabetes, chronic kidney failure, chronic obstructive pulmonary disease and those immunosuppressed or with heart disease have a much larger death rate than other COVID-19 patients. Death risk for these previous health conditions is confirmed by studies in Europe, the United States and China. Combination of the three forementioned risk factors result in very different mortality rates among COVID-19 patients and is, therefore, relevant for public policy and for personal decision making.











 nova página do texto(beta)
nova página do texto(beta)


