Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Journal of the Mexican Chemical Society
versión impresa ISSN 1870-249X
J. Mex. Chem. Soc vol.58 no.4 Ciudad de México oct./dic. 2014
Article
Biocompatibility Evaluation of Electrospun Scaffolds of Poly (L-Lactide) with Pure and Grafted Hydroxyapatite
Luis Jesús Villarreal-Gómez,1 Ricardo Vera-Graziano,2 María Raquel Vega-Ríos,3 José Luis Pineda-Camacho,3 Horacio Almanza-Reyes,3 Paris Astrid Mier-Maldonado,4 and José Manuel Cornejo-Bravo5,*
1 Centro de Ingeniería y Tecnología, Universidad Autónoma de Baja California, Valle de las Palmas, México.
2 Instituto de Investigaciones en Materiales, Universidad Nacional Autónoma de México, Ciudad Universitaria, Coyoacán 04510, D.F. México.
3 Facultad de Medicina y Psicología, Universidad Autónoma de Baja California, Tijuana, México.
4 Centro en Ciencias de la Salud, Universidad Autónoma de Baja California, Valle de las Palmas, México.
5 Facultad de Ciencias Químicas e Ingeniería, Universidad Autónoma de Baja California, Calzada Universidad 14418, Parque Industrial Internacional, Tijuana, México. jmcornejo@uabc.edu.mx
Received November 28th, 2013
Accepted July 7th, 2014.
Abstract
The objective of this work was to evaluate the biocompatibility of scaffolds of poly(L-lactide) with pure and grafted hydroxyapatite, at various concentrations of reinforcement. The biocompatibility tests were carried out in vivo in Wistar rats by implanting the material into the sub-cutaneous and muscle tissues from 1 to 14 weeks and evaluating the surrounding tissue stained with hematoxylin-eosin. For in vitro assays, MTT and neutral red assay were used to evaluate any cytotoxicity in Mioblast Muscle C2C12 Cells (ATCC® CRL-1772TM) and Bovine Coronary Artery Endothelial Cells (BCAEC); Escherichia coli and Staphylococcus aureus were used to evaluate bacterial adhesion. All variants of scaffolds provoked a mild inflammatory response, without showing necrosis. No evidence of cytotoxicity was presented in cell viability tests and good bacterial cell adhesion was visualized for all of the materials studied.
Key words: Biocompatibility, electrospun scaffolds, In vivo and In vitro assay, MTT assay, tissue regeneration, poly(L-lactide).
Resumen
El objetivo de este trabajo fue evaluar la biocompatibilidad de andamios de poli(L-lactida) con hidroxiapatita pura e injertada a varias concentraciones de refuerzo. Las pruebas de biocompatibilidad in vivo fueron llevadas a cabo en ratas Wistar implantando los materiales en tejido subcutáneo y muscular durante 1 a 14 semanas evaluando el tejido adyacente teñido con hematoxilina-eosina. Los ensayos MTT y rojo neutro fueron usados para evaluar alguna citotoxicidad en las líneas celulares musculares mioblásticas C2C12 (ATCC® CRL-1772TM) y células endoteliales de arteria coronaria bovina (BCAEC); y las bacterias E. coli y S. aureus fueron usadas para evaluar adhesión celular bacteriana. Todas las variantes de los andamios provocaron una respuesta inflamatoria suave, sin mostrar necrosis. No hubo evidencia de citotoxicidad presente en los ensayos de viabilidad celular y buena adherencia celular bacteriana fue visualizada en todos los materiales estudiados.
Palabras clave: Biocompatibilidad, andamios electrohilados, ensayos in vivo e in vitro, ensayo MTT, regeneración de tejido, poli(L-lactida).
Introduction
Elderly population and sedentary life due to increased life standards are two imminent factors that provoke decrease in bone mineral mass, bone quantity, and muscle strength in the body. Hence, there is an increasing incidence of bone fractures. Bone has a great regenerative capacity, but a proper healing of the bone requires appropriate alignment and fixation of fractured fragments throughout the process [1].
Fixation of osteotomized and fractured bone segments is achieved using internal rigid fixation devices including plates and screws, and the gold standard materials for these is titanium due to its inherent stiffness and biocompatibility. However, this everlasting stiffness may cause a stress-shielding phenomenon, resulting in osteoporotic bone and skeletal growth retardation in pediatric patients. However, in order to overcome the problems associated with metal fixation devices, a number of polymer-based biodegradable plates and screws were devised and a number of them are already available and have some clinical experience [2].
A strategy to accelerate the bone regeneration is the use of tissue engineering techniques for the production of functional bone segments [3, 4, 5]. "Tissue engineering is a field with the goal of mimics a biological tissue using a combination of cells, scaffolds and mechanical and biochemical stimuli. These tissues may be used to replace or restore the function to missing or damaged elements in the body" [6].
Among the main methods found in tissue engineering is the in vitro growth of cells of interest in a three-dimensional (3D) structure, shaped as the target organ or tissue. However, the cells do not possess the ability to grow in 3D orientations that define the anatomical shape of the tissue; instead, cells migrate to form random or two-dimensional (2D) layered fabrics. Despite this, the 3D structures are required, and this is accomplished by culturing the cells in three-dimensional porous structures known as "scaffolds", where the cells colonize and proliferate [7].
It can be enlisted a large number of synthetic or natural origin biodegradable polymers but only a few of them are suitable as implant materials to be used in hard tissue regeneration due to stringent mechanical property requirements. The most extensively studied biodegradable polymers as biomaterials for this purpose is the lactide/glycolide family of polymers and these efforts have resulted in the approval of their use within the human body by FDA. Different formulations of poly(glycolide) (PGA), poly(lactide) (PLA) and poly(lactideco-glycolide) (PLGA) have been studied extensively for this context [8, 9].
For the preparation of PLA, the monomer lactide is synthesized by dimerization of lactic acid and then the polymer is formed via ring opening polymerization. There are two lactide isomers, namely D and L forms. The stereopolymer poly(L-lactide) (PLLA) is semicrystalline, with a crystallinity of around 37% and has the highest inherent tensile strength and modulus of elasticity among polylactides [1].
PLLA and other biodegradable materials such as poly(ε-caprolactone) (PCL) have been combined with hydroxyapatite (HA), to take advantage of the osteoconductive characteristics of this bioceramic, to prepare scaffolds using the electrospinning technique. The scaffolds produced are porous (microfibrous) materials that mimic the bone extracellular matrix and show active cellular attachment and proliferation [10].
However, there is a poor interaction between PLLA and the bioceramic, and even when HA is a rigid material there is not an increase on the mechanical properties of the mixtures compared to pure PLLA. Besides, there is the risk of the formation of clusters of HA leaving zones with low content of the active material, decreasing the citocompatibility of the scaffolds [11, 12, 13].
To increase the compatibility between PLLA and HA, Vera-Graziano et al. grafted PLLA to HA nanoparticles, and such grafted material was mixed with PLLA to prepare electrospun scaffolds. The scaffolds at different concentrations of reinforcement (HA) have good mechanical and in vitro biological properties. Especially the material containing 4% of PLLA-grafted HA, which has the best properties, in comparison with higher concentrations of PLLA-grafted HA, and the scaffolds made of mixtures with non-grafted HA. The biological properties of the scaffolds were studied by cell adhesion of mesenchymal stem cells through immunofluorescence tests [14].
This work was undertaken to evaluate the in vitro biocompatibility of microfibers made of mixtures of PLLA with non-grafted HA, (PLLA/HA) and grafted HA (PLLA/PLLA-g-HA), on C2C12 and BCAEC cell lines, also in Escherichia coli and Staphylococcus aureus, to demonstrate the non-toxicity on different cell types. Likewise, in vivo biocompatibility studies were performed in two different tissues of Wistar rats. Hopefully, these results will lead to the third stage of biocompatibility investigation as suggested by the current international toxicity standards, hence to evaluate the usefulness of the scaffolds to regenerate in vivo bone and dentin tissues. These materials are proposed to be used in hard tissue regeneration including dental obturations.
Results and discussion
Biocompatibility of microfibers scaffolds of PLLA-g-HA or PLLA/HA
MTT assay and neutral red assay
Figure 1 shows MTT and neutral red results. It can be appreciated that in both the MTT assay and the neutral red incorporation assay, none of the eight variants evaluated showed a decrease in cell activity in C2C12 cells or BCAEC cells, compared to negative controls, which represent 100% of cell growth. Even it can be seen that most of the scaffold promote cell proliferation because absorbance obtained higher than the control, indicating a greater presence in mitochondrial activity and endocytic process in cells. In three of the four tests showed that PLLA/HA30 scaffolds are able to increase the cell growth at 20% higher than the control. Likewise, the scaffolds PLLA/HA4 increases a 27% cell growth for C2C12 cells. The ANOVA test of the results indicate there is not a significant difference between the effects caused by the materials in the exposed cells (P > 0.05).
MTT assay and neutral red assay confirmed that all scaffolds supported normal cellular mitochondrial metabolic and endocytic activity without inducing cytotoxic events. This may be the result, besides of chemical composition of the scaffolds, of their microporous architecture with a porous area of about 67%. It has been demonstrated that PLLA and hydroxyapatite are biocompatible [15]. Also the biocompatibility has been reported in hydroxyapatite scaffolds made by 3D printing where cytotoxicity tests were carried out according to DIN ISO 10993-5 in static and dynamic cultivation setups. Good cell viability as well as good proliferation behavior was found [16]. Despite the similarity of the studied scaffold with our materials, this procedure for fiber formation was very different since the electrospinning method was used for the materials under study. Even when the biocompatibility of PLLA scaffold has been well documented, the purpose of assessing the biocompatibility of the PLLA/HA and PLLA/PLLA-g-HA scaffolds in this work was to determine if the fabrication method is dependable. It should be noted that the compatibility of the material even if they are very similar may depend of the way they are processed and its dimensions, especially when it comes to nanoscale materials as the diameter of the nanofibers and nanoparticles of HA studied here. Another important factor is the origin of the materials, where and how they were obtained. These are sensitive issues when materials are to be applied in biomedicine. Despite that PLLA scaffolds and hydroxyapatite scaffolds have been reported individually as biocompatible materials, it is important to asses if as composite the scaffolds present the same tissue response. For example, coelectrospun polylactide (PLA)/gelatin (GE) composite fibrous matrixes have been identified to exhibit much improved performances compared to the respective components [17]. In the scaffolds under our study no preferential position tendency of the cells onto the scaffold fibers was observed suggesting that the cell morphology is independent of the topography of the fibers. This observation is relevant because roughness may lead to the morphology and position of the cells in a scaffold [14].
Our results demonstrated that PLLA/HA and PLLA/PLLA-g-HA scaffolds are good substrates for cell proliferation independently of HA proportion, as seen in Figure 1, even some of them enhanced growth population. For example: PLLA/HA4, PLLA/HA30 and PLLA/PLLA-g-HA30 scaffolds showed an increment in cell growth of 27%, 10% and 19%, respectively, in C2C12 cells; and PLLA-g-HA30, PLLA/HA10, PLLA/PLLA-g-HA10, PLLA/PLLA-g-HA20 and PLLA/HA30 scaffolds showed an increment in cell growth of 23%, 12%, 10%, 10% and 20%, respectively, in BCAEC cells. Such results have been seen in experiments evaluating electrospun poly (L-lactide-coglicolide) (PLGA) scaffolds, which increased cell growth by 50% compared to other scaffolds [18].
Bacterial adhesion
Materials with a high antibacterial capacity frequently induce severe side effects during and after endodontic treatment, as well as being cytotoxic and mutagenic [19]. For the materials under study we did not see any evidence of bacterial growth inhibition, at the contrary; we observed bacterial monolayer formation over the scaffolds.
Regarding the diffusion study to determine the bacterial cell absorbance of the scaffolds, a significant difference between initial and final absorbances in all samples (Figure 2) was observed, which indicate that all materials absorb or/and adsorb bacterial cells. Both E. coli and S. aureus showed greater cell retention after 5 minutes of incubation. Results obtained are similar to those observed in other biocompatible scaffold materials such as chitosan and gelatin [20].
Both of the bacterial assays shows that all PLLA/PLLA-g-HA and PLLA/HA scaffolds are excellent substrates that enable efficient bacterial cell adhesion. The results are in accordance with the good bioadhesive properties for eukaryotic cells previously observed [14]. We can resume that to promote bacterial adhesion the substrate need to be hydrophobic, and for cellular protein adhesion the substrate has to be hydrophilic. PLLA is a highly hydrophobic polymer, which retain bacteria cells [21], and, apparently, the polar groups of HA promote the adhesion of eukaryotic cells. Bacterial adhesion is an expected event that needs to be prevented for some applications and that is why some formulations are loaded with antibiotics. Therefore, non bacterial adhesion will be more relevant.
After the test materials were extracted no signs of irritability or necrosis in the subcutaneous surrounding area were found (Figure 3). However, it was observed that all samples provoke immune system recognition during the first 5 days after implantation of the test materials (Table 1); polymorph nuclear cells, lymphocytes and plasma cells were found. These cells are present in swollen areas and in the formation of a foreign body granulomatous swelling; however, after 5 days no presence of granulomas was found. As an observation, samples PLLA/PLLA-g-HA20 and PLLA/PLLA-g-HA4 have no evidence of a tissue response against the materials. After 33 days of implantation, adipose tissue and giant cells can be found in most samples, except for PLLA/HA30, which have no evidence of tissue response. The presence of giant cells (fused macrophages) indicates the detection of a foreign body and high phagocytic activity; it means that macrophages tried to digest the material. On the other hand, it was found the presence of fibrous tissue encapsulation in sample PLLA/PLLA-g-HA10 after 33 days of implantation; and, PLLA/PLLA-g-HA30 showed to be encapsulated after 99 days. Later, at 99 days, giant cells remained present around most of the scaffolds, except for PLLA/HA10 and PLLA/HA4 where these giant cells are no longer present. Finally, necrotic tissue was present at 5, 33 and 99 days for the positive control, demonstrating that the sterile gauze causes a persistent immune response.
Figure 3 shows the scaffolding extractions at 99 days after implantation in the subcutaneous tissue, it can be seen that in all cases there is a coating of adipose tissue but because neither erythema nor redness adjacent to the material, this suggests tolerance by the body to the materials, keeping them isolated from the surrounding tissue.
Muscle implantation test
After the test materials were extracted, there were no signs of irritability or necrosis in the surrounding tissues; they looked healthy and normal. The presence of striated muscles was observed after 47 and 96 days after scaffold implantation. In histological smears, we found the presence of adipose tissue in the sample PLLA/HA20 at 47 and 96 days after the material was implanted. At the contrary, the samples PLLA/HA10, PLLA/HA4 showed presence of adipose tissue after 96 days of surgery but not at 47 days. The presence of adipose tissue was found during both microscopic and macroscopic observations in PLLA/HA4, PLLA/HA10, and PLLA/HA20. A membrane coating of fat was observed in all samples, suggesting that both PLLA/HA and PLLA/PLLA-g-HA scaffolds are compatible materials in muscle.
Despite these findings, at 47 days there were giant cells, and fibrous tissue encapsulation in most samples except for PLLA/ PLLA-g-HA10 and PLLA/PLLA-g-HA20 scaffolds. At 96 days the cells were present in the samples PLLA/HA4, PLLA/HA10 and PLLA/PLLA-g-HA10, lack of response in PLLA/PLLA-g-HA20 and PLLA/HA30 scaffold and encapsulation by fibrous tissue in the samples PLLA/PLLA-g-HA4, PLLA/HA20 and PLLA/PLLA-g-HA20. Also, we noted that three samples that showed the presence of adipose tissue also showed encapsulation by fibrous tissue, which evidences the close relationship between adipose tissue to synthesize adipokines and recruitment of fibroblasts to the site of the implant to form the capsule. The only sample that showed granuloma and necrosis was PLLA/HA4 in muscle tissue after 96 days of being implanted. The presence of fibrous tissue capsule, lymphocytes and giant cells suggest that the immune system recognize PLLA/PLLA-g-HA and PLLA/HA scaffolds similarly, and elicited an encapsulation of the material to try to degrade and phagocyte the implants (Table 2).
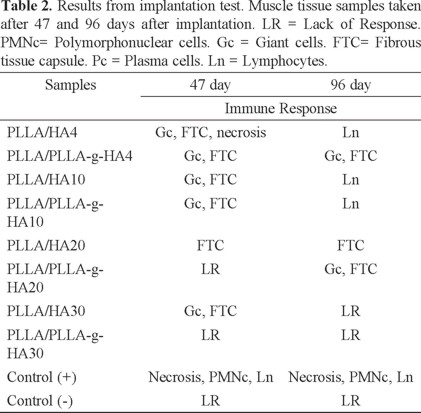
Figure 4, represents the tissue response provoked by all the microfibers of the different scaffolds, it can be seen giant cells trying to phagocyte the microfibers (Figure 4; a and b), this figure also shows how fibroblast cells are surrounding around microfiber isolating the scaffolds from other tissue (Figure 4; a); however, fibroblast cell penetrate the scaffolds, visualizing them inside, demonstrating the correct proportion and size of porous in the scaffolds (Figure 4; a). Finally we show how a normal tissue looks (Figure 4; c) and how looks a necrotic tissue provoked by a toxic material (Figure 4; d).
PLLA have been evaluated in vivo previously. For example, Anderson and Shive reported that local or systemic administration of microspheres made of PLA and PGLA containing insulin does not give rise to any adverse reaction in vivo [22].
Based on this evaluation scale in Table 3, the inflammatory immune response caused by PLLA/HA and PLLA/PLLA-g-HA scaffolds after 1 to 14 weeks of implantation ranged from level 2 to 3 (mild to moderate immune response).

The presence of adipose tissue is related to the same immune system response, although it is important to note that the mechanisms that link adipose tissue of the immune response is not fully understood [3]. But previous investigation showed that non-reactive and biocompatible materials present a membrane encapsulation of adipose tissue, while incompatible materials did not present this phenomenon [23].
In our study, all implanted materials were encapsulated with adipose tissue. According to the previous publications there is strong evidence that PLLA/HA and PLLA/PLLA-g-HA scaffolds are biocompatible.
Some authors suggest that the presence of granuloma in implanted materials does not always imply an incompatibility with the host tissues [7]. Such is the case of Branislav & Mirjana, who investigated the biocompatibility of different dental materials, intended for dental root canal obturation, by implantation in rat muscle tissue, through the analysis of different levels of inflammation of muscle tissue. That research used three different materials to be implanted in Biceps Femoris of Wistar Rat, the materials were Sealapex (Kerr, Romulus, USA), AH-26 (De Trey, Zurich, Switzerland) and Spongio cementitious material based on poly(methyl methacrylate) (PMMA) (U.S. patent 4,296,209), and sterile wax was used as a control. The implantation of Sealapex provoked a strong acute inflammation, infiltration with massive presence of polymorphonuclear and giant cells; likewise, AH-26 produced a strong reaction around the foreign body with lymphocytic infiltration. The presence of giant cells and macrophages shows evidence of high phagocytic activity. Otherwise, the implanted PMMA showed the formation of a fibrous connective tissue capsule consisting of fibroblasts and fibrocytes around the material, after granulation tissue is formed. The reaction found was very similar to the control reaction produced by the inert sterile wax. With these findings, researchers suggest biocompatibility of PMMA [24].
The researches had the concern that the formation of foreign body granuloma may inhibit bone formation; however, the inhibition was not observed, whereas the presence of an inflammatory reaction was mild and did not interfere with the process of bone formation in groups of rabbits implanted with micro and macrogranular bone matrix [25]. This statement is based on the fact that some multinucleated giant cells are closely related to the particle surface, showing evidence of a reabsorbing activity.
Consequently, another important observation in our study was the presence of a granuloma of foreign body in all samples at different times of material extraction. The above results suggest that the formation of foreign body granuloma is a normal immune response to implanted materials; inert materials are considered biocompatible materials that do not cause tissue necrosis.
Finally, it is important to mention, as an observation, that PLLA/HA and PLLA/PLLA-g-HA scaffolds degrade rapidly in subcutaneous and muscle tissue, because of its PLLA fraction; this has been demonstrated by Gong et al. They observed that porous PLLA scaffolds degrade in PBS (pH 7.4) at 37oC in vitro at a relatively slow rate in chondrocytes cells. Different from the exponential degradation of bulk material, they found that the molecular weight decreases linearly as a function of degradation time. Despite this, the degradation rate is accelerated in vivo. After 120 days of culture subcutaneously in nude mice, most of the scaffold has disappeared. The regions initially occupied by the polymer scaffold are filled with collagen type II, with no evident basophilic proteoglycan. The scaffold is also unable to maintain its predesigned shape after a long period of implantation, due to the weakening of the mechanical strength of the construct [26].
In vivo statistical analysis
Samples were compared across the box and whisker plot calculated by Minitab® software (data not shown). Samples have no significant difference with each other sample for causing the tissue response as indicated by the ANOVA test (P > 0.05). On the other hand, comparing to the negative control samples, the sample that caused the less immune response is the PLLA/PLLA-g-HA30 and the one that caused a more evident immune response was PLLA/HA20. Notably, none of the variants of the scaffolds, even in any of the samples taken at different times and places of implantation caused apparent necrosis.
Conclusions
In vitro and in vivo tests were performed in PLLA/HA and PLLA/PLLA-g-HA scaffolds. For In vitro evaluation were used C2C12 and BCAEC cell lines to evaluate any cytotoxicity, and the bacteria Escherichia coli and Staphylococcus aureus were used to evaluate bacterial adhesion. Results showed that none of the scaffolds evaluated present any cytotoxicity, in neither cell lines nor bacterial cells. The in vivo biocompatibility of electrospun PLLA/HA and PLLA/PLLA-g-HA scaffolds after 1 to 14 weeks of implantation in Wistar rats was evaluated in this study. A mild immune response was observed in all samples, which included a fibrous tissue encapsulation and giant cells presence. Nevertheless, there was no presence of tissue damage, necrosis or textiloma, these is good insight to decide the biocompatibility of the studied scaffolds. Also there is not a significant difference of reaction between the different porous fibrous scaffolds; the different proportion of pure and grafted hydroxyapatite apparently do not cause effect in the tissue reaction. It is important to mention that the scaffold PLLA/PLLA-g-HA4 has the best mechanical properties as well as a good biological response for hard tissue regeneration. These results provide valuable information for continuing studies to determine the effectiveness of the scaffolds for bone tissue regeneration.
Experimental
All tests were made according to the biocompatibility testing matrix suggested by the FDA and ISO 10993-1 [27]. According to such testing matrix, biocompatibility tests are the same for scaffolds intended for hard or soft tissue regeneration. Moreover, according to Autian [28], biocompatibility is proposed as a "concept" consisting of three levels: a) non-specific toxicity (cell cultures or small laboratory animals), b) specific toxicity (evidence of use, such as in primates), and c) human clinical trials. Based on this reference, we developed phase a): the required testing previous to experiments in teeth or bone, (usability testing).
Materials tested
The preparation of the materials tested was previously reported by Vera-Graziano et al. [14]. Commercially available hydroxyapatite nanoparticles (Aldrich Chem. Co.) were used as the starting material to polymerize L-lactide, without catalyst. PLLA grafting of 1.81% was obtained. Infrared and nuclear magnetic resonance spectroscopies indicate the formation of a chemical link between the components through the carboxylate ion signals. Solutions of PLLA, obtained by a non-catalyzed ring opening polymerization reaction, were prepared with different proportions of pure and PLLA-grafted HA and used to construct scaffolds by electrospinning. The scaffolds were intensively characterized including their mechanical properties. The software Image J was used to analyze SEM images (retrodispersive method) of the scaffolds and determine the average diameter of the fibers and the percentage of porous area.
Such materials were evaluated for biocompatibility in the present work. The samples were named according to the concentration of pure HA: PLLA/HA4, PLLA/HA10, PLLA/HA20 and PLLA/HA30. Samples containing PLLA-grafted HA nanoparticles were named: PLLA/PLLA-g-HA4, PLLA/PLLA-g-HA10, PLLA/PLLA-g-HA20 and PLLA/PLLA-g-HA30, respectively. The number in each sample represents the weight percentage of hydroxyapatite.
Figure 5 shows representative SEM images of the scaffolds. It can be observed that the distribution of HA is better in the PLLA/PLLA-g-HA scaffolds than in the PLLA/HA scaffolds. The average diameters of the fibers and of porous areas of the scaffolds studied are presented in Table 4. Average fibers diameters and porous areas are very similar for all the scaffolds, except for PLLA/PLLA-g-HA30 scaffold that has smaller fiber diameter.


In vitro assays
MTT and Neutral Red assays
The samples were sterilized by ultraviolet (UV) light exposure under a laminar flow hood for 30 minutes on each side, and placed in DMEM for one day. Mioblast muscle C2C12 cells (ATCC® CRL-1772TM) and Bovine Coronary Artery Endothelial Cells (BCAEC), supplemented for Francisco Villarreal, UCSD School of Medicine, San Diego, California, USA, were used for culturing. The cells were cultivated in DMEM, supplemented with 10% FBS and 100 U/mL penicillin-streptomycin-amphotercin, at 37°C in 5% CO2. The scaffolds were placed and immobilized in tissue culture microplates. Then, C2C12 and BCAEC cells suspended in culture medium (104 cells/mL) were added in the dishes to allow the in-growth of cells to the scaffolds. The polystyrene surface of cell culture microplates was used as a control. The MTT assay and neutral red assay were used for measurement of the cell viability and proliferation. C2C12 and BCAEC cells cultured on the scaffolds after 24 hrs of cell seeding were trypsinized, treated with 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (25 μL), (MTT), or neutral red stain, and incubated four hours at 37°C with 5% CO2. After incubation and adding DMSO, the viable cells were detected by measuring the absorbance of the cell lysates at 570 nm (A570) for MTT assay, and at 540 nm (A540) for neutral red assay, respectively. The cell viability was expressed by optical density (OD) of A570 and A540 of cells cultured on the scaffolds [29].
Bacterial adhesion
To evaluate the bacterial cell growth, scaffolds PLLA/PLLA-g-HA and PLLA/HA were placed in direct contact on bacterial cell cultures in petri dishes. If the material is not cytotoxic, the cells remain in contact with the material and continue to growth normally; on the other hand, if the material is cytotoxic, cell growth stops and an inhibition zone around the material is observed. Teflon was used as a negative control because it is an inert material. These tests were used to measure the antimicrobial activity of PLLA-g-HA and PLLA/HA on microorganisms as Staphylococcus aureus (ATCC® 6538PTM) and Escherichia coli (ATCC® 25922TM). The choice to use these organisms is because they are associated with extraoral wound infections, and in device failure of orthopaedic implants. For the purpose of evaluating whether PLLA/HA and PLLA/PLLA-g-HA scaffolds have a property to be absorbent, an assay was performed in which the different materials were placed at the bottom of sterile flat bottom 10 mL vials, and adding a cell suspension of Escherichia coli ATCC 25922 with an absorbance value of 0.905 and Staphylococcus aureus ATCC 25923 with 0.853 of absorbance. Bacterial cell suspensions were cultured in the presence of scaffolds for 5, 15 and 30 min at 37 oC. The absorbances of the cell suspensions at 420 nm for the different culture times were compared to the absorbance of the cell suspension before incubation in the presence of the scaffolds [30]. Experiments were done in triplicate.
In vivo assays
Test Animals
Twenty four 5-week-old Wistar Rats (Rattus norvegicus) with body weight of 100-300 g were used. The rats were housed one per cage and they had free access to tap water and standard pellet food (Furry Friends Pet Food®). All experiments were approved by the Bioethics Committee of the Medicine and Psychology Faculty, Autonomous University of Baja California, Mexico, with registration number IORG # IORG007487, of United States Department of Health and Human Services (HHS). Also, the experiments were conducted in accordance with the Mexican Legislation Standard of NOM-063-SSA1-1993, Ley General de Salud (Guide for the Care and Use of Laboratory Animals) [31].
In vivo scaffold implantation
For implantation tests, the rats were divided into five groups in total. Two zones for implantation of the test materials were selected: the dorsum subcutaneous skin and the muscle area of the Biceps Femoris. For implantation in subcutaneous skin (SS) 15 male Wistar rats were used, and divided in three groups depending on sample collecting time in days, SS5, SS33 and SS99, each group consisted in five rats; four rats were implanted with three variants of PLLA/HA scaffolds in different zones in dorsum and one with sterile gauze (+ control) and a sham (- control). For implantation (I) in muscle, 10 rats (200-300 g) were used, divided in two groups named as I47 and I96, depending on the days of evaluation after implantation, four rats were implanted with variants of PLLA/HA scaffolds in each leg (two variants per rat), and one with sterile gauze (+ control) in the left leg and a sham (- control) in the right leg.
Histological preparation and analysis
One to fourteen weeks after implantation, the rats were sacrificed using a glass bell containing gauze impregnated with chloroform. Each rat was put into the glass bell about 10 minutes until the rat lost consciousness and die. The implanted areas were dissected, and the implant-containing tissues were removed from the subcutaneous dorsum and the muscle of the Biceps Femoris of the rats. The tissues were immediately fixed with 10% formalin and embedded in paraffin wax, and then sectioned (4 mm) along the longitudinal axis of the implant. The sections were stained with hematoxylin and eosin (H&E); the slices were washed with PBS-T (phosphate buffered saline with Tween 20, 0.05%) and blocked with PBS containing 5% BSA (bovine serum albumin; Roche, Germany) for 1 h at 37 oC.
In Table 3 it is tabulated a scale for a qualitative evaluation of the inflammatory response in tissue, defining inflammatory response in levels from 1 to 4: level 1 corresponds to non-inflammatory response is observed; in this case the scaffolds do not stimulate any response. Level 2, when the immune response is smooth and implies the presence of macrophages and plasma cells; this means that the materials have been detected in local tissue and recruited macrophages to eliminate the foreign body, when macrophages phagocyte the microfibers, particles of the material are presented to B lymphocytes, which are converted into plasma cells. These cells produce a large quantity of antibodies that helps in the response against the materials. Level 3 is for moderate immune response, in addition to macrophages and plasma cells, neutrophils and lymphocytes capsules are observed; when materials provoke a lymphocytes capsule it is because macrophages cannot eliminate the foreign body, they fuse together and become giant cells, the tissue encapsulates the materials to isolate them from surrounding tissue. And, level 4 corresponds to severe inflammatory response and it includes areas of necrosis, all materials that cause necrosis are toxic and provoke aggressive secondary effects [24].
Statistics
Statistical analyses were performed using SPSS ® (SPSS Inc., Chicago, IL). To evaluate significance differences among groups, analysis of variance was performed with post hoc pairwise testing. A α level of 0.05 was selected for significance for all statistical tests.
Acknowledgments
Work supported by a grant from SEP-CONACYT (CB 2010-1-157173) and Dirección General de Asuntos del Personal Académico, UNAM (PAPIIT I IN108913).
References
1. Aydin, E.; Hasirci, V. J. Sib. Fed. Univ. 2010, 1, 3-17. [ Links ]
2. Deepak, S.; Manjula S. Int. J. Clin. Dent. Sci. 2011, 2, 38-43. [ Links ]
3. Sánchez, C.; Molina, M.J. In: Plásticos Aplicados en Medicina. Vol. 1, Ed., UNED, España, 2009, 1-364. [ Links ]
4. Sachlos, E.; Czernuszka, J.T. Eur. Cell Mater. 2003, 5, 29-40. [ Links ]
5. Velazco G. Acta Bioclin. 2011, 1, 1-2. [ Links ]
6. Athanasiou, K.A.; Sanchez-Adams, J. In: Engineering the Knee Meniscus, Vol 1, The Synthesis Lectures on Tissue Engineering. Ed., Morgan & Claypool Publishers. 2009, 1-36. [ Links ]
7. Pistòia, A.D.; Figueiredo, M.A.Z. Braz. Dent. J. 2002, 13, 103-108. [ Links ]
8. Patrício, T.; Domingos, M.; Gloria, A.; Bártolo, P. Procedia CIRP 2013, 5, 110-114. [ Links ]
9. Abedalwafa, M.; Wang, F.; Wang. L.; Li, C. Rev. Adv. Mater. Sci. 2013, 34, 123-140. [ Links ]
10. Fang, R.; Zhang, E.; Xu, L.; Wei, S. J. Nanosci. Nanotechnol. 2010, 10, 7747-7751. [ Links ]
11. Helwing, E.; Sander, B.; Gopp, O.; Vogt, F.; Wartewig, S.; Henning, S. Biomaterials 2001, 22, 2695-2702. [ Links ]
12. Sugiyama, N.; Kunibo, R,; Yoshizawa-Fujita, M.; Takeoka, T. Chem. Lett. 2007, 36, 1476-1477. [ Links ]
13. Hong, Z.; Zhang, P.; He, C.; Qui, X.; Lui, A.; Chen, L.; Chen, X.; Jung, X. Biomaterials 2005, 26, 6296-6304. [ Links ]
14. Vera-Graziano, R.; Maciel-Cerda, A.; Moreno-Rondon, E.V.; Ospina, A.; Gomez-Pachon, E.Y. Mater. Res. Soc. Symp. Proc. 2012, 1373, DOI: 10.1557/opl.2012.274. [ Links ]
15. Gong, Y.; Ma, Z.; Zhou, Q.; Li, J.; Gao, C.; Shen, J. J. Biomater. Sci. Polym. Ed. 2008, 19, 207-221. [ Links ]
16. Leukers, B.; Gulkan, H.; Irsen, S.H.; Milz, S.; Tille, C.; Seitz, H.; Schieker, M. Mat.-wiss. u. Werkstofftech. 2005, 36, 781-787 [ Links ]
17. Yang, X.; Xua, Q.; Yanb, N.; Suia, G.; Caia, Q.; Deng, X. Polym. Adv. Tech. 2010, 22, 2222-2230. [ Links ]
18. Zamani, F.; Amani-Tehran, M.; Latifi, M.; Shokrgozar, M.A. J. Mater. Sci. Mater. Med. 2013, 24, 1551-1560. [ Links ]
19. Nair, M.B.; Varma, K.; Kumary, T.V.; Suresh Babu, S.; John, A. Trends Biomater. Artif. Organs 2006, 19, 108-114. [ Links ]
20. Hima-Bindu, T.V.L.; Vidyavathi, M.; Kavitha, K.; Sastry, T.P.; Suresh-Kumar, R.V. Trends Biomater. Artif. Organs 2010, 24, 123-130. [ Links ]
21. Vrlinic, T.; Debarnot, D.; Mozetic, M.; Vesel, A.; Kovac, J.; Coudreuse, A.; Legeay, G.; Poncin-Epaillard, F. J. Colloid Interface Sci. 2011, 362, 300-310. [ Links ]
22. Anderson, J.M.; Shive, M.S. Adv. Drug Deliv. Rev. 1997, 28, 5-24. [ Links ]
23. Kaminski, E.J.; Shenk, M.W.; Oglesby, R.J. J. Biomed. Mater. Res. 1977, 11, 1097-4636. [ Links ]
24. Branislav, K.; Mirjana, V. Acta Vet. 2009, 59, 267-276. [ Links ]
25. Carneiro, E.; Garcia, R.B.; Oliveira, R.C.; Morales, F.G.; Menezes, R.; Letra, A.; Canova, G.; Calichio, C.; Tania, M.; Granjeiro, J.M. J. Appl. Oral Sci. 2005, 13, 157-162. [ Links ]
26. Gong, Y.; Zhou, Q.; Gao, C.; Shen, J. Acta Biomater. 2007, 3, 531-540. [ Links ]
27. ISO 10993-1:2003. Biological evaluation of medical devices - Part 1: Evaluation and testing. [ Links ]
28. Autian, J. Int. Dent. J. 1970, 20, 481-490. [ Links ]
29. Takamori, E.R.; Figueira, E.A.; Taga, R.; Sogayar, M.C.; Granjeiro, J.M. Braz. Dent. J. 2007, 18, 179-184. [ Links ]
30. Katsikogianni, M.; Missirlis, Y.F. Eur. Cell Mater. 2004, 8, 35-57. [ Links ]
31. Guide for the Care and Use of Laboratory Animals. The National Academies Press. 2011, 8. [ Links ]














