Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista odontológica mexicana
versão impressa ISSN 1870-199X
Rev. Odont. Mex vol.22 no.2 Ciudad de México Abr./Jun. 2018
Original research
Lower gravitational dentures: alternative treatment for atrophic ridges
* National Autonomous University of Mexico, School of Dentistry, Total Prosthodontics Clinic, Honorato Villa y Acosta Laboratory, Dental Biomaterials Laboratory, Graduate and Research School, National School of Dentistry, National Autonomous University of Mexico.
Stability of conventional lower prostheses (CP) is affected by excessive mandibular resorption, the greater weight of a gravitational prosthesis (GP) caused by its combination of metal (internal) and acrylic (external) can increase said stability. Objective: In patients with mandibular atrophic ridge, to compare stability, masticatory performance, weight and perception of CP in comparison with GP. Material and methods: Informed consent of six adult edentulous patients was requested. Residual lower ridge height was measured in mm. Identical CP and GP were manufactured for each patient: firstly, one was used, and then the other, each one for same periods of time. At the end of prostheses use, a Likert type survey was conducted, as well as analogous visual scale (AVS) measuring clinical stability (Woelfel scale), MP (particle mean size with artificial test foodstuff) as well as prostheses weight in grams. Wilcoxon ranking test was used as well as Spearman’s correlations (p = 0.05). Results: Significant differences were found in the clinical stability test (p = 0.046) favoring GP. Correlation among variables analysis indicates that to lesser movement, greater ease for speech and food processing was found. No statistically significant difference was found in MP (p = 0.893). Conclusions: In spite of limitations imposed by sample size, results indicated that GP were more stable and could represent a suitable treatment alternative for patients who are not candidates for surgery or suffer financial limitations.
Key words: Gravitational prosthesis; lower residual ridge atrophy; Woelfel scale; multiple screening method; prosthetic stability
La estabilidad de una prótesis convencional (PC) inferior se ve afectada por una excesiva resorción mandibular; el incremento de peso de una prótesis gravitacional (PG) por su combinación metal (interno) y acrílico (externo) puede aumentarla. Objetivo: Comparar la estabilidad, desempeño masticatorio (DM), peso y percepción del paciente con reborde atrófico mandibular de PC contra PG. Material y métodos: Se solicitó el consentimiento informado en seis adultos mayores desdentados. La altura del reborde residual inferior fue medida en mm. A cada paciente se le elaboró una PC y una PG (idénticas). Se utilizó primero una y luego la otra; cada una en periodos de tiempos iguales. Al término del uso de cada prótesis se le realizó una encuesta tipo Likert y una escala visual análoga (EVA), midiendo la estabilidad clínica (escala de Woelfel), DM (tamaño medio de partícula con el alimento prueba artificial) y el peso de las prótesis (g). Se utilizó la prueba de rangos de Wilcoxon y la evaluación de correlaciones de Spearman (p = 0.05). Resultados: La prueba clínica de estabilidad resultó con diferencia significativa (p = 0.046) a favor de la PG. El análisis de las correlaciones entre variables indica que a menor movimiento mayor facilidad en el habla y la reducción del alimento. En el DM no se obtuvo diferencia estadísticamente significativa (p = 0.893). Conclusiones: A pesar de la limitación del tamaño de la muestra los resultados indican que las PG son más estables y pueden ser buena alternativa de tratamiento para pacientes con limitaciones económicas o no candidatos a cirugía.
Palabras clave: Prótesis gravitacional; atrofia del reborde residual inferior; escala de Woelfel; método de tamizaje múltiple; estabilidad protésica
Introduction
All dentists must be aware of the feeling senior citizens experience with respect to the influence of their dental circumstances with their daily life, and request information on whether this affects their quality of life. These patients require competent and empathic professional care, even in cases when process might be difficult or lengthy, since state of mind bears enormous influence on patient’s interest in a prosthetic treatment.1-3 Mistakes and dissatisfactions arising in these treatments can have varied and complex causes, ranging from lack of communication between patient and dentists, to the dental technician’s performance of the full treatment. Success of a full prosthesis mainly depends on the base stability degree, which is a result of suitable retention elicited by preserved bone remnant, which must be prosthetically usable. In cases when bone ridges suffered marked resorption, the prosthetic triad of the denture will result compromised.4
When teeth are partially or totally lost, mastication, deglutition and food intake might be impaired, representing a risk factor for problems such a dyspepsia.5 When placing an artificial denture, masticatory ability is partially restored, and patients can preserve suitable nutrition. Nevertheless, proprioception offered by the periodontal ligament disappears, thus force is uncontrolled and moreover perception of food taste is distorted.6-8 Maximum masticatory load of full denture bearers is five to six times lesser in total denture users when compared to subject with natural teeth.2 Groups of patients not wearing dentures, either with teeth or partially edentulous, have been assessed in order to observe MP (degree of trituration a test foodstuff can be subjected to in a given number of masticatory strokes or cycles), or masticatory efficiency (number of additional masticatory strokes or cycles required to achieve suitable trituration by subjects who have lost system integrity).
Another factor subject to study was whether age interfered with the aforementioned parameters. It has been found that natural ageing of the human being is fully related to a decrease in masticatory muscular activity, which per force increases to double the number of masticatory cycles required for the formation of a suitable food bolus.2,6,9-11
MP can be measured in two different manners:
Subjectively: this method consists in inquiring about subject’s perception by means of questionnaires related to his masticatory ability.
Objectively: with the help of multiple techniques such as measurement of sugar loss in a chewing gum, the colometrical and photometric methods, optical scanning method of volumetric screening method.6,12
Foodstuffs used for objective evaluation can be natural (carrots, peanuts, soft bread among others) or artificial (heavy polymethylsiloxane). Artificial foodstuff is mostly used in order to circumvent great variation in results, since natural foodstuffs can exhibit variable physical properties (hardness, fracture resistance, size and shape).6,11
The method of multiple volumetric screening (Yurkstas and Manly 1950) measures the volume of artificial foodstuff particles, since they are made to traverse a tower of screens with different mesh openings.10
Hardness of artificial foodstuff (Optocal) is decreased for full denture wearers, contemplating as a base changes of mastication forces with what was previously described. Nevertheless, some authors report in their studies that this tablet is still inadequate for some full denture bearers.13-16
Structural weight plays an important role in prosthesis stability. In the upper jaw, a light denture will exert lesser displacement gravitational force: this is not the case for the lower jaw where slight overweight (30-40 g total) will favor settling within prosthetic limits.1,17 Patients wearing dentures frequently limit the load of supporting tissues by selecting foodstuffs not requiring masticatory effort to achieve tissue tolerance, moreover, due to tongue activity,18 lower dentures exhibit the flaw of not being retained during mastication. Patients will then have to resort to pharmaceutical lining which will compromise oral health.2,8
Since olden times «heavy weight» metallic bases have been used in full dentures, due to the following advantages: greater strength, lesser porosity, thermal conductivity, considerable tissue tolerance, and greater weight, causing thus better stability and lesser deformation. Nevertheless, their use has been discontinued due to the following reasons: they are costlier, more rigid, cause irritation, re-adaptation or rebase is complicated, and for lower bases, can only be of two types 1) using peripheral coverage with resin in the residual ridge crest, and 2) with total coverage of mandibular space and denture.19,20
Some authors have implemented upper denture weight decrease and lower denture weight increase, calling them «gravitational prostheses».21,22
Lower GP is a combination of acrylic resin CP, lodging within it a metallic structure. This structure can be made of different alloys (gold, chrome-cobalt or chrome nickel).20-22 Nevertheless, implementation of these dentures has been empirically performed, this forcibly requires structured research of these prostheses. Thus, the aim of the present study was to compare stability, retention and MD in patients with two types of full prostheses: CP versus GP; studies were conducted at the Total Prosthodontics Clinic of the National School of Dentistry, National University of Mexico, UNAM.
Material and methods
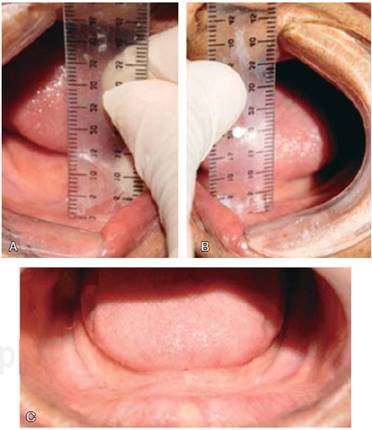
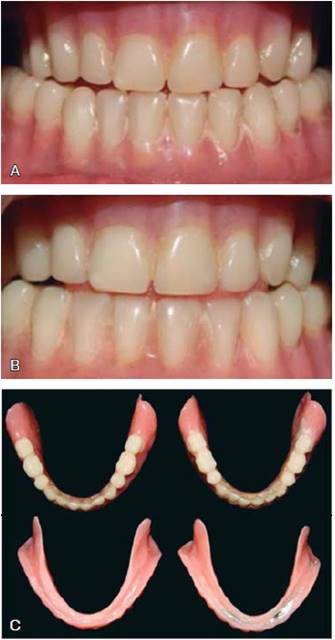
A crossed clinical examination was conducted (using the subject as his own control). A convenience sample was performed selecting patients attending the Total Prosthodontic Clinic, National School of Dentistry, National University of Mexico (UNAM). Patients were fully edentulous with classification of residual ridge V or VI according to Cawood and Howell (1988), with height not exceeding 2 mm, ages ranging 55-85 years, lacking mental disorders and systemically controlled (Figures 1 and 2). Patients were initially assessed according to House Boucher2 mental attitude classification. All selected patients were invited to participate in the research project; subjects who accepted did so under validly informed consent. Clinical procedure was conducted dividing subjects into two groups. Group 1 used CP initially, group 2 used GP from the beginning. A six month usage period was established for both groups; required adjustments were performed and written instructions were administered. After this period, lower dentures were replicated with closed mouth impressions, to then change groups (crossed design) (Figure 3).
Direct source.
Figure 2 Class V of residual ridge. A and B) 2 mm height of residual ridge, respectively right and left premolar are. C) Required clinical characteristics to be included in the study.
Direct source.
Figure 3 Identical conventional full lower denture, and gravitational denture. A) Conventional. B) Gravitational. C) Comparison of both types of prostheses.
Stability was measured according to method described by Woelfel: with the patient in physiological rest position, index and thumb were placed on the lower denture, exerting horizontal and rotary forces, thus determining the degree of movement (Table I and Figure 4).23
Table I Stability scale.23
| Woelfeld scale | |
| Excellent (4) | Prosthesis does not have movement, or there is slight movement when strong direct or rotating force is applied |
| Good (3) | Prosthesis does not have movement, or there is slight movement when applying strong rotating force, but it moves or is dislodged when a strong direct force is applied on one side or the front of the denture |
| Acceptable (2) | Prosthesis has considerable movement when rotating force is applied and is dislodged when moderate direct force is applied. |
| Poor (1) | A force direct or rotating force causes movement in the prosthesis and can dislodge it. Denture must be re-based or replace. |

Direct source.
Figure 4 A) Application of circular loads on the denture. B) Application of direct force on the right lateral section of the prosthesis. C) Application of direct force on the left lateral section of the prosthesis.
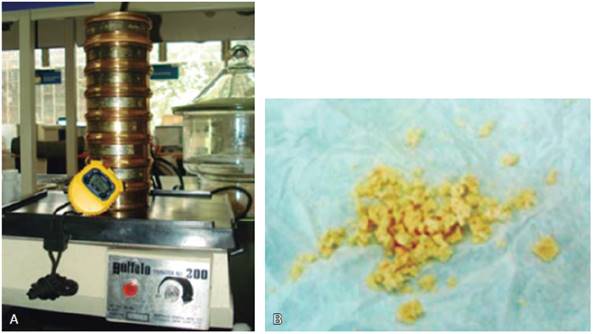
MD was achieved through determination of mean particle size of chewing tablets made with modified Optocal and subjected to volumetric screening.6,13-16,24 To achieve this, the patient was placed in a resting physiological position, sitting down on a bench placed opposite to the operator. The patient was instructed to chew on the artificial foodstuff in quantities indicated in the test,6,9 chewing normally for 40 masticatory cycles, and taking his time. Immediately afterwards, they spat all fragments within their mouth, into a filter paper, rinsing their mouth with water in order to recover remnants and rinsing their dentures. Moreover, the oral cavity was examined in order to ascertain that no remaining particles were left. This procedure was repeated for a total of six times. The first sample was discarded, since it was only used as a familiarization test. All samples were rinsed and dried in a chamber by means of silica pearls during 24 hours. After this they were placed in a tower of seven sieves (mesh opening of 5.6, 4.0, 2.8, 2.0, 0.85, 0.425 and 0.25 mm) on a dental vibrator for two minutes. Material in each sieve was weighed in the 0.01 g OHAUS® precision scale (Figure 5). MPS was calculated by means of the Rosin Rammler equation (Qw = 100 [1 - 2-(x/x50)b]).25
Direct source.
Figure 5 A) Equipment to calculate distribution of artificial foodstuff I different-sized meshes. B) Tablets chewed during 40 masticatory cycles.
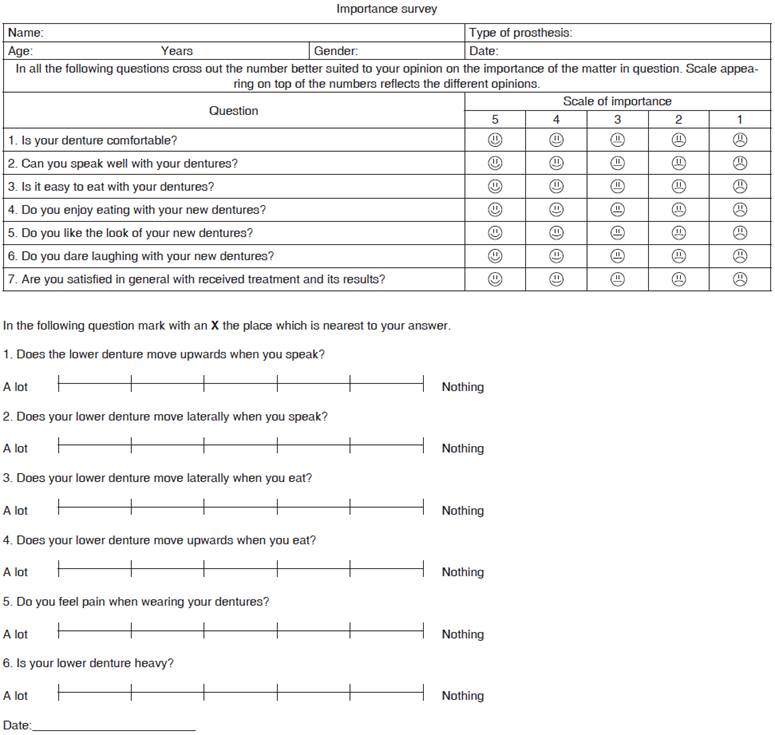
Patient’s perception was determined by means of a subjective instrument of 15 items, through Likert-type scales, and an analogous visual scale, assessing stability, retention, mastication and conformity with treatment (Figure 6). Moreover, all types of prostheses were weighed.
Statistical analysis
Descriptive analysis procedures were undertaken. Considering the number of cases to be evaluated, comparisons were analyzed with Wilcoxon sign rank test and Spearman correlation test. Established significance level was p ≤ 0.1. Analysis was conducted with support of statistical package SPSS, version 16.
Results
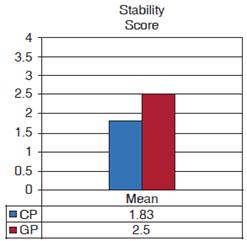
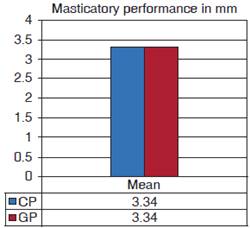
Initially, 30 subjects participated in the test, nevertheless, this number decreased to six, mainly due to health causes (falls, physically limiting diseases, demises, among others). Weight of prostheses increased up to 40% (z -2.201 p = 0.028) Stability test revealed that GP were more stable (p = 0.046); with respect to masticatory performance, no differences between prostheses were found in MP (z value -.125, p = 0.893).
With respect to the survey with Likert-type questions and analog visual scale (AVS) (Figure 6) total sum indicates contrast between both types of prostheses: gravitational prostheses were more functional (AVS p = 0.043). Statistical comparison tests mainly identified a difference (p = 0.039) in the question «lateral mobility of the denture when speaking» as well as «pain when using it», which would indicate more pain and difficulty to speak with conventional dentures (Figure 7 and 8).
As an example of generalized feeling we reproduce comments of a patient who, due to health reasons did not continue in the study, but he was very grateful: «Immediately after placement of gravitational denture (without knowing the clear purpose of the project) I felt greater weight. Increase of weight is to give it more stability, right? I feel improvement when eating, speaking, and my denture no longer moves. I feel happy!»
Discussion
Use of full acrylic resin prostheses is conventional, taking into account the advantages they offer when compared to metallic base prostheses.7 Nevertheless, use of acrylic/metal combines some benefits of both materials used in the present study. Results showed improvement in denture function, such as mentioned by Reis (2009), although not as accentuated as improvement observed with implant-supported dentures.13,21,26-29
Stability was clearly greater in gravitational prostheses. It is clear that the main treatment to «recover» ideal size of residual ridge for suitable retention and stability will always be surgical procedure, nevertheless, not all patients are candidates for such procedures, or do not possess the required financial means, thus, gravitational prostheses, even though with increased price due to metallic structure, can be a viable alternative to treatment.
Normally, dentists instruct patients wearing full prostheses in the sense that foodstuffs must be well hydrated to facilitate their breakdown. Artificial food Optocal, being plastic, hinders saliva entrance thus decreasing humectation, therefore, it could be modified to resemble more natural foodstuffs consumed by these patients, especially because detriment of this MP has been shown in total prostheses wearers, even more so in atrophic borders,14 thus compromising satisfaction of the prosthetic treatment. Nevertheless, material standardization facilitates procurement of more objective results. Certainly, several factors intervene in determination of adequate mastication, such as age, salivation, size of the residual ridge, decreased or increased vertical dimension, denture retention, placement of artificial teeth including width of occlusal surface of the teeth, up to quality and hardness of foodstuffs. In the present study difficulties were encountered with DM test, even though the test foodstuff possesses hardness of 40% lesser than the foodstuff used in patients with teeth. When comparing TMP masticatory performance patients in this research (3.34 mm) with that of average of young males and females with full dentition and lacking Optosil-measured malocclusion (1.8 mm), it could be observed that they exhibited MP lesser in 46%.30 The fact of not having found differences in TMP even though patients reported they could eat better with gravitation prostheses, is due to a smaller effect, therefore the size of the sample should be much greater. Other studies6 surprisingly report that TMP only decreased in 9% when comparing original and new prostheses, thus implying that benefits derived from foodstuff fracture capacity experience small increase. These data confirm the fact that masticatory function of toothless patients requiring full dentures is greatly impaired, causing great difficulties when chewing hard foodstuffs.31-34 It is well known that patients afflicted with mastication problems caused by partial or total edentulism exhibit nutritional deficiencies35-37 and systemic disorders such as dyspepsia,5 these patients’ increase intake of soft foods and carbohydrates, decreasing intake of fiber-rich foods,37,38 and proteins found in animal meat.34,35 These problems decrease quality of life and increase mortality. (Heath, 1972, Miura 2000, De Souza-e-Silva et al 2010, Greksa 1995 and Sherder 2008), thus it is of the utmost importance to improve masticatory function.
It is important to stress that lack of previous studies in order to be able to compare obtained results was a limiting factor for this clinical assay, other limitations were the following: health problems such as depression, trauma and demise, which reflected upon patient cooperation and attendance. There are no records of standardization in metallic structure manufacturing, only records of metallic bases are available, and some dental technicians provide reports on metallic bar shapes.20,21
Conclusions
According to results of statistical tests and correlations on patients’ perceptions, it is hereby concluded that there was greater function and satisfaction with gravitational prostheses. Patients were able to speak better and they smiled more often, felt stability when prostheses were heavy and, at the same time, they experienced better food processing abilities, this can lead us to believe that gravitational prostheses are a suitable treatment alternative for patients with extreme mandibular atrophy.
One of the advantages found in the present study was subjective measurement to complement tests conducted in the mouth,6 since, gauged standardized tests are quite different from freely undertaken daily mastication, and therefore it is important to evaluate patients’ satisfaction with respect to speech, eating etc.
Referencias
1. Ozawa-Deguchi JY, Ozawa-Meida JL. Fundamentos de prostodoncia total. México: Trillas; 2010. [ Links ]
2. Zarb GA, Bolender CL, Hickey JC, Carlsson GE. Prostodoncia total de Boucher. 10 ed. México: Interamericana McGraw-Hill; 1994. [ Links ]
3. Telles D. Prótesis total. Convencional y sobre implantes. Sao Paulo: Santos; 2011. [ Links ]
4. Sharry JJ. Prostodoncia dental completa. Barcelona: Toray; 1977. [ Links ]
5. Carretero-Ancelmo D. Deficiencia masticatoria por pérdida dentaria como factor de riesgo para dispepsia en el adulto mayor [Tesis Licenciatura]. Lima, Perú: Universidad Nacional Mayor de San Marcos. Facultad de Odontología. E. A. P. de Odontología; 2008. [ Links ]
6. Ahmad SF. An Insight into the masticatory review article performance of complete denture wearer. Annal Dent Univ Malaya. 2006; 13: 24-33. [ Links ]
7. Winkler S. Prostodoncia total. México: Editorial Limusa; 2004. [ Links ]
8. Mioche L, Bourdiol P, Monier S, Martin JF, Cormier D. Changes in jaw muscles activity with age: effects on food bolus properties. Physiol Behav. 2004; 82 (4): 621-627. [ Links ]
9. Teodisio-Procopio E. Desempeño masticatorio en niños mexicanos de 5-7 años con mordida profunda antes y después del tratamiento con el Nite-Guide [Tesis Magistral]. México: Universidad Nacional Autónoma de México. Facultad de Odontología. División de Estudios de Posgrado e Investigación; 2009. [ Links ]
10. Sánchez-Ayala A. Metodología clínica del rendimiento masticatorio. Fórmula Odontológica. 2004 [Internet]; 2 (3). Disponible en: http://www.odontologosecuador.com/espanol/artodontologos/rendimiento_masticatorio_dental.htm [ Links ]
11. Farias Neto A, Mestriner Junior W, Carreiro Ada F. Masticatory efficiency in denture wearers with bilateral balanced occlusion and canine guidance. Braz Dent J. 2010; 21 (2): 165-169. [ Links ]
12. Slagter AP, Olthoff LW, Steen WH, Bosman F. Comminution of food by complete-denture wearers. J Dent Res. 1992; 71 (2): 380-386. [ Links ]
13. Fontijn-Tekamp FA, Slagter AP, Van Der Bilt A, Van ‘T Hof MA, Witter DJ, Kalk W, Jansen JA. Biting and chewing in overdentures, full dentures, and natural dentitions. J Dent Res. 2000; 79 (7): 1519-1524. [ Links ]
14. Liz-Pocztaruk R, Araujo-Vidal R, da-Fontoura-Frasca LC, Gomes-Rivaldo E, Duarte-Gaviao MB, Van-der-Bilt A. Satisfaction level and masticatory performance of patient rehabilitated with implant-supported overdentures. Rev Odonto Cienc. 2009; 24 (2): 109-115. [ Links ]
15. Liz-Pocztaruk R, Fontoura-Frasca LC, Gomes-Rivaldo E, Lima-Fernandes E, Duarte-Gaviao MB. Protocol for production of a chewable material for masticatory function test (Optocal-Brazilian version). Braz Oral Res. 2008; 22 (4): 305-310. [ Links ]
16. Speksnijder CM, Abbink JH, van der Glas HW, Janssen NG, Van Der Bilt A. Mixing ability test compared with a comminution test in persons with normal and compromised masticatory performance. Eur J Oral Sci. 2009; 117 (5): 580-586. [ Links ]
17. Ozawa-Deguchi JY. Prostodoncia total. 5 ed. México: Universidad Nacional Autónoma de México; 1995. [ Links ]
18. Koshino H, Hirai T, Ishijima T, Tsukagoshi H, Ishigami T, Tanaka Y. Quality of life and masticatory function in denture wearers. J Oral Rehabil. 2006; 33 (5): 323-329. [ Links ]
19. Horst UA. Prótesis para desdentados. Berlín, Alemania: Quintessence; 1973. [ Links ]
20. Brudvik JS. Capítulo 17: Bases metálicas. En: Morrow RM, Rudd KD, Rhoads JE. Procedimientos en el laboratorio dental prótesis completas. Tomo I. Barcelona: Salvat; 1988. pp. 455-472. [ Links ]
21. Reis JC. Placas gravitacionales. Alta Técnica Dental. 2009; 56: 10-14. [ Links ]
22. Torres N. Placas huecas. Alta Técnica Dental. 2008; 50: 41-47. [ Links ]
23. Rubilar F, Jiménez LF, Rochefort C. Retención y estabilidad de bases protésicas superiores obtenidas a partir de dos técnicas de impresión utilizadas en la rehabilitación de dentaduras totales con prótesis convencional. Revista Dental de Chile. 2009; 100 (1): 4-12. [ Links ]
24. Van Der Bilt A, Mojet J, Tekamp FA, Abbink JH. Comparing masticatory performance and mixing ability. J Oral Rehabil. 2010; 37 (2): 79-84. [ Links ]
25. Rosin P, Rammler E. Gesetzmassigkeiten in der kornzusammensetzung des zementes. Zement. 1933; 31: 427-433. [ Links ]
26. Ortiz M, Scarton J, Rodríguez A, Canto O, Cabratosa J. Sobredentaduras: una opción de tratamiento fiable. A propósito de un caso clínico. DENTUM. 2009; 9 (2): 63-68. [ Links ]
27. Cho SC, Froum S, Tai CH, Cho YS, Elian N, Tarnow DP. Immediate loading of narrow-diameter implants with overdentures in severely atrophic mandibles. Pract Proced Aesthet Dent. 2007; 19 (3): 167-174. [ Links ]
28. Lang JP, Lagustera C, Mendonça MJ, Takahachi C. Avaliação dos sistemas de retenção para overdentures implanto suportadas mandibulares: revisão de literatura. RGO. 2006; 54 (4): 356-362. [ Links ]
29. Mestre-Aspa R, Sánchez-Garcés MA, Berini-Aytés L, Gay-Escoda C. Estudio del grado de satisfacción en pacientes edéntulos totales tratados con implantes. Avances en Periodoncia. 2001; 13 (2): 93-99. [ Links ]
30. Hernández-Sánchez F. Desempeño masticatorio en adultos jóvenes con oclusión normal [Tesis Magistral]. México, D.F.; 2012. [ Links ]
31. Ishikawa Y, Watanabe I, Hayakawa I, Minakuchi S, Uchida T. Evaluations of masticatory performance of complete denture wearers using color-changeable chewing gum and other evaluating methods. J Med Dent Sci. 2007; 54 (1): 65-70. [ Links ]
32. Sheiham A. Dietary effects on dental diseases. Public Health Nutr. 2001; 4 (2B): 569-591. [ Links ]
33. Hung HC, Colditz G, Joshipura KJ. The association between tooth loss and the self-reported intake of selected CVD-related nutrients and foods among US women. Community Dent Oral Epidemiol. 2005; 33 (3): 167-173. [ Links ]
34. Quandt SA, Chen H, Bell RA, Savoca MR, Anderson AM, Leng X et al. Food avoidance and food modification practices of older rural adults: association with oral health status and implications for service provision. Gerontologist. 2010; 50 (1): 100-111. [ Links ]
35. Akpata E, Otoh E, Enwonwu C, Adeleke O, Joshipura K. Tooth loss, chewing habits, and food choices among older Nigerians in Plateau State: a preliminary study. Community Dent Oral Epidemiol. 2011; 39 (5): 409-415. [ Links ]
36. Geissler CA, Bates JF. The nutritional effects of tooth loss. Am J Clin Nutr. 1984; 39 (3): 478-489. [ Links ]
37. Borges-Yáñez SA, Maupomé-Carvantes G, Martínez-González M, Cervantes-Turrubiates L, Gutiérrez-Robledo LM. Relación entre el estado de salud bucal y el consumo de alimentos energéticos y nutrimentos en ancianos de tres localidades en México. Nut Clin. 2003: 6 (1): 9-16. [ Links ]
38. Samnieng P, Ueno M, Zaitsu T, Shinada K, Wright FA, Kawaguchi Y. The relationship between seven health practices and oral health status in community-dwelling elderly Thai. Gerodontology. 2013; 30 (4): 254-261. [ Links ]
Received: November 2016; Accepted: November 2017











 texto em
texto em