Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista odontológica mexicana
Print version ISSN 1870-199X
Rev. Odont. Mex vol.18 n.4 Ciudad de México Oct./Dec. 2014
Case reports
From immediate prostheses to overdentures: Case report
Haidé Reséndiz Melgar* y Rubén Bernal Arciniega§
* Oral Prosthesis and Implantology Master, Graduate and Research School.
§ Master in Dentistry, Professor, Oral Prosthesis and Implantology Specialty.
National School of Dentistry, National University of Mexico.
ABSTRACT
The present article purports a description of laboratory and clinical procedures used to rehabilitate a partially maxillary and mandibular edentulous patient. Treatment was divided into two phases. The first phase encompassed the insertion of an immediate maxillary total prosthesis as well as an immediate mandibular overdenture with balanced occlusal scheme. Once the patient's tissues were stabilized, the second phase of the treatment was undertaken: immediate prostheses were exchanged for a conventional maxillary denture as well as an tooth-supported overdenture retained by root-axial stud-type devices. In this second phase, the immediate prostheses' anterior guide was reproduced and a lingualized occlusal scheme was used. Described procedures allowed the decrease of clinical and laboratory time without endangering the quality of the final rehabilitation.
Key words: Immediate denture, overdenture, full denture, lingualized occlusion.
BACKGROUND
Rehabilitation of a patient who will eventually wear dentures represents a challenge for any prosthodontist, this is due to the fact that oftentimes, different treatment modes should be combined.
Whenever a patient is to be subjected to multiple extractions, it is recommended that at the same appointment when extractions are to be performed, immediate prostheses be inserted to help protect and exert pressure on soft tissues and thus avoid collapse, decrease residual crest resorption, improve residual shape of bone crests,1-3 decrease bleeding and pain in post-extraction sites, maintain cheek and lip support and improve and re-establish facial harmony as well as facilitate phonation and mastication during the transition period from natural teeth to artificial teeth.4
In addition to all the aforementioned, immediate prosthesis placement psychologically benefits patients since the embarrassing period of not having natural or artificial teeth is avoided.5
When using an immediate overdenture, that is, a removable denture supported by residual ridges and natural teeth or implants,6 additional benefits are maintenance of joint proprioception with neuromuscular reflex78 as well as preservation of bone volume in the residual ridges.9
It must nevertheless be mentioned that the aforementioned benefits are sometimes limited by loss of abutment teeth10 or by the impossibility of placing artificial teeth without incurring in over-contouring the prosthesis.11
In spite of benefits achieved with these treatments, the following disadvantages are inherent to their performance: patient discomfort when subjected to multiple extractions, inability to achieve esthetic potential, difficulty to properly record cranio-mandibular relationships, problems while adapting the denture on extraction day, increment of treatment cost, denture over-contouring and premature need for tissue conditioning or re-base materials.5
Treatment of overdentures and immediate prostheses followed by conventional procedures are part of the wide range of prosthetic options available to rehabilitate an edentulous patient. Irrespective of the selected option, it is essential to consider the fact that any alternative must purport the aim of establishing functional occlusion.12
For the last 70 years, the occlusal scheme of a full denture can be classified into one of the following four occlusal concepts: balanced occlusion, unbalanced occlusion, monoplane or linear articulation and lingualized occlusion.13,14 Selection of occlusal scheme for a full denture remains subject of controversy. Up to this date, selection and placement of posterior teeth in a denture still is an empirical fact,14-18 since there still is deficient evidence of clinical studies to compare the different options. Notwithstanding the aforementioned facts, the lingualized occlusion scheme is currently assuming a more prominent role.18-20
Lingualized occlusion provides the following benefits: improved adaptation to different types of ridges, improved masticatory effectiveness,21 lateral interferences elimination, artificial teeth can be placed without risk of unbalancing the articulation due to cusp interferences,22 greater ease for cleansing mandibular occlusal surfaces, better esthetics, ease of manufacture and adjustment.19,20,23
Proper selection and development of occlusal scheme to be used in a rehabilitation is essential; it contributes to achieving predictable results in the full denture treatment development.24
Predictability of a prosthetic rehabilitation in a partially edentulous patient who will end up wearing dentures is difficult to achieve since two treatment phases are involved: immediate dentures and final restoration. Even though these clinical circumstances are common in the world's population,25 in the conducted literature review, no references were found which described evolution of a case from the point of immediate denture insertion up to the completion of the rehabilitation. It was thus considered necessary to count with appropriate documents which would document this approach.
The aim of the present article was to describe laboratory and clinical procedures used to rehabilitate a partially edentulous patient, from the moment of insertion of an immediate full prosthesis until final prosthetic rehabilitation of a conventional maxillary full denture and an overdenture supported by teeth and alveolar ridges and retained with axial-root attachments, manufactured under the approach of lingualized occlusion.
CASE PRESENTATION
A 62 year old male attended the Implantology and Oral Prosthesis Service of the Graduate and Research School, National School of Dentistry, National University of Mexico (UNAM), in order to <<fix his mouth>>. Upon interrogation, the patient disclosed the fact of being a controlled diabetic, with a 10 years evolution of the disease, as well as not having previously worn dentures.
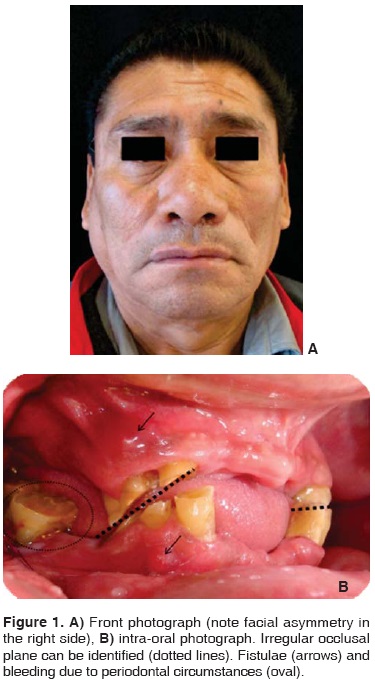
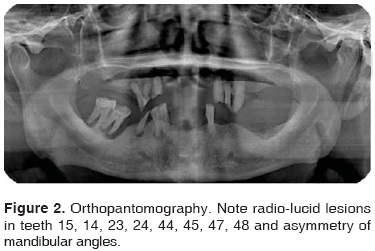
Extra-oral clinical examination revealed facial symmetry and right mandibular condyle dislocation with decrease of maximum opening. Intra-oral examination revealed upper and lower partial edentulism, presence of fistulae in the region of teeth 14, 24, 44, irregular occlusal plane, chronic periodontitis as well as poor oral hygiene (Figure 1). X-ray assessment revealed radio-lucid lesions in teeth 15, 14, 23, 24, 44, 45, 47, 48 as well as asymmetrical mandibular rami (Figure 2).
In accordance to observed clinical circumstances in the patient, several treatment options were proposed. The patient accepted a two-phase procedure. Phase I: periodontal treatment followed by extractions of teeth 15, 14, 13, 25, 24, 23, 45, 47, 48; insertion of an immediate full maxillary denture and an immediate mandibular overdenture, using as abutments teeth 33, 43, 44. Phase II consisted of insertion of a full upper denture and a mandibular overdenture supported by teeth and alveolar ridges and retained by axial root attachment in teeth 33, 43 and single coping in tooth 44.
Taking an impression was the treatment starting point for the manufacturing of immediate dentures. Pressure-free technique was used26 with trays (Rimlock, Dentsply, USA) which were individualized using wax (Utility-wax, mdc Dental, Mexico) as well as irreversible hydrocolloid (Max Print Chromatic, mdc Dental, Mexico).
Impressions were poured with type III plaster (Magnum, mdc Dental, Mexico). Recording plates were manufactured on these models using visible-light activated acrylic (Palatray, Kulzer, Germany and True Wax, Dentsply, USA). Cranio-mandibular relationships were recorded (Imprint Bite 3M ESPE, Germany) and models were transported to a semi-adjustable articulator with the help of a facial bow (Hanau 194 modular system and Hanau Springbow, Water Pick, USA).
Location of upper and lower incisors was clinically assessed (MFT Vita Zahnfabrick, Germany) in accordance with phonetic and esthetic parameters (Figure 3).27,28 Model surgery was later undertaken, a gauge 89 acetate was vaccumed (Ultradent, USA) and was then used as surgical guide on extraction day.

Posterior teeth (MFT Vita Zahnfabrick, Germany) were placed following a balanced occlusal scheme. Occlusion plane was achieved taking the upper third of pyriform papillae as a reference point. A biomechanical plate (Universal Co, USA) for occlusal analysis was used to shape medio-lateral and anterior-posterior curves. It was placed on the mandibular model with the help of silicon guides (Elite HD putty, Zhermack, Italy). Posterior teeth were placed within the vestibular-lingual limits of Pound's triangle.28,29
Dentures were acrylized with visible-light activated acrylic (Triad Dentsply, USA), and polished and finished in the conventional manner (Polycril mdc Dental Mexico; Universal Polishing Paste, Ivoclar, Liechtenstein).
Immediate dentures were inserted on extraction day. Pulpectomy and coping preparation of teeth 33, 43 and 44 (Figure 4) were equally achieved at that time. 24 hours later, the patient was programmed to adjust occlusion. One week after insertion of immediate dentures, root canal treatment of abutment teeth was completed, and tissue conditioner was applied (Lynal, Dentsply, USA). This material was periodically changed according to circumstances exhibited by the patient's tissues.

Six months after the surgical phase, the intaglio surface of the dentures was replicated with heavy-body silicon (Speedex putty, Coltene, Whaledent, Swizerland).
Individual impression trays without spacers were manufactured on the duplicates, a wax rim was placed instead of conventional handles (Nictone mdc Dental, and All-Season Filene wax, Mexico). This process was undertaken in order to enable physiological impressions to later be used as recording bases (Figure 5).
Maxillary muscle rectification was taken with heavy-body silicon, final impression was taken with light-body silicon (Orange wash and Zetaflow putty, Zhermack, Italy).
Muscle rectification of mandibular physiological impression was achieved with heavy silicon, final impression was taken with light-body silicon (Speedex putty and Speedex light body, Coltene, Whaledent, Switzerland). Light impression material was introduced within root canals using a number 40 lentulus (Dentsply, USA). Castable plastic pins were placed in order to confer support to this portion of the impression material (Reliance dental Mfg, USA). Physiological impressions were poured with type IV plaster (Fuji, USA).
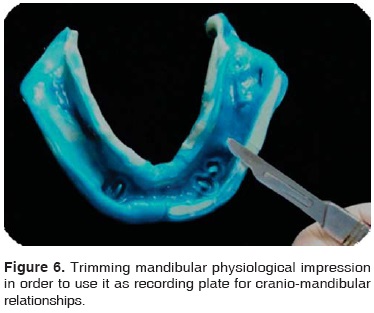
Upon model completion, they were used as recording plates for physiological impressions, 2 mm of the muscle rim were trimmed before placing them into the patient's mouth (Figure 6). Cranio-mandibular recordings were taken with polyvinyl siloxane (Imprint bite, 3M ESPE, Germany).
Study models were transferred to a semi-adjustable articulator with the help of a facial bow (Hanau 194, modular system and Hanau Springbow, Water Pick, USA); they were mounted with the split-cast system (Bredent, Germany) in order to be transferred to the parallelometer and easily remounted.
Base plates were manufactured with visible-light activated acrylic (Palatray, Kulzer, Germany). With the help of the Alma Gauge system (Dentsply, USA) the position of anterior teeth present in immediate dentures was transported (Physiodens Vita Zahnfabrik, Germany).
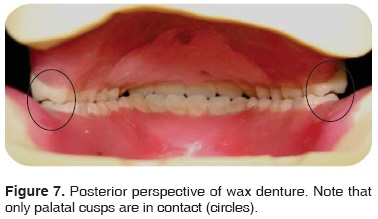
Occlusal curve and plane were obtained in the aforementioned manner. Posterior teeth (Lingoform Vita Zahnfabrik, Germany) were placed following mechanical principles described by Payne22 to develop a lingualized occlusal scheme (Figure 7).
Wax-up dentures were tested and a matrix was obtained with heavy-body siloxane polyvinyl (Elite HD putty, Zhermack, Italy) in order to record the position of teeth. This silicon matrix was used as a guide to determine space available for axial attachments (Vario-Kugel-Snap UNI Bredent, Germany) and to place a metallic mini-base.
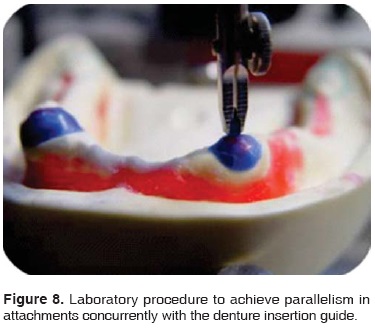
Attachments for teeth 33 and 43 were parallelized (Paratherm, Dentaurum, Germany) and cast as well as the single coping for tooth 44 in an alloy with high gold content (60%) (Jelenko, USA) (Figure 8). Simultaneously to this procedure a metallic mini-base was manufactured on the mandibular working model; it was cast in a chrome-cobalt based alloy (Remanium 800, Dentaurum, Germany). Mini-base was painted with an opacifying agent (Eclipse mdc Dental, Mexico) and it was reserved to be captured into the mandibular denture during processing.
The metallic mini-base was fixed upon the mandibular working model with cyanoacrylate (Crazy Kola Loca, Mexico) so as to avoid displacements during processing. In order to preserve festoon, prostheses were placed in a muffle using laboratory-use silicon (Zetalabor, Zhermack, Italy) and were processed with pigment-characterized (Aesthetic colour set, Candulor, Germany), thermo-curing acrylic (Lucitone, Dentsply, USA).
Dentures were re-mounted and occusal adjustment was achieved using an articulating foil (Braush foil, Bausch, USA). Twelve contacts per arch were obtained. Contacts were located at upper palatal cusps and on the central ridge line of mandibular teeth. Dentures were polished (Polycril, mdc Dental, Mexico) and shined with paste to polish resin (Universal Polishing Paste, Ivoclar, Germany).
In one single appointment root attachments and single coping were cemented (Ketac cem 3M ESPE, Germany) and dentures were inserted. 48 hours after insertion attachments were activated on the mandibular overdenture using visible-light activated acrylic (Triad gel, Dentsply, USA) (Figure 9). Finally, occusal contacts were once more verified, completing thus the second phase of treatment (Figure 10).


DISCUSSION
Rehabilitation of a partially edentulous patient who will in the future wear full dentures encompasses processes which progress from immediate denture insertion up to placement of permanent dentures. Nevertheless, consulted bibliography did not reveal references describing the clinical evolution of such patients; this shows the existing need to count with information describing cases with these characteristics, from beginning to end. It would thus be possible to identify clinical decisions which contributed to the final result of a given rehabilitation as well as relate different stages of treatment among themselves. This would be beneficial to patients and clinicians alike.
The particular circumstances of the present case helped obtain predictable results in immediate dentures. It could be established that mounting models in the articulator represented the clinical circumstances of the patient.
The test of placing the incisor teeth ensured suitability of anterior guide. According to Pound, this is a critical factor for the esthetic success of a denture.28-30 Nevertheless, when immediate dentures are manufactured, clinical tests are sometimes not feasible; therefore, it is vital to inform the patient of the possible disadvantages of this type of treatment.5
Immediate dentures helped improve esthetics and masticatory function of the patient. Likewise, they provided valuable information for the final rehabilitation. Based on them, accurate individual impression trays could be manufactured (by means of replicating its intaglio surface). Information was acquired to reproduce the anterior guide which phonetically and esthetically resulted appropriate for the patient. This allowed saving clinical times (anatomical impression, upper rim orientation, anterior teeth tests) which are necessary for described conventional procedures.11,26
Another advantage achieved with the placement of immediate dentures was condylar repositioning in order to obtain better function of the temporomandibular joints. This facilitated obtaining cranio-mandibular relationships for permanent dentures.
Attachments and metallic mini-base for the mandibular overdenture provided favorable biological31 and mechanical behavior for the rehabilitation.32 Nevertheless, the cost represented a considerable investment for the patient.
In this particular case, lingualized occlusion was considered the most viable occlusal scheme, since mandibular deviation caused by the patient's facial asymmetry required freedom of eccentric movements.33 According to several authors14,16,18,19,22 this mechanical behavior is one of the most important advantages of lingualized occlusion. Nevertheless, it is relevant to remember that, to the present date, there is no scientific evidence to indicate that this occlusal scheme is better to any other.16,17
CONCLUSIONS
It is necessary to count with documents which fully describe the clinical evolution of a partially edentulous patient, future candidate to wearing dentures.
Treatment proposal here presented described clinical and laboratory procedures used to rehabilitate a partially edentulous patient, progressing from the moment of immediate denture insertion up to the permanent prosthetic rehabilitation, which was a conventional maxillary denture and an overdenture supported by teeth and alveolar ridge and retained by axial root stud attachments. Described procedures allowed decrease of clinical and laboratory times without incurring in poorer quality of final rehabilitation.
REFERENCES
1. Johnson K. A clinical evaluation of immediate denture procedures. J Prosthet Dent. 1966; 16: 799-810. [ Links ]
2. Loo W. Ridge preservation with immediate dentures. J Prosthet Dent. 1968; 19: 5-11. [ Links ]
3. Kelly EK, Sievers RF. The influence of immediate dentures on tissue healing and alveolar ridge form. J Prosthet Dent. 1959; 9: 738-742. [ Links ]
4. Seals RR, Kuebker WA, Stewart KI. Immediate complete dentures. Dent Clin North Am. 1996; 40: 151-167. [ Links ]
5. Gilboa I, Cardash HS. An alternative approach to immediate overdenture. J Prosthodontics. 2009; 18: 71-75. [ Links ]
6. The Academy of Prosthodontics. The glossary of prosthodontic terms. J Prosthet Dent. 2005; 4 (1): 58. [ Links ]
7. Pacer FJ, Bowman DC. Occlusal force discrimination by denture patients. J Prosthet Dent. 1975; 33: 602-609. [ Links ]
8. Mushimoto E. The role in masseter muscle activities of functionally elicited periodontal afferents from abutment teeth under overdentures. J Oral Rehabil. 1982; 8: 441-455. [ Links ]
9. Van Waas MA, Jonkman RE, Kalk W, Van't Hof MA, Plooij J, Van Os JH. Differences two years after tooth extraction in mandibular bone reduction in patients treated with immediate overdentures or with immediate complete dentures. J Dent Res. 1993; 72 (6): 1001-1004. [ Links ]
10. Ettinger RL, Qian F. Abutment tooth loss in patients with over-dentures. J Am Dent Assoc. 2004; 135: 739-746. [ Links ]
11. Zarb GA, Bolender LC, Carlsson GE. Boucher's prosthodontic treatment for edentulous patients. 4th ed. USA: Ed. Mosby; 1990. [ Links ]
12. Fotoula N, Pagona KA. Rationale for choices of occlusal schemes for complete dentures supported by implants. J Oral Implantol. 2006; 32 (4): 200-203. [ Links ]
13. Beck H. Occlusion as related to complete removable prosthodontics. J Prosthet Dent. 1972; 27 (3): 446-456. [ Links ]
14. Lang BR. Complete denture occlusion. Dent Clin N Am. 2004; 48: 641-665. [ Links ]
15. Peroz I. Comparison between balanced occlusion and canine guidance in complete denture wearers a clinical, randomized trial. Quintessence Int. 2003; 34 (8): 607-612. [ Links ]
16. Sutton AF, McCord JF. Interventions for replacing missing teeth: denture chewing surface designs in edentulous people. Evid Based Dent. 2005; 6 (2): 39-40. [ Links ]
17. Carlsson GE. Critical review of some dogmas in prosthodontics. J Prosthodontics Res. 2009; 53 (1): 3-10. [ Links ]
18. Bernal RA, Reséndiz HM. Oclusión lingualizada. Alta Técnica Dental la Revista. 2010; 62: 14-16. [ Links ]
19. Rodney D, Engelmeier RL. Lingualized occlusion revisited. J Prosthet Dent. 2010; 104 (5): 342-346. [ Links ]
20. Parr GR, Ivanhoe JR. Lingualized occlusion: an occlusion for all reasons. Dent Clin North Am. 1996; 40: 103-112. [ Links ]
21. Sutton A, Worthington H, McCord J. RTC Comparing posterior occlusal forms for complete dentures. J Dent Res. 2007; 86 (7): 651-655. [ Links ]
22. Payne H. A posterior set-up to meet individual requirements. Dent Dig. 1941; 47: 20-22. [ Links ]
23. Lang B, Razzoog. A practical approach to restoring occlusion for edentulous patients. Part II: Arranging the functional and rational mold combination. J Prosthet Dent. 1983; 50 (5): 599-606. [ Links ]
24. Sato Y, Tsuga K, Akagawa Y. A method for quantifying complete denture quality. J Prosthet Dent. 1998; 80 (1): 52-57. [ Links ]
25. Petersen P, Yamamoto T. Improving the oral health of older people: of the Who Global Health Programme. Community Dent Oral Epidemiol. 2005; 33: 81-92. [ Links ]
26. Ozawa DJ. Prostodoncia total. 5a ed. México: Ed. Dirección General de Publicaciones, UNAM; 1995. Pp. 210-221, 405-432. [ Links ]
27. Pound E, Murrell GA. An introduction to denture simplification. J Prosthet Dent. 1971; 26 (6): 570-580. [ Links ]
28. Pound E. Utilizing speech to simplify a personalized denture service. J Prosthet Dent. 1970; 24 (6): 586-600. [ Links ]
29. Pound E, Murrell GA. An introduction to denture simplification. Phase II*. J Prosthet Dent. 1973; 29 (6): 598-607. [ Links ]
30. Pound E. Lost-fine arts in the fallacy of the ridges. J Prosthet Dent. 1954; 4 (1): 6-16. [ Links ]
31. Wataha J. Biocompatibility of dental casting alloys: a review. J Prosthet Dent. 2000; 83 (2): 223-234. [ Links ]
32. Schneider R. Diagnosing functional complete denture fractures. J Prosthet Dent. 1985; 54 (6): 809-813. [ Links ]
33. Ozelik TB, Pektas ZO. Management of chronic unilateral tempo-romandibular joint dislocation with mandibular guidance prosthesis: a clinical report. J Prosthet Dent. 2008; 99 (2): 95-100. [ Links ]
Note This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam Mailing address:
Mailing address:
Haidé Reséndiz Melgar
E-mail: h_rm@hotmail.com











 text in
text in 


