Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Revista odontológica mexicana
versão impressa ISSN 1870-199X
Rev. Odont. Mex vol.18 no.3 Ciudad de México Jul./Set. 2014
Case report
Implant-supported prosthetic rehabilitation prior to conducting hyperbaric oxygen therapy and after having completed resection of an epidermoid carcinoma from the floor of the mouth and radiotherapy. Clinical case report
Mathias Martínez,* Rafael Ruiz Rodríguez,§ Juan Carlos López NoriegaII
* Maxillofacial Surgeon, Instructor- Professor of Surgery, Carabobo University, Valencia, Venezuela.
§ Graduate School Professor, National School of Dentistry, National University of Mexico (UNAM).
II Graduate School Professor, National School of Dentistry, National University of Mexico (UNAM).
ABSTRACT
The present article purports to present a case of implant-supported rehabilitation of a patient who had previously undergone a procedure of floor of the mouth squamous cell carcinoma resection followed by radiotherapy (56 Gy total). Treatment consisted on hyperbaric oxygen therapy by means of the following protocol: previous to implant placement: 20 daily sessions, 100% oxygen at 2.4 ATM pressure during 90 minutes as well as 10 daily sessions of 100% oxygen at 2.4 ATM pressure, during 90 minutes after implant placement. Prosthetic rehabilitation was conducted six months after implant placement. It consisted of an implant-supported removable prosthesis with a ring system to achieve retention. Presently the patient is at a two year follow-up period after rehabilitation, and is free of tumor activity in the treated zone. The patient has so far achieved appropriate esthetic and functional results.
Key words: Dental implants, hyperbaric oxygen, oral cancer.
INTRODUCTION
Patients who have been subjected to surgical and radiation therapy for treatment of head and neck cancer are considered a great challenge from the reconstructive perspective since esthetics and function of involved tissues must be restored.1 Sequels and complications elicited by combinations of the aforementioned treatments result in dental arches which are difficult or impossible to rehabilitate with conventional dentures, which is due to a denture deficient stability in a compromised oral environment.
Use of bone-supported implants can improve the quality of the rehabilitation allowing the patient to experience appropriate function and esthetics.2
Radiotherapy elicits tissue changes: they become hypo-cellular, hypo-vascular and hypoxic. This situation causes inappropriate and delayed healing with high probabilities of developing osteoradionecrosis. In the head and neck region, the lower jaw is the most commonly affected site.3 The fact that implant integration in previously irradiated tissues is compromised has been widely demonstrated. This could be due to the fact that those tissues experience hypo-vascularity as well as alterations in the ability of bone regeneration.4
Radiotherapy had previously been considered a contraindication in cases of implant surgery7 Nevertheless, it has been shown that hyperbaric oxygen therapy is the only vehicle to increase vascularity and oxygen tension in irradiated tissues.4
The present article presents treatment sequence and considerations to be observed in the rehabilitation of a patient with implant-supported prostheses who had previously been subjected to tumor resection and radiotherapy.
CLINICAL REPORT
A 56 year old male patient was referred to the Maxillofacial and Oral Surgery Service of the National School of Dentistry, National University of Mexico (UNAM). Referral was made from the Maxillofacial Prosthesis Service of the Instituto Nacional de Cancerología (National Cancer Institute) of Mexico (INCAN).
The patient had previously been assessed at the INCAN Head and Neck Service, which he attended due to a exophytic lesion located at the anterior and left region of the floor of the mouth. The lesion presented a five-month evolution period, was hard in consistency, painful to palpation and measured approximately 20 mm. Moreover, two jugulodigastric adenomegalies on the left side were detected. The lesions measured 2 and 1.5 cm respectively, were of a hard consistency and painless. Using the current classification system for tumor stages studies, it could be proposed that the patient was at Stage III (T2M1N0).5
The INCAN Head and Neck Service professionals undertook surgical treatment of the patient: They performed resection of the mucosa of the floor of the mouth, marginal mandibulectomy and bilateral neck supraomohyoid dissection. The lesion's histopathological assessment confirmed a diagnosis of moderately differentiated epidermoid carcinoma which infiltrated muscle tissue as well as the sublingual gland.
Two months after surgical treatment, the INCAN radiotherapy Service subjected the patient to teletherapy (external beam radiation) on the floor of the mouth and jugular-digastric and ganglionary areas. The treatment was divided into three fields: anterior, right lateral and left lateral, to achieve a total dosage of 56 Gy
The patient was then assessed by the INCAN Maxillofacial Prosthesis Service. At that point, suggested treatment was patient rehabilitation through titanium endosseous implants and removable full prosthesis supported by implants.
When the patient was assessed at our Service, he informed of a five year follow-up, free of tumor activity, nevertheless with limitations in phonation and masticatory functions. Intra-oral physical examination of the patient revealed conventional full denture rehabilitation in the upper jaw, edentulous state in the lower jaw, mucosa showing xerostomy and alveolar ridge pertaining to Cadwood and Howell Class IV (Figure 1).6

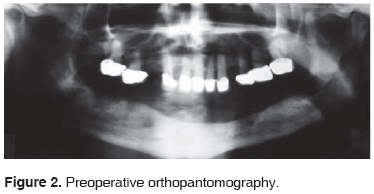
It was decided to undertake hyperbaric oxygen protocol. Protocol consisted of 20 daily sessions of 90 minutes at 2.4 ATM pressure, 100% oxygen (mono-seat hyperbaric chamber, Sechrist Industries Inc, 2820 Greta LN, Anaheim, CA) before implant placement. Ortho-pantomographic X-ray image revealed an appearance of residual alveolar ridge of normal characteristics (Figure 2).
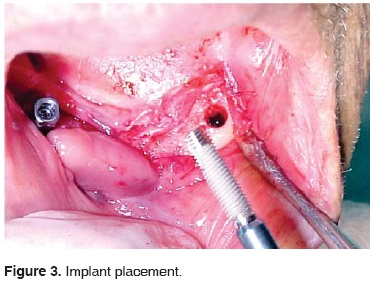
The patient was placed under local anesthesia with 2% lidocaine and 1:100.000 epinephrine. A 4 cm long incision was made at the anterior-inferior alveolar ridge crest (lower incisors area). A mucoperiosteal flap was raised which exposed residual alveolar bone in the lower anterior region of the mandible. The first surgical bed was achieved; a parallelism pin was placed before proceeding to second surgical bed, and so forth until achieving four receptor beds. Four 4 mm diameter x 16 mm long titanium screw implants were placed (Sulzer Dental Inc Taper Lock Screw TLB16) (Figure 3). First suture was undertaken with continuous sutures (Figure 4) and postoperative indications were issued. Oral administration of ibuprofen 400 mg, and amoxicillin, 500 mg, every 8 hours, during four days was prescribed. The following day, treatment was continued with 10 daily sessions of hyperbaric oxygen, 100% oxygen at 2.4 ATM pressure. Sessions lasted 90 minutes. Total was 30 sessions (20 sessions before surgery and 10 sessions after surgery). The patient did not experience any postoperative complication.

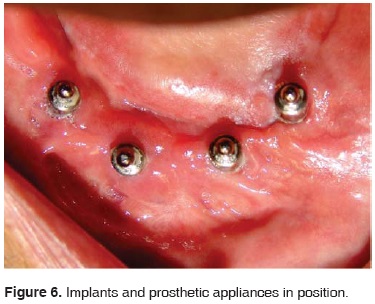
Six months later, an ortho-pantomography was conducted; it revealed data of implant integration. Implants were then uncovered, healing screws were placed, and clinical observation of their integration was undertaken.
Two weeks later the INCAN maxillofacial prosthesis service undertook the rehabilitation process.
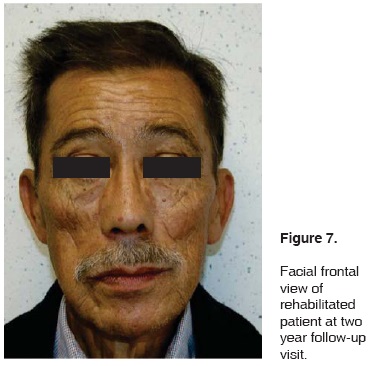
At a two-year follow-up period, the patient was satisfied with the results. The patient did not experience signs of inflammation around the implants and he exhibited suitable esthetic and functional properties (Figures 5, 6, 7 and 8).


DISCUSSION
Currently, the most commonly used treatment to treat malignant tumors of the cranial-maxillary-facial region is a combination of surgery and radiotherapy.7 Patients who have become edentulous as a result of malignant tumor resection procedures, frequently present esthetic, masticatory and phonation function alterations.9
Radiotherapy collateral effects can be divided into early and late effects. In the realm of early effects, an alteration is elicited in intrinsic structures of soft tissues: salivary glands, skin, oral and nasal mucosa (dermatitis, mucositis, xerosthomy, friable, functionally inadequate, atrophic mucosa). As part of late effects, bone tissue becomes involved and can suffer demineralization, reparative fibrosis, increase in infection susceptibility and finally, avascular necrosis (osteoradionecrosis).8
Radiotherapy elicits significant changes in bone tissue. These changes reduce the potential for implant bone integration and increase rate of implant non-integration.8
Experimental studies have histologically revealed that use of hyperbaric oxygen as adjuvant treatment reduced the failure rate of implants placed on previously irradiated bone.9
The most challenging reconstructive endeavor is found in patients afflicted with tissue defect resulting from radical oncologic surgery and who have been subjected to more than 50Gy radiotherapy.10
Studies previously conducted in this type of patients reveal a high rate of complication and low rate of success in the procedures aimed at reconstruction after surgery and radiotherapy.11
CONCLUSIONS
The effects of hyperbaric oxygen therapy on irradiated tissues have been previously studied. Elevation of oxygen tension in hypoxic bones and soft tissues results into the following: fibroblastic proliferation, capillary growth, collagen synthesis and capillary angio-genesis. All the aforementioned events are deemed necessary in order to achieve suitable integration of implants.11
In addition to anchorage benefits achieved with use of bone-integrated implants, this type of rehabilitation elicits a suitable esthetic result by allowing presence of volume in a deficient zone (as consequence of performed resections).The patient experiences more comfort and security since these rehabilitations exhibit suitable anchorage. Moreover, accessibility to the area is preserved, since the patient can easily remove the rehabilitation devices and thus perform suitable hygiene procedures. The area is equally accessible for constant inspection and control of any tumor recurrence.7
REFERENCES
1. Oelgiesser D, Levin L, Barak S, Schwartz-Arad D. Rehabilitation of an irradiated mandible after mandibular resection using implant/tooth-supported fixed protests: A clinical report. J Prosthet Dent. 2004; 91: 310-4. [ Links ]
2. Barber HD, Seckinger RJ, Hayden RE, Weinstein GS. Evaluation of osseointegration of endosseous implants in radiated, vascularized fibula flaps to the mandible: A pilot study. J Oral Maxillofac Surg. 1995; 53 (6): 640-4. [ Links ]
3. Marx RE. Osteoradionecrosis: A new concept of its pathophysiology. J Oral Maxillofac Surg. 1983; 41: 283. [ Links ]
4. Marx RE, Ehler WJ, Tayapongsak P et al. Relationship of oxygen dose to angiogenesis induction in irradiated tissue. Am J Surg. 1990; 160: 519. [ Links ]
5. Howaldt HP, Kainz M, Euler B. Vorast H: Proposal for modification of the TNM staging classification for cancer of the oral cavity. J Craniomaxillofac Surg. 1999; 27: 275-288. [ Links ]
6. Cawood JI, Howell RA. A classification of the edentulous jaws. Int J Oral Maxillofac Surg. 1998; 17: 232-236. [ Links ]
7. Granström G, Jacobsson M, Tjellström A. Titanium implants in irradiated tissue: Benefits from hyperbaric oxygen. Int J Oral Maxillofac Implants. 7; 15-25. 1992. [ Links ]
8. Friedenstein AJ, Latzinik NC, Gorskaya VF, Sidorovich SY. Radiosensitivity and postirradiation changes of bone marrow clonogenic estromal mechanocytes. Int J Radiat Biol. 1981; 39: 537-576. [ Links ]
9. Granström G, Tjellström A, Brånemark PI. Osseointegrated implants in irradiated bone: A case controlled study using adjunctive hyperbaric oxygen therapy. J Oral Maxillofac Surg. 1999; 57; 493-499. [ Links ]
10. Serafin D, Riefkohl R, Thomas I, Georgiade NG. Vascularized rib-periosteal and osteocutaneous reconstruction of the maxilla and the mandible: An Assessment. Plast Reconstr Surg. 1980; 66: 719-725. [ Links ]
11. Greenwood TW, Gilchrist AG: Hyperbaric oxygen and wound healing in post-irradiation head and neck surgery. Br J Surg. 1973. 12; 5, 394-397. [ Links ]
Note This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam Mailing address:
Mailing address:
Mathias Martínez
Policlínico Valencia Torre C piso 3,
consultorio 317
Avenida Carabobo,
2001 Valencia, Venezuela
Teléfono: 0058 241 8202917
E-mail: dr.mathiasmartinez@cantv.net











 texto em
texto em 


