Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista odontológica mexicana
versión impresa ISSN 1870-199X
Rev. Odont. Mex vol.18 no.1 Ciudad de México ene./mar. 2014
Case report
Implant-supported orbit prosthetic rehabilitation in patient with malignant teratoid medulloepithelioma
Elizabeth Garita Medrano,* Vicente González Cardín,§ Araceli Galicia AriasII
* Graduate of the Maxillofacial Prosthesis Specialty, Graduate and Research School, National School of Dentistry, National University of Mexico (UNAM).
§ Head of the Maxillofacial Prosthesis Department, National Cancer Institute, Mexico City, Mexico.
II Methodology Consultant and Professor, Graduate School, National School of Dentistry, National University of Mexico (UNAM).
ABSTRACT
Maxillofacial prosthesis can be described as «the specialty in dental science devoted to the aesthetic rehabilitation by artificial means of intra-and extra-oral structures».1 Orbit prostheses are artificial devices used to substitute the absence of the eye and annex structures (eyelids, lashes and eyebrows). They represent a rehabilitation alternative when surgical reconstruction is either unviable or not preferred by the patient. In our days, in the light of recent research advances, we can make use of bone-integrated implants. To this date they have proven to be the best fixation means in craniofacial prosthetic rehabilitation cases. The clinical case introduced in the present study is that of a male patient exhibiting postsurgical orbital-facial sequels after a carcinoma derived from the central nervous system (CNS) (malignant teratoid medulloepithelioma). Main treatment for this type of carcinoma is ocular globe and circumscribed affected areas exenteration. In this case, this procedure left an orbital-facial defect which was rehabilitated with a maxillofacial prosthesis, fixated to the supraorbital ridge by bone-integrated implants. The aim of the present study was to describe the comprehensive treatment administered to a patient exhibiting this kind of history, from the moment when the condition was diagnosed, its treatment, and the prosthetic rehabilitation of the resulting defect. This study shows the advantages obtained when using bone-integrated implants as a means for prosthesis retention. It is equally observed how this type of rehabilitation greatly improves the aesthetic appearance of patients afflicted with surgical facial sequels, thus achieving a more confident and self-assured reinsertion into society. In order to achieve successful treatment and offer mental and physical welfare to the patient we must work alongside a multi-disciplinary team, to comprehensively solve the case. We can then finally offer the real advantages of prosthetic rehabilitation with a retention means which has proved to be an additional advantage for patients wearing orbital prostheses. Implant usehas bornea great impact in these patients, fostering favorable reinsertion into society, since facial defects are dissimulated and patients can exhibit comfort and security in their day-to-day activities, without fear of a possible prosthesis displacement.
Key words: Orbital-facial prosthesis, malignant teratoid medullepithelioma, implants, bone-integration.
1. INTRODUCTION
Absence of the ocular globe can be due to congenital (hereditary) defects, oncologic surgery, trauma or infections. All of these factors might warrant exenteration. Medullopeithelioma is a primary, childhood, generally benign tumor. It originates in the non-pigmented ciliary epithelium and takes the shape of a whitish-grayish mass or cyst in the iris or ciliary body. This tumor has also been named dictioma, diquitoma or diktioma. Teratoid medulloepithelioma can present different heteroplasia grades (substitution of normal tissue for abnormal tissue, or normal tissue found outside of its habitual location). It can be found in the following tissues: hyaline cartilage, rhabdomyoblasts (germ cells which originate muscle tissue), glial tissue (similar to cerebral tissue) and non-differentiated mesenchymal cells. Also known as teratoneuron (Figures 1 to 3) (2).2



Prosthetic rehabilitation consists on placing a removable prosthetic device to cover the defect and give the patient an aesthetic appearance by replacing the eye and its adjacent structures.
The prosthesis can be kept in place by anatomical means, that is to say, by the defect in itself; by chemical means, which would be the use of a silicon-skin adhesive or by mechanical means among which we find lenses and bone-integrated implants. The latter are considered ideal due to the advantages they offer the patient; they provide excellent results and optimal retention.
Implants are commercially-pure titanium screws in which the metal has been subjected to a special surface treatment in order to guarantee integration to the bone.3
Titanium is the preferred metal due to the following characteristics: it possesses neutral electric load, it is not cytotoxic, it favors cellular contact, it possesses low thermal conductivity and it is very light-weighted. All the aforementioned characteristics render titanium biocompatible and suitable to be implanted into the human body.
When placed within the bone, a bone-integration mechanism is triggered, that is to say, it elicits a functional, structural and direct connection between live bone and implant surface.5 Bone remodeling events take place in two phases: first, there is an osteoclast-elicited resorption increase, for somewhat 15 days, and later there is bone formation, which takes 45 to 70 days and is directed by osteoblasts.6
There are different types of implants according to size, surface and shape. Titanium implants can be classified into smooth or rough surface, according to the type of surface treatment they might have undergone. At the beginning, all implants were smooth, but in our days, scientific literature reports indicate that rough-surface implants exhibit increased bone-integration speed and quality. From the anti-rotary mechanism perspective, they are basically divided into internal-hexagonal and external-friction implants. From the design point of view, implants can be divided into self-twist implants, and implants which are not. Finally, from the size point of view, implants present different diameters and lengths.4
Patients must be suitable in order to achieve success with bone-integrated implants, especially when we want to ensure success with implant permanence in the bone. To warrant whether a candidate is ideal, amount and quality of bone structure where the implant is to be placed must be assessed, as well as the patient's general health status. Another factor to consider is whether the patient was or is going to be irradiated, as well as his motivation and cooperation in the care and preservation of the prostheses which are going to be into place.
Main contraindications for implant 'placement are presence of severe disease which might alter bone metabolism, specific infections, malignant tumors affecting the bone, or extensive periods of radiotherapy.7
Implant bone-integration failure is estimated normal at 2%, skill of the surgeon plays a role as well as consideration of the fact that organisms are always different and their natural processes are sometimes unpredictable and uncontrollable.8
2. BACKGROUND
According to the prosthodontic terms glossary, maxillofacial prosthesis is the branch of prosthodontics dealing with restoration and/or replacement of facial structures and the stomatognathic system by way of prosthetic appliances which might or might not be regularly removed.3
History cannot provide an exact date for when bucco-maxillofacial prosthetic rehabilitation began. Pierre Fauchard was one of the first to contribute to the beginnings of prosthetic work: he manufactured a silver mask to replace part of the lower face of a French soldier hurt in battle.9
Another important moment for maxillofacial prostheses beginnings, was in the XVIth century when Ambroise Pare manufactured a nose prosthesis using gold, silver and paper. In 1889, Claude Martin discovered the use and advantages of ceramics as yet another material used to manufacture nose prostheses.9
With respect to background on bone-integrated implants, it can be mentioned they were initiated in the sixties, at the University of Göteburg, Sweden, and the applied Biotechnology Institute, Göteburg, Sweden, where countless clinical and experimental biology studies were undertaken. The aforementioned studies targeted the expansion of knowledge on the possibilities of medullar and bone tissues reparation and regeneration. They also developed studies on the ideal design of non-biological components which could meet the tissue requirements so as to produce bone-integration at molecular level.10
Professor Per Ingvar Branemark discovered titanium osseo-integration. It was an accidental discovery achieved when observing that microscopic titanium cameras implanted in bone could not be removed, once healing had taken place, due to the fact that the titanium structure had been totally incorporated into the bone.4
In 1965, for the first time, an edentulous patient was treated with bone-integrated implants. These implants exhibited a conical shape to simulate tooth shape, and were experimentally placed in the lower jaw. From that moment onwards studies and research directed to perfecting implant shape and size as well as titanium treatment to achieve ideal bone integration have been constant.11
Bone-integrated extra-oral implants for extra-oral prosthetic retention were used in Sweden, from 1979 onwards, mainly in auricular (ear) prostheses.12
Years later, Branemark, in his efforts to apply this type of treatment, discovered the exceptional characteristics of titanium biocompatibility when placed in direct contact with live bone tissues. Thereafter, these characteristics have been known as osseo-integration.
There are four modalities of Medulloepithelioma reported tumors: embryionic, non-teratoid, teratoid, and adult uveal.
Incidence of central nervous system (CNS) tumors during childhood has been reported as the second cause of death among children under 15 years of age, although most tumors appear in patients after 45 years of age.13
3. CLINICAL CASE REPORT
36 year old male patient (L.R.F) (file number 000031799), born and living in the State of Mexico, single, incomplete secondary school education, jobless.
On June 1st 2003 he was treated at the INCAN (National Cancer Institute). The patient presented exenteration of left orbital globe performed in another institution.
The patient attended our institution due to a previous recurrence diagnosis. Diagnostic studies revealed a tumor invading left conjunctiva and maxillary antrum. There was infiltration to soft and bony tissues. A radical maxillectomy was decided upon with orbital floor resection. A craniofacial approach was decided upon after emitting final diagnosis of malignant teratoid medulloepithelioma. The patient informed of first having noticed the condition five years before, with presence of left eye sclera opacity. Three years before coming to us he attended a physician due to eye pains, loss of visual acuity and general discomfort (malaise).
At the National Cancer Institute he was subjected to a series of reconstructive surgeries with autologous (the patient himself) grafts and flaps. He received prosthetic rehabilitation treatment: and an orbital-facial prosthesis was manufactured. The prosthesis was retained by titan-magnetics (titanium magnetic implants) which were placed in the area's remaining bone.14
3.1. DIAGNOSTIC AIDS
The following tests were conducted as diagnostic aids:
3.1.1. Computarized axial tomography (CAT): this examination consists upon an X ray exploration which yields detailed axial images of the body. Instead of an image, as obtained by conventional x-rays, CAT obtains multiple images when rotating around the body. A computer combines all these images into a final image which then represents a cut of the body resembling a slice. This device creates multiple images in slices (cuts) of the body part subjected to study.15
3.1.2. Visual acuity: can be defined as the eye's capacity to perceive objects. Visual acuity is determined by macular function, which is the most differentiated area of the retina, it is expressed as a fraction, the upper figure represents the distance found between the patient and the table, which generally is 20 feet (6 meters), the lower figure indicates the distance at which a normal-sighted subject could read the same line correctly. For instance 20/20 is considered normal, 20/40 indicates that the line the patient reads correctly at 20 feet (6 meters) could be read at 40 feet (12 meters) by a normal-sighted person.16
3.1.3. Cell blood count (CBC): the term hematic cytometry comes from cytos (cell) and metry (measurement) and haema (blood). Data provided by hematic cytometry (HC) on the red series are: hemoglobin (Hb), hematocrit (Hct) number of red blood cells (RC), average globular volume (AGV), average corpuscular haemoglobin (ACH) corpuscular hemoglobin average concentration (CHb) as well as coefficient of average globular volume concentration (AV-AGV). Data provided by hematic cytometry with respect to white series are: number of white blood cells (WBC), as well as their differential count and alterations. Leukocyte numbers depend upon many factors such as age, weight, smoking habits, birth control hormone consumption, etc. In adult patients, reference values vary between 4 and 12 x 109/L (4,000 to 12,000 µL).17
3.1.4. Clinical chemistry: chemical processes are used to measure blood levels of chemical components. Samples most commonly used in clinical chemistry are blood and urine. There are many different exams to analyze almost all types of chemical components present in the blood or urine. Components can include glucose in the blood, electrolytes, enzymes, hormones, lipids, (fats) proteins as well as other metabolic substances. Some of the most commonly used tests are: blood glucose, electrolytes, enzymes, hormones, lipids, metabolic substances and proteins.18
3.1.5. Culture: culture can be described as bacteria harvesting from an object or tissue in order to allow later reproduction in a suitable culture medium, in order to identify them and assess to which species theybelong.19
3.1.6. Osseous gammagram: bone scan (tracking) is the exploration of the skeleton which allows detection of small functional alterations before they can be radiographically observed.20
3.1.7 Urine culture: is the urine culture conducted to assess symptomatic or asymptomatic urinary tract infections (UTI).21
3.1.8. Parasitology: is the discipline which studies eukaryotic organisms living off a host to whom they can inflict damage.22
3.1.9. Thorax teleradiography: allows visualization of cardiac silhouette (heart and vascular structures) as well as vision of pulmonary fields. This study allows identification of anomalies in heart size and great vessels (aorta and pulmonary artery) as well as lesions within the lungs.20
3.1.10. Magnetic resonance: is a technique designed to obtain images of the body based upon the physical phenomenon of resonance, by applying radio-frequencies to the atoms or dipoles among aligned fields of the sample. This technique allows the study of a sample's chemical or structural information. These images are used in many diagnoses as information source. Nuclear magnetic resonance makes use of resonance properties. MR uses strong magnetic fields which act upon the atoms which compose different substances in the body such as hydrogen. Different tissues emit different waves depending upon their density and water content. A computer translates the patterns of these waves into very detailed images of the body parts where anomalies can be found and therefore used to emit a medical diagnosis. MR produces axial (cross-sectioned) cuts (slices) of the body, similar to cuts obtained from computerized axial tomography, but it can also present projections of different planes: coronary and sagittal. Intra-venous contrast can be used (gadolinium).23
3.1.11. Stereolithography: it consists on creating real models taken from archives into three-dimensional images obtained from a CAT with 0.30.5 mm (CAT with tri-dimensional reconstruction) and stored in a DICOM formatted CD (digital imaging and communications in medicine). Thus, a model with 97.7-99.12% anatomical comparison is obtained.
4. DIAGNOSIS
Diagnosis of medulloepithelioma was emitted after completion of the aforementioned studies. This is a rare CNS tumor affecting generally young children. It exhibits a very aggressive behavior. This lesion belongs to the group of neuro-ectodermal primitive embryonic tumors from its first description in 1926; scientific literature has only reported 40 cases of medulloepithelioma.24
Medulloepithelioma are large tumors, at diagnosis they present symptoms of inter-cranial hypertension. Their radiological image can vary greatly. Initially, these tumors were described as isodense (photon capacity attenuation similar to normal or reference)25 and well-circumscribed with CAT, and did not collect contrast. Magnetic resonance shows hypodense lesions (possessing density or attenuation capacity lower than the considered as normal or reference for a given area or structure),25 these lesions tend to collect contrast at advanced stages of tumor progression. Medulloepithelioma are rapid-growing tumors. They present very poor prognosis. Survival in described cases varies from days to more than 10 years. Average survival is 2-3 months. Amongst factors influencing its fatal evolution are the following: dissemination, radioresistance and high rate of tumor recurrence.26
Prosthetic rehabilitation consists on placing a removable prosthetic device covering the whole defect, granting aesthetic appearance to the patient by replacing the loss of eye and surrounding structures.
5. TREATMENT
5.1. FIRST STAGE
Exenteration is the treatment of choice for this affliction. It consists on removing the ocular globe and surrounding structures affected by the tumor. In the present case, eyelids and soft tissues surrounding them were removed. A radical maxillectomy was performed (surgical technique entailing resection of upper maxillary bone including sections of the malar bone, orbital floor, fronto-nasal apophyses of the lower jaw and half the hard palate)25 as well as orbital floor resection due to the invasion of the tumor into soft and hard tissues. The tumor was reported to measure 7 x 6 x 3.8 cm. It presented free surgical borders. Four ganglia of the neck were resected and showed no tumor evidence.
For a full healing treatment, the patient was subjected to adjuvant radiotherapy, so as to eliminate possible tumor cell remnants and avoid recurrence of the disease. 60 Grays were administered (a grey is a unit derived from the International Unit System which measures absorbed dosages of ionized radiations of a given material). One Gray is equivalent to the absorption of a ionizing energy joule by a kilogram of irradiated material (Figures 4 and 5).27

Upon completion of radiation therapy the patient presented radiation-collateral problems such as grade II mucositis (it is the swelling, irritation and ulceration of mucosal cells which coat the digestive tract). It can develop in any location of the digestive apparatus, from the mouth to the anus. It is a chemotherapy-related side effect which can be very troublesome and painful. The classification of R.L. Capizzi & et al is as follows: grade I: oral mucosa erythema, grade II: small, isolated ulcerations, grade III: confluent ulcerations covering over 25% of the oral mucosa, grade IV: hemorrhagic ulcerations,28 as well as problems in the right eye. These problems included: conjunctivitis (swelling or infection of the membrane that covers the eyelids (conjunctiva),29 blepharitis (inflammation of eyelash) follicles on the edges of the eyelid caused by excessive proliferation of bacteria normally present in the skin)30 as well as xerosthosis (dryness). The patient additionally presented scabs in the left nasal fossa.
To treat all the aforementioned radiotherapy-caused problems, drugs were prescribed according to the condition, namely:
• Caliprene (pilocarpine hydrochloride): this drug is recommended for treatment of symptoms associated to xerostomia, due to hypofunction of salivary glands caused by radiotherapy in cases of neck and head cancer treatment.31
• Meticorten (prednisone): this drug is recommended for treatment of several bone-muscle endocrine diseases, dermatologic collagen, allergic, ophthalmic respiratory hematological neoplasia as well as other types of conditions with documented response to steroid treatment.31
• Micostatin (nystatin): this drug is indicated for treatment of candidiasis in intestinal, vaginal, vulvar and oral mucosa. It is equally used as treatment of skin fungal infection and skin muco-cutaneous fungal infections. This drug is not recommended for systemic use.31
• Terrados (oxytetracycline): oxytetracycline is useful for long term treatment of rosacea and acne vulgaris. It is a primary bacteriostatic agent and it is believed its anti-microbial effect is due to the inhibition of protein synthesis. Oxytetracycline is active against a great variety of gram-positive and gram-negative organisms.31
• Tobradex (dexamethasone and tobramycin sulfate): these drugs are recommended for treatment of infectious processes which entail inflammation of palpebral conjunctiva, bulbar tissue, cornea, anterior segment of the eye, anterior chronic uveitis, and cornea damage. These drugs are equally used as prophylactic agents for postsurgical infections and inflammations. Main usage of combined therapies is warranted in the presence of inflammatory situations in which there is high risk of secondary infection (eye trauma, including surgery), penetration of foreign substances or objects, or chemical burn due to radiation or thermal agents. The component alcohol dexamethasone controls inflammatory response.31
• Vantal (benzydamide hydrochloride): this formula represents an anti-inflammatory antiseptic and bucco-pharyngeal analgesic agent. It is used as adjuvant in mouth and pharynx discomfort. It is used in the following instances: cheilitis, stomatitis, gingivitis, periodontitis, pericoronitis, mucositis and oral mucosa inflammation due to dental surgery, dental prostheses, orthodontic treatment, extractions, pharyngitis, tonsillitis, laryngitis, epiglottitis, glositis, abscesses, leukoplakia, as well as inflammation entailing oral inflammation such as candidiasis.31
At a later point, the resulting defect was covered with a transverse rectus abdominis muscular-cutaneous flap (TRAM). The flap was micro-vascularized. This technique consists on transferring a block of skin fatty tissue from the infra-umbilical abdominal region to the region to be reconstructed.32
After recovery of this reconstructive surgery, thinning of the facial flap was required. Liposuction of the flap was equally undertaken due to the excess of fatty tissue which increased the area volume (Figure 6).

It was evident that cancer treatment left as sequel a facial defect with absence of the eye. These problems could not be totally corrected with surgical methods (plastic or reconstructive surgery (Figure 7). Therefore, the patient was offered a prosthetic rehabilitation alternative.

When, after consulting with the patient, the physcians decided to place a bone-integrated implant for prosthetic rehabilitation, the left orbit had to be deepened, a left retro-auricular flap was taken as well as a graft from the costal cartilage in order to obtain sufficient supporting hard tissue to be able to insert titanium implants (Figure 8).

5.2. SECOND PHASE
Placement of implant and costal graft was previously determined with the help of stereolithography. Thus, secure and accurate implant placement was ensured (Figure 9).

5.2.1. Work model: a facial impression of the patient was taken in order to obtain a master working model to then develop surgical guides. In this process, Vaseline was previously applied over hair, eyebrows and eyelashes in order to avoid their becoming stuck to the impression material. A reversible hydrocolloid-type impression material (alginate) was placed on the patient's face. Care was taken to preserve free airways and enable respiration. A gauze was placed above the alginate so as to contain the material and avoid overflow, on top of it, a plastered gauze was placed to give support to the impression and thus avoid rips or deformations at the moment of separating it from the face. The material was allowed to set for about ten minutes. After this, the patient was requested to gesticulate in order to help impression removal. The impression thus obtained was run with type III plaster (gypsum) (el-mix). When this material was set, the impression was removed and the edges were trimmed.
5.2.2. Surgical guide: once the plaster model was achieved, construction of a surgical guide was undertaken to ease bone-integrated implants placement and also to ensure their suitable angulation and parallelism degree. All this was achieved after the surgeon had indicated the best location where to place the implants according to the amount of bone present. This guide was manufactured with number 80 acetate (Figures 10 to 12)(11).



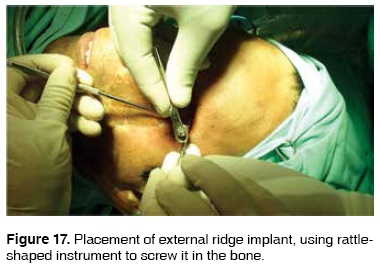
5.2.3. Implant placement: implant placement into the bone was achieved with the help of the surgical guide, which was placed in the orbital area after performing the incision to uncover the bone. Its use is essentially to insert the first burr to open the bone through the guiding tube. After this, once inclination and location are marked, the guide is withdrawn; to then continue increasing the size of the surgical burr until reaching the width of the implant which is to be placed. In the present case, three bone-integrated titanium implants were used: Titan Magnetics, Straumann, «extra-oral» type. Two were placed in the inner canthus (edge) and one in the outer canthus. All implants measured 4.1 mm in width and 6 mm length (ref 043.030S, lot 1016 ti 2007-04; ref 043.030S, lot 1026, 4.1 mm, 6. mm ti 2010-03 ref 043.030S, lot 1017, 4.1 mm 6.0 mm ti 2007-11) (Figures 13 to 17) (14, 15, 16). Implants protruded in the mouth after healing. Two months were permitted to elapse in order to change the healing cap for the magnetic device. This had the aim of becoming the receptor of the future prosthesis which would carry in the back a magnet which would antagonize with these magnetic devices screwed into the implant (Figure 18).





Prosthetic rehabilitation was undertaken six months after implant placement. A facial impression was taken in order to obtain a work model. It was achieved with Straumann implant impression devices (Figure 19). The positive version was obtained by running type IV plaster (Vel-mix). Manipulation implants were previously placed in the laboratory (Figure 20). These provided us with exact implant placement in the patient in the work model. We could thus work on the model and simulate the real-life situation.


5.2.4. Resin base plate: a resin base plate was manufactured in order to contain the magnets. This base would form the back section of the prosthesis. It was manufactured with self-curing clear acrylic. It was placed after having placed the magnets into the laboratory implant, scattering powder and liquid over the previously treated model with plastic-acrylic separator in the desired area. Once the acrylic had set, resin plates were removed from the model in order to polish it and trim excesses (Figures 21 and 22).


5.2.5. Eye characterization: using the right eye as a model, the left eye prosthesis was manufactured.
All eye characteristics such as sclera color and vascularization as well as iris color were copied, so as to obtain as much likeness to the eye as possible, to then place in the silicon prosthesis and obtain a natural effect. The eye prosthesis was manufactured with self-curing acrylic resin with use of ferrous pigments and acrylic paints.
5.2.6. Orbital prosthesis wax modeling: the process begins by situating the eye on the working model, for it to assume the same location of the patient's eye. This is achieved placing it in the patient once a simulation of the future eyelids are placed in pink wax. Care must be taken to reach pupil center and eye depth in exact replica of the counterpart.
Pink wax is modeled, patient's characteristics such as eyelid thickness and opening are replicated, bone and soft tissue are copied. Wrinkles, expression lines, bumps and dark circles around the eyes are equally replicated. Allthese characterization effects are constantly corroborated by placing the model on the patients face.
5.2.7. Placement of prosthesis in muffle: a prosthodontic muffle was used. Type III plaster was used for the base of the muffle. The acrylic guide was placed upon the eye prosthesis. This was performed in order to avoid displacements of the eye and incorrect eye positioning when the de-waxing process was undertaken. Once the plaster had set, two layers of plaster-acrylic separator were applied to then proceed into the placement of the counter-muffle, to finally incorporate type IV plaster (Vel-mix) (Figure 23).

5.2.8. De-waxing process: once the muffle plaster had set, it was placed in a press and then taken to a pot with 100° hot water, where it remained for approximately 15 minutes. Once this time had elapsed, the press was removed and the muffle opened. At this point, the wax, now liquid, could run. More hot water was applied with powder detergent; both muffle counterparts were brushed with a plastic bristle brush, in order to avoid wax and fatty remnants in the plaster (Figure 24).

5.2.9. Medical grade silicon intrinsic characterization: with the patient present, his skin color blemishes, dark circles, moles etc were replicated. This coloring was given to the silicon with «Flock» fibers (textile fibers). Different hues were made up according to the area to be replicated, and then added according to the desired effect (Figures 25 and 26).


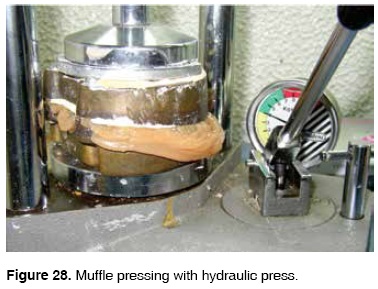
5.2.10. Silicon pressing: silicon was placed within the muffle with a fine spatula (spatula used to mix dental cements); it was placed in sections, according to the color given to each portion, e.g. darker color around the eye (eyelids and circles) and the rest of the silicon on the other areas of the muffle. Once this procedure was completed, the muffle was closed by joining both counterparts. It was then taken to a hydraulic press, with 400 kg pressure. It was then left for 24 hours to vulcanize (Figures 27 and 28).

5.2.11. External characterization of eye prosthesis: after setting, the silicon was recovered from the muffle (Figures 29 and 30). At this point, over-extended borders of the prosthesis were trimmed. The prosthesis was polished and finally placed on the patient to proceed with the external characterization. Characterization was achieved with oil paint and acrylic monomer as diluting agent. Paint was applied to the prosthesis with brushes of different thicknesses according to the area which was being characterized. This procedure aimed at providing accurate skin color as well as blemishes, freckles, scars, or darkening of specific areas. Finally, when the color of the prosthesis was deemed satisfactory, a coat of medical-grade silicon was applied in order to seal the color and avoid its fading. This silicon coat must be left 24 hours to dry. After this period eyelashes and eyebrows were applied with a dermal needle: the hair was passed through its center so as to insert it into the silicon. Amount, position and length of eyelash and eyebrow hair were replicated, so that the prostheses resembled to the utmost the patient's natural appearance (Figure 31).



6. DISCUSSION
Maxillofacial prostheses play an important role in rehabilitation after surgery caused by diseases which leave facial sequels. Facial prosthetic rehabilitation provides psychological benefits and better quality of life for patients afflicted with these sequels.
Presently, the use of implants has eliminated many of the problems connected to the use of prostheses retained into place with medical-degree adhesives.
In the past, mobility of soft and even bony tissues compromised retention of the prostheses as well as the adhesive, and therefore, patients' acceptance was low. When these new prostheses are used, the patient experiences ease to place it and remove it as well as retention quality while performing different activities. Patients are unconcerned when sweating, sneezing, coughingor when performing harsh movements. These prostheses are easily placed into their proper position, contrary to adhesive-assisted prostheses which can be placed incorrectly.
Patients wearing implant-supported prostheses are more satisfied with the rehabilitation treatment than patients wearing adhesive-retained prostheses. They inform of a better quality of life.
Another benefit of bone-integrated rehabilitation is ease for the prostheses' hygiene. If the prosthesis were to have adhesive remnants this endeavor would prove to be more difficult. Adhesive remnants in conjunction with skin humidity on the prosthesis can cause fungi in cases when cleansing is not correctly undertaken; this, in the long run, can affect the skin in contact with the prosthesis. Nevertheless, this has not yet been reported.
Use of adhesives can be a hindrance for natural gesticulation movements, either due to patient's fear of prosthesis dislodgements or as a result of negative experiences. In these cases the prostheses are not natural-looking and the patient's expression is rigid.
An additional point would be patient's dependence: they must carry the adhesive at all times to avoid accidents in case sweat would weaken the adhesion, or in cases the patient must travel. An additional problem would be cases when the adhesive is hard to get or no longer for sale.
The length of life of the prosthesis is also at stake, since the patient should exert the utmost care when withdrawing it, if this is not the case, he could tear the edges when withdrawing the prosthesis.
The patient studied in this clinical case presented problems with soft tissues surrounding one of the implants, specifically the one on the outer canthus. Tissue at that location kept growing up to the point of completely covering the magnet. Surplus tissue was excised in three different instances, but healing resulted in new tissue increase (Figures 32 to 34) (33). It was then decided to allow the healing process until the device was covered and later test whether the magnet managed to fulfill its retention purpose through the tissue. This was anticipated by using magnets with 12,000 gauss strength. Once this was achieved, there was no longer a need to expose the device covered by tissue. In this manner, it was discovered that the magnet worked through the tissue and we were no longer forced to inflict on the patient minor surgical events which could entail discomfort and infection risks.



7. CONCLUSIONS
In order to achieve successful treatment and provide mental and physical welfare to the patient a multi-disciplinary team is required in order to comprehensively solve the case. In this fashion, the patient will receive the full benefits of a prosthetic rehabilitation treatment with a retention device which will prove to be a great advantage for patients wearing orbital prostheses. Implant use has borne great impact in these patients since they allow their re-insertion into society, conceal facial defects and offer comfort and security in their daily activities, free of the fear of possible prosthesis dislodgements (Figures 35 and 36).


REFERENCES
1. Alvarado E, González V, Jiménez R. Reporte de casos clínicos de prótesis combinadas (intraoral y extraoral). Gaceta Mexicana de Oncología. 2003. pp. 30-37. [ Links ]
2. Zona gratuita. Diccionario de oftalmología [Internet]. 2002-2004 [acceso 10 de enero de 2007]. Disponible en: http://www.zona-gratuita.com/curiosidades/DicOftalmologia/M.htm [ Links ]
3. The Academy of Prosthodontics Foundation. The glossary of prosthodontic terms. 7th edition. USA: 1999: p. 83. [ Links ]
4. Cuesta J. ¿Qué es la implantología? Implantología estética, S.L [Internet]. Enero 2006 [acceso 27 de octubre de 2006]. Disponible en: http://www.implantologiaestetica.com/que_es_%20la_implantologia.htm [ Links ]
5. Gel G. Elementos de fijación en las epítesis craneofaciales retenidas por implantes. Abteilungsleiter Epithetik; p. 1-17. [ Links ]
6. Massardo L. Enfermedades óseas metabólicas: osteoporosis. Apuntes de reumatologia [Internet]. 2006 [acceso19 octubre de 2006]. Disponible en: http://escuela.med.puc.cl/publ/Apuntes-Reumatologia/Osteoporosis.html [ Links ]
7. Changetal. Treatmentsatisfaction with facial prostheses. The Journal of Prosthetic Dentistry. 2005; 94 (3): 275-280. [ Links ]
8. Toljanic J et al. Osseointegrated craniofacial implants in the rehabilitation of orbital defects: an update of a retrospective experience in the United States. The Journal of Prosthetic Dentistry. 2005; 94 (2): 177-182. [ Links ]
9. Jankielewics I et al. Prótesis bucomaxilofacial. Barcelona: Quintensence; 2003: pp. 38, 234, 434. [ Links ]
10. Menneking H et al. Medidas de protección en las epítesis faciales ancladas en el hueso. Springer-Verlag. 1998; 46: 579-582. [ Links ]
11. Peñarrocha M. III Congreso Nacional de la Sociedad Española de Cirugía Bucal. Dentalword [Internet]. Disponible en: http://gbsystems.com/news/107.htm [ Links ]
12. McKinstry R. Fundamentals of facial prosthetics. ABI Profesional Publications; Estados Unidos de América. 1995: p. 80. [ Links ]
13. Kleihues P. Brain tumours: morphological aspects and classification. Brain Pathology. 1993; 3 (3): 251-306. [ Links ]
14. INCaN. Expediente clínico del paciente. [ Links ]
15. Wikipedia, enciclopedia Libre. Tomografía axial computarizada. [Internet]. 28 octubre 2006 [acceso 9 de noviembre 2006]. Disponible en: http://es.wikipedia.org/wiki/Tomograf%C3%ADa_axial_computarizada [ Links ]
16. Exámen de agudeza visual. Enciclopedia Médica en Español [Internet]. 4 agosto 2005 [acceso 2006 de noviembre 2010]. MedlinePlus. Disponible en: http://www.nlm.nih.gov/medlineplus/spanish/ency/article/003396.htm [ Links ]
17. Abreu LM. Interpretación de la citometría hemática. Programa Nacional de Actualización y Desarrollo Académico para el Médico General [Internet]. 1999 [acceso 16 de noviembre de 2006]. Disponible en: http://www.drscope.com/pac/mg/a5/mga5_p5.htm [ Links ]
18. Health System. La quimica clínica [Inernet]. University of Virginia 2007 [acceso 8 de febrero de 2007]. Disponible en: http://www.healthsystem.virginia.edu/UVAHealth/adult_path_sp/clinchem.cfm [ Links ]
19. Aboitiz C. ¿Qué es un cultivo? [Internet] bbmundo. 2000 [acceso 8 de febrero de 2007]. Disponible en: http://www.bbmundo.com/bbsalud/leerNota.asp?idSub=6&idArt=301 [ Links ]
20. Sociedad Española de Medicina Nuclear. Ejemplos de exploraciones [Internet]. 19 de septiembre de 2006 [acceso 9 de febrero de 2007]. Disponible en: http://www.semn.es/publico/ejemplos.html [ Links ]
21. Rodríguez F et al. Indicaciones y valoración clínica del urocultivo Revista Medicine. [Internet]. 2002; [acceso 9 de febrero de 2007]. 08 (61): 3270-3272 Disponible en: http://db.doyma.es/cgibin/wdbcgi.exe/doyma/mrevista.go_fulltext_o_resumen?esadmin=si&pident=13023967 [ Links ]
22. Torres M. Parasitologia para enfermería [Internet]. Pontificia Universidad Católica de Chile. 2001 [acceso 9 de febrero de 2007]. Disponible en: http://escuela.med.puc.cl/paginas/udas/Parasitologia/Parasitol_03.html [ Links ]
23. Wikipedia. [Internet] Resonancia magnética nuclear. Enciclopedia Libre. 2007 [acceso 9 de febrero de 2007]. Disponible en: http://es.wikipedia.org/wiki/Resonancia_magn%C3%A9tica_nuclear [ Links ]
24. Encinas M. Tumores de iris-cuerpo ciliar [Internet]. Tumores Intraoculares.Org [acceso 12 de enero de 2007]. Disponible en: http://www.tumoresintraoculares.org [ Links ]
25. Instituto Científico y Tecnológico de la Universidad de Navarra. Diccionarios elmundo.es. [Internet]. 2001 [acceso 10 de febrero de 2010]. Disponible en: http://diccionarios.elmundo.es/diccionarios/cgi/lee_diccionario.html?busca=isodenso&submit=+Buscar+&diccionario=8 [ Links ]
26. Burger PC. Tumors of the central nervous system. Atlas of tumor pathology. Washington, DC: 1994. [ Links ]
27. Wikipedia. [Internet] Gray. Enciclopedia Libre. 2007 [acceso 10 de febrero 2007]. Disponible en: http://es.wikipedia.org/wiki/Gray_(unidad_radiobiol%C3%B3gica) [ Links ]
28. Health System. El Control de la mucositis [Internet]. University of Virginia. 2004 [acceso 9 de febrero de 2007]. Disponible en: http://www.healthsystem.virginia.edu/UVAHealth/peds_oncology_sp/manmuc.cfm [ Links ]
29. MedlinePlus. Conjuntivitis [Internet]. Enciclopedia Médica en Español. 2005 [acceso 9 de febrero 2007]. Disponible en: http://www.nlm.nih.gov/medlineplus/spanish/ency/article/001010.htm [ Links ]
30. MedlinePlus. Bleferitis. Enciclopedia Médica en Español. [Internet] 2006 [acceso 9 de febrero de 2007]. Disponible en: http://www.nlm.nih.gov/medlineplus/spanish/ency/article/001619.htm [ Links ]
31. Thomson. Diccionario de especialidades farmaceúticas PLM. Biblioteca Médica Digital [Internet]. Facultad de Medicina. UNAM. 2006 [acceso 9 de febrero de 2007]. Disponible en: http://www.facmed.unam.mx/bmnd/dirijo.php?bib_vv=6 [ Links ]
32. Lozano J. Reconstrucción mamaria con el colgajo musculocutáneo recto abdominal transverso (TRAM). Revista Anales. [Internet] 2005; 28 (2) [acceso 9 de febrero de 2007]. Disponible en: http://www.cfnavarra.es/salud/anales/textos/vol28/sup2/suple7a.html [ Links ]
 Mailing address:
Mailing address:
Vicente González Cardín
E-mail: vicentegonzalezcard@hotmail.com
Note
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam











 texto en
texto en 


