Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista odontológica mexicana
Print version ISSN 1870-199X
Rev. Odont. Mex vol.17 n.4 Ciudad de México Oct./Dec. 2013
Case reports
Treatment of craniofacial region wounds caused by dog bite
Víctor Rodrigo Velázquez Reyes,* Martín Gilberto Flores Ávila,§ Arturo Gómez Pedroso BalandranoII
* Maxillofacial Surgery Resident, ISSSTE Lic. Adolfo Lopez Mateos Hospital, Mexico City, Mexico.
§ Physician attached to Maxillofacial Surgery Specialty, ISSSTE Lic. Adolfo Lopez Mateos Hospital, Mexico City, Mexico.
II Head of Service and Professor of the Maxillofacial Surgery Specialty, ISSSTE Lic. Adolfo Lopez Mateos Hospital, Mexico City, Mexico.
ABSTRACT
Patients arriving with dog bite lesions in the craniofacial region are treated at the Maxillofacial Surgery Service. These patients require inter-consultation with the maxillofacial surgery service. Patients wounds are cleansed with a three-fold (solution in thirds) solution for 30 minutes, to then proceed to wound closure. Other protocols are restricted to wound closure and cleansing and antibiotic administration. Wounds caused by animal bites are complicated. These wounds can be macerating, sharp, lacerating or avulsive. Antibiotic, tetanus and rabies prophylaxis are indispensable. The most important aspect is cleansing and primary closure of the wound. Post-surgical treatment includes tight control to prevent or control infection and when needed, secondary revision of the scar with reconstruction purposes. In the present study, data from 58 patients were gathered. The following variables were examined: data on existing or non-existing infection according to region, age, gender, exposition time from the moment of aggression to hospital treatment, as well as anatomical region of the lesion.
Key words: Wounds, dog-bites, risk factors, infections.
INTRODUCTION
We would like to point out the relevance of this study: Rabies is defined as a deadly, acute , infectious and communicable disease. It affects the nervous central system and is caused by a virus of the lyssavirus gender and the Rhabdoviridae family. It is transmitted through virus-containing saliva from a contaminated subject or animal. It can also be transmitted through laboratory-infected material. It represents one of the mammals zoonotic diseases transmitted to mankind mainly through the saliva of an infected animal from a bite, scratch or constant lick on skin or mucosa. Rabies is a deadly disease, in order to prevent it any subject who has been bitten, scratched or licked by a rabid animal, or an animal suspected of being sick, must, with medical consent, receive specific anti-rabies treatment. This treatment could be suspended as soon as laboratory diagnosis and epidemiological studies would so warrant.
In Mexico, between 1992 and 1999 and average of 24 fatalities per year were recorded. When studying age groups, the most affected (48%) was the 5-14 years group. The 15-44 age group followed in frequency, where fatalities reached 23%. Nevertheless, it is important to point out that in 90% of all cases, medical attention was not requested.1
These lesions are mostly wrongly considered innocuous, therefore, it is reckoned that, in developed countries only a fourth of them are reported. The most affected age group is within the 5-14 age rank. Male over female ratio is 2 to 1.
Of all domestic animals attacks reported, 80 to 90% are caused by dogs and 6 to 8% by cats. Other wildlife animals are foxes (6%), wolves, skunks and bats. Less frequent animals (3%) are sheep and horses.2
98.349 subjects sustained injuries in the aforementioned period, This means that 99 out of every 100,000 inhabitants sustained canine aggression. Antibiotic treatment was only prescribed to 34.5% of afflicted patients. Aggressions on humans were caused by dogs (71%), chiroptera (23%) and 6% by other species like cattle, raccoons foxes and skunks.1,2
In Mexico there is a rabies national prevention and control program, it encompasses massive vaccination of dogs and cats. This has elicited decrease of human rabies cases from 1991.3 Social importance of rabies is related to its lethality which, in humans is almost 100% it is estimated that in Mexico about 90,000 subjects are attacked by dogs.1
Nowadays, wounds in the facial region caused by dog-bite are very frequent in our society. Their successfull treatment represents a challenge. Animal bites are always contaminated with the same bacteriae present in human bacterial flora, generally they include Pasteurella multocida or a micro-organisms variety which cause zoonotic diseases such as fever due to ratbite.1
Another more recent source reckons that in the USA between one and two million subjects are attacked by dogs and cats. The type of these lesions are of diverse intensity, but over 50% of all victims are pre-school and school-age children. The most afflicted face areas are nose and ears. Lesions progress from superficial to amputations.4
The assailant (aggressor) animal can be of varied race and aggressiveness. It must be considered whether he was provoked or not. At any rate, the most frequent site of the lesion is related to the patient's age: in our country, statistical evidence reveals the following most frequent sites: face, arms, body trunk, legs and scalp. Due to their size and weight, pediatric patients are most prone to this type of incidents. Children, being curious and adventurous tend to approach animals, which in some cases even are the family's pet.2
Documented national and international incidence reveals that up to 65% of lesions are located in the head, face and neck, especially in children under four years of age.2,3
Severity of lesions was assessed according to Lackmann classification:
LACKMANN'S CLASSIFICATION:
I. Superficial lesion, without muscle involvement.
II. Deep lesion, with muscle involvement.
III. Deep lesion with muscle involvement and tissue defect.
IVa. Class III combined with vascular damage of nerve lesions.
IVb. Class III combined with bone damage or organ involvement.5,6
Force generated by an animal's bite can reach 820 kg per square inch. Depending on the animal's dental morphological characteristics, bites can be penetrating or puncture wounds (caused by cats, which are associated to greater incidence of infection) avulsion wounds (dog), crashing or lacerating wounds (horse), or any combination of the aforementioned which damage skin, muscle and bones.2
MICROBIOLOGY OF BITE WOUNDS
These wounds are contaminated by a great variety of micro-organisms, among which we can find aerobic bacteria ( Streptococcus spp, Bacillus subtilis , Capnocytophaga canimorsus , Clostridium perfringens , Eikenella corrodens , Klebsiella , Moraxella catarrhalis , Pasteurella multocida , Pseudomonas , Serratia marcescens , Staphylococcus aureus et epidrmidis , among others) anaerobic bacteria (Prevotella spp, Fussobacterium spp, Bacteroides spp, Arachnia propionica , Eubacterium spp, Veillonella spp, among others) as well as other germs ( Clostridium tetani , Leptospira spp, Hepatitis B virus, herpes simplex virus (HSV), rabies virus.7-15
PATIENTS AND METHODS
Data were gathered from 58 patients. Patients belonged to heterogeneous ethnic backgrounds and were part of the population seeking treatment at the Hospital Regional ''Lic. Adolfo Lopez Mateos'' ISSSTE (Regional Hospital ''Lic. Adolfo Lopez Mateos'', Mexico City) from march 2006 to may 2008. Since patients were deemed emergency cases, they were all treated, irrespectively of whether they were entitled to treatment or not. The following patient variables were studied: data of presence or absence of infection, type of craniofacial region affected, age, gender, exposition time since aggression to hospital treatment, and anatomical location of lesion. Patients depicted in figures 1 and 2 are distinct representatives of this type of lesions: they were bitten at home by their own family pets and presented predominantly craniofacial region lesions.

SPECIFIC OBJECTIVES
1. To determine incidence and frequency of dog bite-wounds cases located in craniofacial region of patients seeking treatment at the Maxillofacial Surgery Service.
2. Ascertain characteristics of injured (aggressed) patients within the study period., that is to say, assess age, gender, exposition time from moment of aggression to hospital treatment, presence or absence of infection and anatomical region involved.
TREATMENT OF DOG-BITE WOUNDS
Treatment in the Institution offered to this type of patients is usually sufficient to minimize collateral effects of this type of aggressions sustained by patients. Moreover, infections triggered by this type of wounds are normally controlled if timely treated.
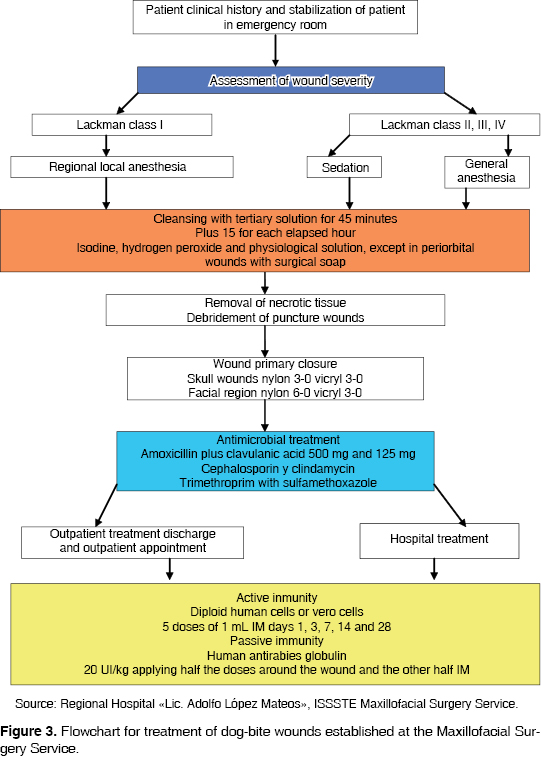
All 58 patients were treated with the following anti-microbial scheme: Trimethroprim with Sulfamethoxazolate (dosage: 10 mg per kg) every 12 hours for 7 to 10 days. Amoxicillin with clavulanic acid 50-80 mg/kg/dayly every 12 hours (Red Book, CDC 2006), 50-80 mg/kg/day for 7 to 10 days.7 This presentation is the one institutionally used, it was complemented with an paracetamol-type analgesic, dosed at 15 mg per body weight kilogram, per day. Also used were diclofenac or naproxen at measurable dosage established in Mexican and international scientific literature, and according to service flow diagram of Maxillofacial surgery as depicted in figure 3. Cleansing was performed with tertiary solution: 9% physiologic solution, isodine and hydrogen peroxide) for 45 minutes, with an additional 15 minutes more for each hour elapsed with isodine, peroxide and physiological solution. Exception was made for peri-orbitary lesions which were only cleansed with surgical soap. Wound suture was performed in consultation with the Maxillofacial Surgery Service which provides statutes for handling of that type of wound when lesions are found within the craniofacial region. Human anti-rabies immunoglobulin is not applied to ambulatory patients (outpatients); it is only given to patients requiring hospitalization, or in cases when the aggressor animal cannot be put in observation or is an unknown animal.4,6,7,11-14
RESULTS
Results shown in the present study were gathered along three years from March 2006 to May 2009, based upon duty hours and Maxillofacial Surgery Service database (Regional Hospital ''Lic. Adolfo Lopez Mateos'' ISSSTE, Mexico City). The aforementioned data revealed a total of 58 patients with dog-bite wounds. Analyzed cases revealed the following: presence or absence of infection according to region, age, gender, exposition time from moment of aggression to hospital treatment, and affected anatomical region. Data submitted in Graphs were analyzed with SPSS statistical analysis program. The program exhibited the following data.
In figure 4 the following can be observed: regions most affected by infections are the cranial region (25%) and the lower third (17%). This took place in patients which sustained infections after tertiary cleansing treatment (based on 9% isotonic saline solution, isodine foam and hydrogen peroxide) followed by medication.

In the figure 4 data the following can be observed: percentages of patients exhibiting infections according to the affected craniofacial region. Within the analysis of this graph it can be observed that patients presenting greater frequency of infections were those with wounds in the cranial region; they were followed by patients sustaining wounds in the lower facial third. This can be explained due to the presence of hair in the area which provides an infection-prone zone since there is presence of a physical barrier or mechanical deterrent for the proper cleansing of the wound (in spite of performing trichotomy in the wound-afflicted area). With respect to lesions in the lower third of the face it can be deducted that present infections were caused by the communication existing among oral cavity wounds: the bacterial flora of the animal mixed with that of the aggressed patient. Moreover, there were minimal data of infection in patients sustaining wounds in the middle and upper third of the face.
Figure 5 describes age groups most vulnerable to this type of wounds. It can be seen that pediatric patients are the group most vulnerable group to dog bites. Another additional reason would be, due to his short bodily height, the proximity of the patient's face to the dog's snout. Moreover, the animal has the basic instinct to aggress vital zones such as the cervical or facial region in order to make his prey vulnerable.16
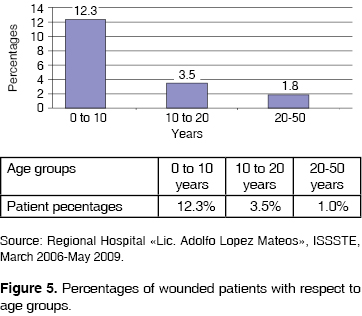
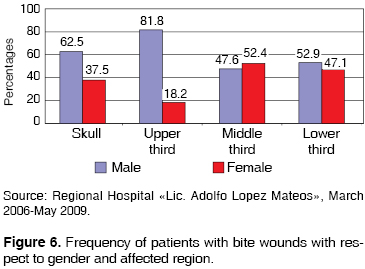
Figure 6 depicts a marked increase in the relationship existing between male and female patients facial wounds due to dog-bites. 57.9% of all patients were male and 42.1% female. This could be due to the fact that boys could be more curious about other living things, in this case dogs, and would be more prone to exhibit an attack-like behavior towards the animal. A relationship can be found between the gender of the patient and the involvement of facial thirds. Moreover, male patients exhibited high involvement of upper facial third followed by cranial region and lower facial third. There was a decrease in the middle facial third. Female patients exhibited a slightly larger percentage. In all affected regions, male patients presented higher number of cases: 57.9%
The Table depicted in figure 7 illustrates the time it takes from the moment a patient is bitten until his hospital treatment. In this graph we can observe that the time elapsed in our hospital from the moment a dog-bitten patient arrives until he receives treatment is 45 to 60 minutes. These patients are considered a priority. Some patients presented longer exposition times (90 to 120 minutes) this implies greater infection risks and longer cleansing times.16
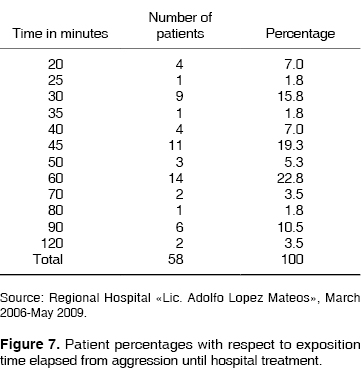
Figure 8 depicts cleansing time with respect to treated patients' percentages. It can be observed that the greater number of patients (33%) received cleansing for 15 minutes, 26.5% were cleansed for 45 minutes. These were deemed the best cleansing times for patients which, as can be seen in figure 7, had been exposed for 60 minutes.

DISCUSSION
Dogbites are relatively common lesions. There are reports of informed incidence pointing out that 172 to 740 for every 100,000 subjects sustain this type of injuries per year. This range reflects the fact that finding proportions of duly documented actual dog-bite cases is variable or erratic; they represent a range of 10 to 50% within an open-care population as reflected by the study conducted by the Secretaria de Salud (Ministry of Health) in the 1995 official notification.1
Lackmann & al reported that lesions caused by dog bites resulted in tissues flattening and tearing. The lesions become more severe when the victim is shaken. This fact can be observed in figures 1 and 2 where patients sustained lacerating wounds.5 In 2007, Gonzalez & al reported the fact that forces elicited by a dog bite can be crushing forces able to generate a 820Kg pressure per square centimeter.2 Wolf conducted a study in 1998 where he reported that American Pit Bulls can generate this type of pressures in one bite.17 Lesions can be simple scratches or perforations, but can reach greater defects in bone and soft tissue as mentioned by Lackmann and Wolf in their studies. This fact is quite relevant, since the study conducted by Lackmann was the base for the wound classification bearing his name.5,17 These wounds show a tendency to become infected as a result of primary bacterial inoculation of normal flora present in the dog's snout. Incidence of reported infection varies from 5 to 30% according to Raffi & al in their 1987 study.8 Weinert, Talan and Murphy concur in stating that the most common pathogens in this type of wound are Staphylococcus aureus and Pastorella multicoda. The latter is characteristic of this type of lesions.9-11 Treatment of dog bites has evolved with the passing of time. In the past, late closure or second intention healing were accepted bearing in mind possible infection risks and the fact that dog bites should not be treated with first intention closure. These tendencies are mentioned as past history in articles written by Lackmann, Stefanopulous, Morgan, Akhtar and Wolf.5,7,14,16,17
In all patients recorded in the present study a primary closure was performed after cleansing with the tertiary solution (isodine, peroxide and 0.9% physiological solution). This was performed initially in order to limit infection or inoculation of bacteria existing in the aggressing animal's snout. This would also be true in cases where the wound exhibits communication to the patient's oral cavity. These facts have been recorded in the guide for dog bites treatment provided by the Maxillofacial Surgery Service based on studies conducted by Monroy (2009), Goldstein (1992), Morgan (2005), Akhtar (2006) and Wolf (1998).12-14,16,17
Gonzalez (2007) reported that tetanus is infrequent. In our days, rabies rarely develops due to vaccine drives and aggressive surgical and medical handling. Rabies is the most ancient known viral zoonosis, it has a 100% lethality. As reported by Monroy 2009 rabies is an acute disease, transmitted by a virus which affects primarily animals, and occasionally man. To this date, it has proven to be a lethal disease. Transmission to man is basically through the bite of a rabid animal. It is a universal disease affecting wild and domestic animals.
CONCLUSIONS
In the period comprised between march 2006 to may 2009, only 12.3% patients were infected, which is tantamount to 7 patients out of the 58 patients treated in that period. The cranial region presented greater number of infections. Handling established by the Maxillofacial Surgery Service has been effective, it consists on the following: cleansing with tertiary solution for 45 minutes plus 15 additional minutes per hour elapsed since the aggression with isodine, hydrogen peroxide and physiological solution, except for periorbital wounds which were cleansed with surgical soap. Neverhteless, the treatment is occasionally too aggressive since it elicits sweeping saprophytic bacterial flora in affected regions, which can cause infection. There are other additional external factors, such as the case of patients presenting wounds in the cranial surface, with presence of hair and poor wound hygiene exhibited by the patient. With respect to lesions in the upper third, 81.1% were located in the left auricular region; 72.7% were found in the palpebral zone. No cleansing with tertiary solution was performed on periorbital area lesions; germicidal soap and 0.9% solution were used in these cases in order to avoid damage to the eyeball (caused by chelation of isodine and peroxide). This solution was used for the same time as the tertiary solution. With respect to the middle third 81% were located in the naso-labial region; 4% of them became infected. In the lower third infection increased to 17.6%; most lesions were found in the sub-mandibular and chin areas. When studying wounds with respect to gender, it can be stated that there was predominance of male patients (57.9%) with respect to female patients. With respect to exposition time, it can be noted that, in our hospital, time elapsed from the moment of dog bite patient arrival to treatment is 45 to 60 minutes, since these patients are considered critical. Other patients had to suffer longer expositon times (90 to 120 minutes) this fact could elicit infection. In figure 8 the graph depicts greater percentages (33%) of patients receiving 15 minutes cleansing periods; followed by 24.6% patients being cleansed for 45 minutes. This could be considered the best cleansing time to prevent infections in patients as consequence of exposition to dog bite wounds in any region, without incurring the risk of a saprophytic bacterial sweep in the affected area. These procedures, in combination with antibiotic and immunological treatment for rabies prevention allow the decrease of infection caused by this type of lesion.2,12
REFERENCES
1. Secretaría de Salud. Notificación a la Norma Oficial Mexicana NOM-011-SSA1993. Para la Prevención y Control de la Rabia. Diario Oficial de la Federación, 25 de Enero 1995. [ Links ]
2. González ME, Hernández CA. Protocolo de manejo en mordeduras por animales. Revisión de la literatura e informe de dos casos. Revista ADM . 2007; LXIV (6): 250-254. [ Links ]
3. Schvartzman SD, Pacin MB. Lesiones por mordedura de perro en niños. Arch Argent Pediatr . 2005; 103 (5): 389-395. [ Links ]
4. Abuabara A. A review of facial injuries due to dog bites. Med Oral Patol Oral Cir Bucal . 2006; 11. E 348-50. [ Links ]
5. Lackmann GM, Draf W, Isselstein G, Tollner U. Surgical treatment of facial dog bite injuries in children. J Craniomaxillofac Surg . 1992; 20: 81-6. [ Links ]
6. Rainer KM, Hölzle F, Poxb C, Thurmüller P, Wolff KD. Animal bite injuries to the head: 132 cases. British Journal of Oral and Maxillofacial Surgery. 2006; 44: 235-239. [ Links ]
7. Stefanopoulos PK, Tarantzopoulou AD. Facial bite wounds: management update. Int J Oral Maxillofac Surg . 2005; 34: 464-472. [ Links ]
8. Raffi F, Baron D, Drudgeon HB, Nicolas F, Courtieu AL. Pasteurella multocida bacteraemia: report of thirteen cases over twelve years and review of the literature. Scand J Infect Dis . 1987; 19: 385. [ Links ]
9. Wienert P, Heiss J, Rinecker H, Sing A. A human bite. Lancet . 1999; 354 (9178): 572. [ Links ]
10. Talan DA, Citron DM, Abrahamian FM, Moran GJ, Goldstein EJC. Bacteriologic analysis of infected dog and cat bites. N Engl J Med . 1999: 340: 85-92. [ Links ]
11. Murphy E. Pathology resident microbiology of animal bites. Clinical Microbiology Newsletter . 2008; 30: 7. [ Links ]
12. Monroy A, Behar P, Nagy M, Poje C, Pizzuto M, Brodsky L. Head and neck dog bites in children. Otolaryngology-Head and Neck Surgery . 2009; 140: 354-357. [ Links ]
13. Goldstein EJ. Bite wounds and infection. Clin Infect Dis . 1992; 14: 633-638. [ Links ]
14. Morgan M. Hospital management of animal and human bites. Journal of Hospital Infection . 2005; 61: 1-10. [ Links ]
15. Guy RJ, Rosen T, Orengo IF, Wolf JE. Successful treatment of acute head and neck dog bite wounds without antibiotics. Ann Plast Surg . 1986; 1: 45-48. [ Links ]
16. Akhtar N, Smith MJ, McKirdy S, Page RE. Surgical delay in the management of dog bite injuries in children, does it increase the risk of infection? J Plast Reconstr Aesthet Surg . 2006; 59: 80-85. [ Links ]
17. Wolf K. Management of animal bite injuries of the face: experience in 94 patients. J Oral Maxillofac Surg . 1998; 56: 838-843. [ Links ]
Note This article can be read in its full version in the following page http://www.medigraphic.com/facultadodontologiaunam Mailing address:
Arturo Gómez Pedroso Balandrano
Mailing address:
Arturo Gómez Pedroso Balandrano
E-mail: argopebal@hotmail.com











 text in
text in 


