Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista odontológica mexicana
versión impresa ISSN 1870-199X
Rev. Odont. Mex vol.17 no.4 Ciudad de México oct./dic. 2013
Original research
Changes in the position of cranio-cervical complex skeletal structures after an orthognatic surgery event
Iris Ocampo Fonseca,* María de la Paz Consuelo Aguilar Saavedra,§ Francisco Manuel Sánchez RamosII
* Former resident, Orthodontics Graduate Program, General Hospital Manuel Gea Gonzalez Mexico City.
§ Member of Scientific Committee, Mexico's Orthodontics Association, Former coordinator, Orthodontics specialty, General Hospital Manuel Gea Gonzalez, Mexico City.
II Guest Professor, Orthodontics Graduate Program, General Hospital Manuel Gea Gonzalez, Mexico City.
ABSTRACT
The aim of the present study was to conduct research on presence of changes in skeletal structures' position of the cervical-cranial complex after treatment involving orthognatic surgery. 30 patient files were reviewed. Patients were afflicted with initial class I, II and III malocclusions which had been treated with orthognathic surgery. With the help of lateral skull X-rays, measurements were taken of pre- and post-surgical positions of vertebrae, hyoid bone, as well as skull rotation. It was found that patients subjected to combined surgery presented greater range of skull rotation changes in a posterior direction (p = 0.006). Female patients presented tendency to posterior skull rotation, and exhibited distance decrease from atlas to skull base (p = 0.23). In surgical patients, it is important to timely identify these skull rotation changes since they might elicit relapse of performed orthognathic surgery and/or occipital headache.
Key words: Vertebrae, orthognathic surgery, cervical column, hyoid bone, cranial rotation.
INTRODUCTION
The aim of the present study was to explore the presence of changes in the position of bone structures of the cranio-cervical complex in patients afflicted with class I, II, and III skeletal malocclusions who have been subjected to orthognathic surgery.
Biomechanics is the branch of Physics which studies the mechanics of forces and their effects, inasmuch as they apply to the human body or animals. Biomechanics studies embodies dynamic and static state. Statics studies bodies in remain at rest and in equilibrium as a result of forces exerted unto them. When all forces act simultaneously upon a body, their effect is cancelled, and therefore, no movement is elicited. At that point, the body can be considered in equilibrium (balance). Dynamics is the science that studies bodies in movement.1
Normal posture of human beings requires a complex biomechanical function among skeletal and muscle systems, articulations, ligaments and nervous system.2-4
A correct posture must provide balance of the human body on its articulations. Balance depends on neutralization of gravity forces exerted by counter-forces of mass centers of each body segment (one upon the other); these in turn must be aligned with articulations found between each segment.
Brodie, in 1971 stressed the importance of homeostasis in the mechanism of posture ''...changes at the head's support point require alterations in the neck's muscles activity so as to readapt the posture of the head and prevent its unbalance''. The mechanism of the head involves more than a simple weight re-distribution. The posture of the head is also influenced by sight, the cochlea, as well as proprioceptive factors. (Roaf, 1977); it can be modified by oropharyngeal mechanisms connected to the functional maintenance of airways. (Linder-Aronson 1979).5
Skeletal structures analyzed in the present study were: cervical vertebrae, skull and hyoid bone.
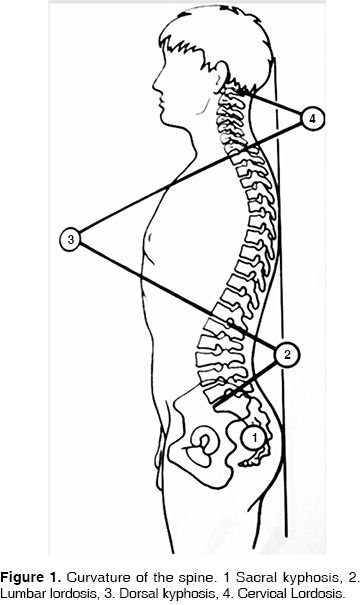
The backbone (spinal column) is composed of 7 cervical vertebrae, 12 thoracic vertebrae, 5 lumbar vertebrae, 5 fused sacral vertebrae and 3 to 4 fused coccygeal segments. From a frontal plane, the spine looks straight and symmetrical. From a saggital plane, the spine presents several curvatures: lordosis and kyphosis. Lordosis is a concavity of the spine formed by vertebrae: there can be cases of lumbar or cervical lordosis. Kyphosis is a convexity formed by vertebrae; there is sacral kyphosis and dorsal kyphosis.1 Presence of spinal curvatures increase the rachis resistance to axial compression forces6-8 (Figure 1).
Cervical spinal cord is divided into two sections: the upper cervical rachis (sub-occipital) which contains the first cervical vertebra (atlas), and the second cervical vertebra (axis), as well as the lower cervical rachis which extends from the lower side of the axis up to the upper surface of the first dorsal vertebra. These two segments of the cervical spinal chord complement each other to undertake pure rotation, inclination or flexure movements with extension to the head.3
Flexure of the head on the cervical rachis and flexure of rachis over the dorsal rachis are dependent upon anterior muscles. At the level of the upper cervical rachis, major and minor anterior straight muscles determine a flexure in the atlanto-occipital articulation. The long muscle of the neck and the major anterior straight muscle determine flexure in underlying articulations. The long muscle of the neck determines straightening and rigidity of cervical rachis. At a distance of the cervical rachis, and therefore endowed with longer lever arm, the necks' anterior muscles act as powerful head and cervical rachis flexors. These are the supra-hyoid and infra-hyoid muscles ( mylo-hyoid and anterior belly of the digastric muscle which bond the lower jaw to the hyoid bone and the infra-hyoid muscles such as the thyro-hyoid, sterno-hyoid, sterno-thyroid and omo-hyoid muscles). Simultaneous contraction of these muscles determines the descent of the lower jaw, but in cases when the lower jaw is blocked against the upper jaw by the simultaneous contraction of masticatory muscles, contraction of supra- and infra-hyoid muscles determines the flexure of the head on the cervical rachis and flexure of the cervical rachis on the dorsal rachis, as well as the strengthening of the cervical lordosis. These muscles play an essential role in the statics of the cervical rachis.3,7
The skull is supported by the cervical spinal cord. Nevertheless it is neither centered nor balanced on the spinal cord. Balance is lesser due to the position of the lower jaw which is located underneath the anterior section of the skull, causing more skull weight to move forward. For this reason there is no balance among skeletal components of head and neck.9
CERVICAL- SKULL SYSTEM DYNAMICS
The cervical-skull system is an intrinsic component of the body's upper quadrant. It is composed of head, neck and scapular girdle. It is formed by skeletal structures (skull and cervical vertebrae) connected by articulations (atlanto-occipital, atlanto-axial and vertebral) muscle attachments, ligaments, aponeurosis, innervations and blood supply.6 The dynamics of this system consist in preserving the balance of the skull on the spine. This is achieved when the eyes are horizontally fixed.In this position, the occlusal plane is horizontal, which is also the case of the auricular-nasal plane, which passes through the upper border of the external auditory conduct and the anterior nasal spine. During the biomechanical process of the skull-cervical dynamics, a system of levers is formed:
• There is a fulcrum point located at the level of the occipital condyles (Figure 2).
• Resistance formed by the weight of the head applied to its center of gravity located close to the sella turcica (Figure 2).
• Potency constituted by the strength of the sub-occipital muscles which at all times must compensate for the weight of the head which tends to make it fall in a forward direction (Figure 2).

This situation of the head's gravity center explains the relative potency of the posterior muscles of the nape of the neck with respect to the flexor muscles of the neck. Extensor muscles (sub-occipital muscles) fight gravity whereas flexor muscles (supra-hyoid and infra-hyoid muscles) are helped by gravity.3
In 1976, Torgen and Solow associated cranial posture, type of respiration and facial structures. Specific facial patterns could be associated to the type of natural position of the head.10
In a class I skeletal pattern, the flexure/extension cranial dynamics is normal, as well as spinal curves. In cases of mandibular retrognathia, there is a decrease in spinal curves and cranial extension when there is no other etiology associated to the postural disorder. In cases of mandibular prognathism, there is an increase of spinal curves and cranial flexure when there is no other etiology associated to the postural disorder. These spinal adaptations to skeletal relations class II and III, although frequent, are not systematic.6
A class II malocclusion brings head and shoulders forward, with a rectified cervical column. Mandibular condition in turn the cervico-scapular position. In a class III malocclusion the tongue is brought to a low position and the head is displaced towards the bach.6
Cleall & al did not find differences in the head's posture in class I and class II patients.11
The relationship existing among Biomechanics - Skull- mandibular- spinal- hyoid region and airways can be considered an ''Indivisible Functional Unit''. M Rocabado suggested that a precise diagnosis is required to normalize relationships among the aforementioned structures. This diagnosis should be based on an objective method of radiographic evaluation which determines the biomechanical aspects of the skull-mandible-spine relationship. In this analysis, Dr Rocabado assesses: 1. Skull angular and cervical spine angulation. 2. Distance between occipital base and posterior arch of the atlas and its association to craniofacial pain syndromes.3. Position of the hyoid bone in the determination of the spine physiological curvature. 4, Hyoid spinal relation and position of lingual rest, and 5. Airways.12
Morphological characteristics of subjects exhibiting increased cranio-cervical angle present decreased facial depth, increased mandibular inclination as well as increased anterior lower facial height.13
The hyoid bone does not possess bone articulation or articular relationship. Nevertheless, it does exhibit firm relationship to the anterior cervical spine through the cervical fascia. Supra-hyoid and infra-hyoid muscles perform concurrent functions with the hyoid bone in order to achieve normal functioning. These muscles depend on the hyoid bone and its relationship with the anterior region of the spine, as well as the scapular girdle. In turn, the hyoid bone plays a role in the determination of the spines physiological curvature.12
The position of the hyoid bone is a reflection of ligament muscular tensions and of inserted fascia. The relationship of the hyoid bone and the spine has been studied by many researchers such as Ricketts (USA), Elkimo, Ingervall and Carsson (Sweden) and Dibby (South Africa). These studies determine cranio-spinal and mandibular relationships, spinal curvatures and airways. The study of these biomechanical relationships allows planning of treatments (orthodontic and/or surgical-orthodontic) which will ensure and facilitate long lasting results.12
Athananasiou in 1989 defined orthognathic surgery as a procedure designed to correct acquired or congenital dento-facial deformities; a procedure aimed at improving facial and dental esthetics and to normalize stomatognathic functions.14
Grecco, in 1990 mentioned the fact that orthognathic surgery procedures designed to correct dento-facial anomalies affect the size and position of soft tissues and alter pre-existing relationships among soft and hard tissues.15
According to Solow and Tallgren (1987) the position of the hyoid bone is coordinated to facial morphology, head and spinal posture.12 Posture changes (Gustavsson, 1972, Winnberg 1988) and changes in the inclination of the lower jaw (Graber 1978, Tallgren and Solow 1987) have been reported as influencing hyoid bone position.15
Wenzel, 1989, Katakura 1993 and Hochban reported noticeable decrease of pharyngeal sagittal dimensions and increase of head extension after mandibular retro-positioning procedures.14,15 Solow, 1967, Tallgren 1977, Posnick 1978, and Showfety 1987 mentioned the fact that extension of the head had been associated to increase of the anterior-posterior maxillary-mandibular dimension, as well as increase in the anterior facial height.14
Solow (1996) showed a compensatory posture to maintain airways free. The extension of the spine-skull relationship allows separation of the base of the tongue and the soft palate from the posterior pharyngeal wall.14 Achilleos, Krongstad, Lyberg (2000) demonstrated the fact that after correction of mandibular prognathism by way of surgical procedure with mandibular retro-positioning, the base of the tongue and the soft palate result elevated; and as a result of this elevation airways decrease and the cranio-cervical angle experiences an increase (2.7°). Nevertheless, in the long term, there is no record of airway decrease, this would then explain the compensatory functional readjustment exhibited by hyoid bone, tongue and cervical muscle system in order to preserve the airway pattern.14
Takagi (1967), Fromm and Lundberg (1970), Wickwire (1962), Athanasiou (1991), Lew (1993), and Enacar (1994) state the fact that osteotomies performed in order to retro-position the lower jaw, exert influence in the position of the hyoid bone, and as a consequence, in the position of the tongue.14 In 2000 Gu found that in patients subjected to retro-positioning of the lower jaw, the posture of the head increased its extension and the hyoid bone moved in a downward and posterior direction.16
C Phillips (1991) conducted a study where he assessed changes in cranial posture in patients previously subjected to different types of surgical procedures. He observed that those patients who had been subjected to maxillary intrusion, maxillary intrusion with mandibular advance, mandibular advance as well as maxillary intrusion combined with mandibular retro-positioning, presented decrease in the vertebral skull angle (skull anterior rotation). Patients subjected to mandibular retro-positioning exhibited head flexure as well as increased vertebral skull angle (skull posterior rotation). Patients subjected to maxillary and mandibular surgery exhibited increase in head flexure. No patient presented changes in cervical inclination or cervical lordosis. One year after surgical procedure, the vertical skull angle mean increased (skull posterior rotation) in groups subjected to maxillary intrusion, mandibular advance and maxillary intrusion combined with mandibular advance. This means that in these groups, after surgical procedure, there was flexure of the head, and a year after surgical procedure, patients experienced the tendency to return to pre-surgical posture. This angle remained unaltered in patients subjected to mandibular retro-positioning. In patients subjected to only one surgical event, (maxillary or mandibular), values for cervical skull angle and vertebral skull were similar to pre-surgical values. For patients subjected to maxillary intrusion with mandibular advance, the posture of the head remained with increased flexure when compared to pre-surgical values while cervical skull angles were decreased (anterior rotation). Patients subjected to maxillary intrusion with mandibular retro-positioning experienced flexure of the head, but differences were not statistically significant. Even though there was a tendency to a decrease of cervical lordosis after mandibular retro-positionig, neither this measure nor any other measure related to cervical inclination revealed statistically significant changes.5
METHOD
Files of 200 patients treated at the Orthodontics and Reconstructive Plastic Surgery departments were reviewed. Cases fulfilling inclusion criteria were selected. The sample was composed of 30 patients with skeletal Class I, II or III malocclusion who had undergone ortognathic surgery.
Files included exhibited pre- and post-surgical lateral skull X-rays. Post-surgical X rays were taken at least 3 months after surgery. Patients were over 18 years of age, of both genders, and exhibited Class I, II or III pre-surgical skeletal relationship. Files of patients afflicted with degenerative systemic diseases and growth alterations were excluded.
The problem posed in the present study was to determine whether there were changes in the position of cranio-cervical complex skeletal structures after performing orthognatic surgery in patients with Class I, II and III malocclusion.
In the sample used in the present study, 60% were female (n = 18) Group average age was 21 years, average 21 years with SD:4.
Cephalometric tracings were performed on the pre- and post-surgical lateral skull X-rays. For this purpose, a number 0.02 stylograph was used on an acetate tracing sheet. Performed cephalometric tracings were angles SNA, SNB, ANB as determined by planes Nasion-point A and Nasion-point B. Vertical facial dimension was also millimetrically assessed by considering the distance of the Frankfort plane and the chin point projected over a vertical line perpendicular to the Frankfort plane. With the help of cephalometric tracings described by Dr Mariano Rocabado the following measurements were assessed in pre- and post-surgical lateral skull X-rays: skull rotation (skull-odontoid angle), distance from occipital base to the atlas posterior arch (Figure 3), cervical curvature, hyoid triangle (Figure 4), cranio-cervical angle (Figure 5) and cervical inclination (Figure 6).




Pre- and post-surgical data were correlated with ANB measurements, vertical dimension, type of surgery and type of maxilla-mandibular skeletal relationship with postsurgical cervical values.
RESULTS
The aim of the present study was to ascertain whether there would be changes in the position of the cranio-cervical complex skeletal structures after orthognatic surgery in patients exhibiting class I, II, or III maxillo-mandibular skeletal relationship. This is an important fact for it is known that changes in the position of bone structures in the cranio-cervical complex, can cause relapse or occipital headache.12 Multiple types of orthognatic surgery were performed. They were grouped into four categories, according to the area in which the surgery was performed and to the amount of performed osteotomies. Group 1 included surgeries entailing the upper jaw; group 2 comprised procedures performed on the lower jaw, Group 3 encompassed surgeries entailing one osteotomy in the upper jaw and osteotomies in the lower jaw, Group 4 included triple surgeries (upper and lower and chin). 50% of the sample belonged to group 3 (this group included combined surgery mainly (n = 13) maxillary impaction and chin sliding (n = 1), segmented surgery and chin sliding (n = 1), and advance Lefort I plus chin sliding (n = 13). Group 1 followed in frequency (33.3%). This group included upper segmented surgery (n = 1), maxillary impaction (n = 1) and Lefort I (n = 8). Even though maxillary impaction (vertical dimension modifiers) surgeries were included, vertical dimension skeletal surgical modifications were not significant. Significant changes were only achieved in the maxillary-mandibular anterior-posterior relationship with an ANB change average of 6° (p < 0.0001). Non significant values in vertical dimension are due to the fact that there were only 2 cases of maxillary impaction, and all the remaining surgical procedures required correction of an anterior-posterior skeletal discrepancy.
The most frequent surgical procedure was combined surgery n = 13 (Lefort I advance with mandibular retro-positionig). Significant changes were achieved in patients who underwent combined surgery who presented changes greater than 3.9° in the skull posterior rotation (p = 0.006). Female patients showed a significant decrease (0.86 mm) in the distance from occipital base to atlas posterior arch (p = 0.023). This meant female patients exhibited tendency to the posterior rotation of the skull with respect to C 1.
PRE-SURGICAL MAXILLARY-MANDIBULAR RELATIONSHIP
According to maxillary-mandbular relationship and Steiner's normality classification, 80% of cases exhibited out-of-the-norm measurements (0 to 4° of ANB angle). For the whole group post-operative mean ANB angle was -2.4°. The male patients group exhibited -3.9° (SD 4.46°), and the female patients group exhibited -11.3° (SD 5.14°) p = 0.10.
Facial Vertical Dimension Average was 103.5 mm (SD 9.9). Male patients exhibited 111.4 mm (SD 7.7) and female patients showed 98.3 mm (SD 7.6) p ≤ 0.0004.
When examining pre-operative maxillary-mandibular skeletal relation type it could be observed that class III appeared in 66.7% cases, followed by class I (20%) and finally class III with 13.3%. In male patients, initial maxillary-mandibular skeletal relation type was 8% for class I, 17% for class II and 75% for class III. In female patients proportions were 28% for class I, 11% for class II and 61% for class III.
PRE-OPERATIVE CERVICAL MEASUREMENTS
Angle formed by McGregor Plane and odontoid plane . Average for this angle was 102.7° (SD 8.8°) Male patients exhibited a 107.58° angle (de 7.5) which implied tendency to skull anterior rotation. Female patients exhibited a 99.44° angle (SD 8.1°) p = 0.01 which implies tendency to skull posterior rotation but with values within norm (96°-106°).
Distance between occipital base and atlas' posterior arch . Average in distance between occipital base and atlas was 5.5 mm (SD 3.6) values were within norm (4-9 mm). Males exhibited 7.9 mm (SD 3.2) which meant tendency to skull anterior rotation with values within norm. Females exhibited 4.02 mm (SD 3.07), p = 0.004 which implied tendency to posterior skull rotation with values within norm.
Cervical curvature . Average of cervical depth was 4.1 mm (SD 4.1) Males exhibited 3.2 (SD 3.86) and females 4.69 (SD 4.30) p = 0.29.
Hyoid bone vertical position . The distance from point H to H' was 0.32 mm (SD 6.07). This implied the fact that the hyoid bone was vertically elevated with respect to the Me-C3 plane. Males exhibited a distance of 4.29 mm (SD 3.26) in the vertical position of the hyoid bone with respect to Me-C3 plane. Females exhibited 2.3 mm (SD 6.12) p = 0.99. abnormal position of the hyoid bone over Me-C3 plane, vertically elevated.
Cranio-cervical angle . Average of cranio-cervical angle was 88.8° (SD 8.5°). Males exhibited 86.5° (SD 6.40) and females 90.33° (SD 9.58°) p = 0.99. This implied the fact that, in relation to the skull, C2 in males was in a more posterior position when compared to females.
Cranio-cervical inclination . Average of cervical inclination angle was 85.23% (SD 6.8°) Males exhibited 85.15° (SD 7.09) p = 0.95 and females 85.17° (SD 6.88). Values of cervical inclination (C1 to C4) with relation to the skull were similar for both genders.
POSTOPERATIVE CEPHALOMETRIC AND CERVICAL MEASUREMENTS CHANGES
There were statistically significant changes in the ANB angle average before and after the surgical event. It increased 6° (positive) p < 0.0001 (Table I).
No statistically significant differences were observed with respect to type of surgery in the ANB angle approximation to the norm, (p = 0.27), neither were there norm-approximation differences in ANB angle among genders (p = 1). Nevertheless, when male and female groups were independently assessed it was observed that in male patients ANB angle average increased from -3.9° to 3.6o (implying a 0.3o difference) p < 0.0001. In female patients ANB angle average increased from -1.38o to 5.38o (6.0o increase) p < 0.0001.
67% of all patients reached class I maxillary-mandibular skeletal relationship. Patients with initial class I maxillary-mandibular skeletal relationship remained in class I after the surgery. This was due to the fact that they were subjected to surgeries which entailed no modification of point A or point B (chin sliding), or, at any rate, modification was only from 2 to 3 degrees in ANB and the patient continued in class I skeletal relationship (maxillary impaction). Combined and triple surgeries were also performed. They were performed on patients with vertical facial patterns and therefore, was initially within norm. With the surgical procedure, the anterior-posterior relationship was only modified by 3-4°, preserving thus a class I skeletal relationship. The greater surgical changes were in a vertical direction. 33% of the sample showed changes towards a class II maxillary-mandibular skeletal relationship. In this group were patients presenting an initial class III skeletal relationship as well as one case of class I. Patients with skeletal class III underwent a combined surgery, advance Lefort I or triple surgery. Those patients did not reach a skeletal class I relationship,; surgical planning must not only be based upon skeletal relationship, it must also consider soft tissues. Therefore, in certain cases, due to esthetic reasons, the ANB angle is not brought to normal values. The patient presenting initial class I skeletal relationship, who was brought to class II was a case presenting severe vertical problems, where ANB was initially shown to be within normal values. The most severe problem was found in the vertical dimension, therefore, a combined surgery was planned. For esthetic and functional reasons it was decided to preserve a class II skeletal relationship. 100% of patients presenting class II initial maxillary-mandibular skeletal relationship remained in class II. This was due to the fact that this group underwent maxillary impaction, segmental and chin sliding, and these procedures do not modify the ANB angle. 45 of patients with initial class III maxillary-mandibular skeletal relationship changed to class I, 35% to class II and 20% persevered in skeletal class III. Patients in which class III persisted were severe cases, where, although ANB was brought to values closer to norm, they notwithstanding remained negative.
There were no observed statistically significant changes in vertical dimension when comparing pre-operative period with post-operative p = 1 Changes were not found in vertical dimension average in male patients (p = 0.35) or female patients (p = 0.82).
According to type frequency of maxillary-mandibular skeletal relationship after orthognathic surgery, the following could be observed: 43.33% presented class I, 44.43% presented class II and 13.33% exhibited class III (Figure 7).

Paired t test revealed there were no statistically significant changes in the angle formed by MacGregor plane and odontoid plane in the postoperative period p = 0.62. Nevertheless, when analyzing changes in the position of cranio-cervical complex skeletal structures according to the type of orthognatic surgery, it was observed that patients who underwent combined surgery (Lefort I advance and mandibular retro-positioning) presented greater proportion of changes in the posterior rotation of the skull. They presented decrease of 3.91° (p = 0.006) in the angle formed by McGregor and odontoid planes. There were no changes in the average of skull rotation angle in males or females (p = 0.40 and p = 0.23 respectively) (Table II).
There were no significant changes (in millimeters) in the vertical position of the hyoid bone or in the cervical curvature, neither were there changes in the degree average of the cranio-cervical angle and the inclination of the spine from the pre-surgery to the post-surgery period p = 0.33, p = 0.59, p = 0.13 and p = 0.90.
In cases where there were changes in measurements, when pre-surgery and post-surgery periods were compared with paired t test, the following statistically significant results were obtained:
• 12 cases presented increase in the angle formed by McGregor and odontoid planes (anterior skull rotation) and average 102.9° (pre-surgery) and 107.9° (post-surgery) was observed, the mean between both values was -5° (SD: 2.9) p ≤ 0.0001. These 12 patients with decrease in the same angle (posterior rotation) exhibited a mean of 105° in pre-surgery and 101.1° in post-surgery periods, with a mean 3.9 between both (SD: 3), p ≤ 0.0001.
• 14 cases presented increase in the distance from occipital base to atlas (skull anterior rotation) pre-surgery mean was 5.8 mm and post-surgery 7.6 mm, therefore mean between both measurements was -1.7 mm (SD: 1.1) p ≤ 0.0001.
• 8 cases presented decrease in this same measurement: in pre-surgery phase they presented 5.8 mm, and in post-surgery phase they presented 4.3 mm, mean was 1.5 mm (SD: 1.2 mm) and p ≤ 0.0001.
• 9 cases exhibited decrease of cervical curvature; they measured 4.4 in pre-surgery phase, and 3.4 in post-surgery phase, thus presenting mean of 2.7 between both (SD: 2.4) and p = 0.002.
• 16 cases exhibited increase in cervical curvature; in pre-surgery they presented mean of 2.9 mm and in post-surgery 4.9 mm, thus -2 mean between both (SD: 0.93) and p ≤ 0.0001.
• 17 cases presented elevation of the hyoid bone; in pre-surgery period they presented mean of -0.29 mm and after surgery a mean of -3.5 mm, thus observing mean between both of 3.2 (SD: 4.1) and p = 0.003.
• 10 cases presented descent of the hyoid bone; in pre-surgery period they presented mean of -065 mm and after surgery 2.5 mm with a mean of -3.2 (SD: 3.9) and p = 0.007.
• 8 cases presented decrease of the cranio-cervical angle, in pre-surgery they showed a 90o angle and in post-surgery a 85.5° angle, thus mean of 4.5° (SD: 2.8) and p = 0.0001.
• 17 cases which presented decrease of this same angle showed a pre-surgery mean of 87.5o and post-surgery mean of 92.3o, thus a mean of 4.8 between both (SD: 4.3) and p ≤ 0.0001.
• 14 cases of cervical inclination decrease of the angle exhibited in pre-surgery period a 84.8o mean and in post-surgery 81.21, thus a mean between both of 3.6 (SD: 2.8) and p ≤ 0.0001.
• 15 cases which presented increase of this same angle showed pre-surgery mean of 85.6% and post-surgery measurement of 89.3°, thus a -3.6 mean between both and p ≤ 0.0001 (Table III).
DISCUSSION
Wenzel, 1989, Katakura, 1993 and Hochban, 1996, reported decrease in pharyngeal sagittal dimensions and increase in head extension after a procedure of mandibular retro-positioning.13,15
Solow, 1967, Tallgren 1997, Posnick 1978 and Shofety 1987, reported correlation between extension of the head with increase in anterior-posterior maxillary-mandibular dimension and increase in anterior facial height.14
Solow 1996 demonstrated the fact that extension of the head is a compensatory posture which preserves free airways.13
Achilleos, Krogstad, Lyberg 2000, reported that mandibular retro-positioning decreases airways and causes increase of the cranio-cervical angle (2.7°). He reported a compensatory functional readjustment of the hyoid bone, tongue and cervical musculature to preserve a free airway.13
The aforementioned concepts, when compared to results obtained in our study explain the reason why patients who underwent combined Lefort I surgery( advance with mandibular retro-positioning) presented a tendency to skull posterior rotation, possibly in a compensatory effort to preserve free airways.
Takagi 1967, Fromm and Lundberg 1970, Wickwire, 1972, Athanasiou 1991, Lew, 1993 and Enacar 1994 agreed in reporting the fact that mandibular retro-positioning had an influence on the position of the hyoid bone.13 Gu, in 2000, reported that in patients subjected to mandibular retro-positioning, an increase of head extension could be observed, as well as the downward and backward transit of the hyoid bone.15 In the present study we did not find significant changes in the hyoid bone vertical position, nevertheless, hyoid bone changes in anterior-posterior direction were not determined.
Bracco, Deregibus, Piscetta and Ferriario (2002) informed that an increase in vertical dimension could be associated to the extension of the head over the cervical spine as well as a decrease of cervical lordosis (mainly C1, C2, and C3).6 In our sample, vertical dimension was not modified. Cranio-cervical angle and cervical lordosis basically remained unchanged in the post-surgical period.
Phillips (1991) reported that patients subjected to vertical dimension modification and maxillary-mandibular anterior-posterior distance modifications exhibited decrease of the vertebral cranial angle (skull anterior rotation). Patients subjected to mandibular retro-positioning exhibited flexure of the head as well as an increase of the vertebral cranial angle (skull posterior rotation). Patients subjected to maxillary and mandibular surgery presented increase in head flexure. None of the patients exhibited changes in cervical inclination and in cervical lordosis.
In our study changes in vertical dimension were not significant, contrary to anterior-posterior changes Based on these findings we beg to state that maxillary-mandibular skeletal changes in anterior-posterior direction cause changes in the skull rotation.
CONCLUSIONS
When establishing comparisons among patients who did exhibit cervical measurement changes from pre-surgical to post-surgical periods, and when separating values indicating increase or decrease, all cervical changes resulted statistically significant. The sample used in the present study included a great amount of surgical procedures; results exhibited significant changes only in patients subjected to combined surgery. This type of surgery constituted the greater part of our sample, and did reveal statistically significant data. Nevertheless, upon separating the sample into those who experienced increased or decreased cervical measurements, all values resulted statistically significant. In this study it was clear that there were significant changes in cervical measurements when comparing pre and post-operative periods. Values reveal increase or decrease of measurements, this might be due to the diversity of surgical procedures included in the sample. It is probable that behavior of cervical measurements (value increase or decrease) might be due to the surgery as well as skeletal changes undergone by the patient. The present study only recorded pre-and post-surgical changes in the position of skeletal structures of the cranio-cervical complex. Neither the presence of relapse in surgical results was recorded nor the determination of occipital headache was determined.
The present study led us to conclude the following:
• There were changes in the position of bone structures of the cranio-cervical complex.
• Patients subjected to combined orthognathic surgery exhibited decrease in the angle formed by McGregor and odontoid plane. Decrease of this angle indicated skull posterior location possibly triggered as a compensation to the decrease of pharyngeal spaces.
• In female patients there was significant decrease in the distance found between skull base and atlas, this indicated a tendency to skull posterior rotation. This could trigger sub-occipital compression and occipital headache as a consequence. These changes could also cause post-surgical relapse.
The present study did not assess symptomatology of any kind. Nevertheless we suggest the need to conduct studies to assess clinical manifestations or symptoms as well as post-surgical relapses.
REFERENCES
1. Le Veau B. Biomecánica del movimiento humano . 2nd ed. Trillas, 1991. [ Links ]
2. Herkowitz HN, Garfin SR, Balderston RA, Eismont FJ. Columna vertebral . 4o ed., McGraw Hill, 2000; pp. 1121-1146. [ Links ]
3. Kapandji IA. Cuaderno de fisiología articular . 2nd ed. Masson, tomo 3, 1991, pp. 13-55. [ Links ]
4. Cooper JM, Glasgow RB. Kinesiología, Panamericana, 1973, pp. 50-87. [ Links ]
5. Phillips C, Snow M, Turvey T, Proffit W. The effect of othognathic surgery on head posture. European J Orthod . 1991; 397-403. [ Links ]
6. Francois RD. Tratado de osteopatía craneal análisis ortodóntico diagnóstico y tratamiento manual de los síndromes craneomandibulares . Panamericana, 2002, pp. 145-150. [ Links ]
7. Rouviere H, Delmas A. Anatomía humana . 9o ed., Masson, tomo 2, 1987, pp. 15-30. [ Links ]
8. Gardner E, Gray DJ, Rahilly RO. Anatomía estudio por regiones del cuerpo humano . 2nd ed., Salvat, 2001, pp. 23-38. [ Links ]
9. Okeson JP. Tratamiento de oclusión y afecciones temporomandibulares. 4o ed., Mosby, 1999, pp. 29-65. [ Links ]
10. Preston CB, Todres JI. The relationship between ortho head posture and head posture measured during walking. Am J Orthod . 1997, 283-287. [ Links ]
11. Solow B, Tallgren A. Dentoalveolar morphology in relation to craneocervical posture. Am J Orthod . 1977; 47 (3): 157-164. [ Links ]
12. Rocabado M. Análisis biomecánico cráneo-cervical a través de una telerradiografía lateral. Rev Chil de Ortodoncia . 1984, pp. 1-11. [ Links ]
13. Solow B, Siersbaek-Nielsen S, Greve E. Airway adequacy, head posture, and craniofacial morphology. Am J Orthod . 1984; 86 (3): 214-223. [ Links ]
14. Achilleos S, Krogstad O, Lyberg T. Surgical mandibular setback and changes in uvuloglossopharyngeal morphology and head posture: a short- and long-term cephalometric study in males. European J Orthod . 2000, 22; 383-94. [ Links ]
15. Achilleos S, Krogstad O, Lyberg T. Surgical mandibular advancement and changes in uvuloglossopharyngeal morphology and head posture: a short- and long- term cephalometric study in males. European J Orthod . 2000; 22: 367-381. [ Links ]
16. Savjani D, Wertheim D, Edler R. Change in cranio-cervical angulation following orthognathic surgery. European J Orthod . 2005; 27: 268-273. [ Links ]
Note This article can be read in its full version in the following page http://www.medigraphic.com/facultadodontologiaunam Mailing address:
Francisco Manuel Sánchez Ramos
Mailing address:
Francisco Manuel Sánchez Ramos
E-mail: drsanchezr@me.com











 texto en
texto en 


