Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista odontológica mexicana
Print version ISSN 1870-199X
Rev. Odont. Mex vol.17 n.3 Ciudad de México Jul./Sep. 2013
Case reports
Maxillary sinus elevation and simultaneous implant placement using PRGF (plasma rich in growth factors), hydroxyapatite and allogenic graft. Seven year case report
Nayibe Hernández Tejeda,* Ma. del Carmen López Buendía§
* Graduate, Periodontics Specialty, Graduate School, National School of Dentistry, National University of Mexico (UNAM).
§ Professor, Periodontics Specialty, Graduate School, National School of Dentistry, National University of Mexico (UNAM).
ABSTRACT
Maxillary sinus floor elevation is a predictable surgical procedure meant to vertically increase the amount of bone in the posterior region of the upper jaw to enable placement of a prosthetic rehabilitation device supported by implants. The aim of the present article was to describe elevation of the maxillary sinus floor using plasma rich in growth factors, absorbable hydroxyapatite and bone allograft as sub-antral graft materials with simultaneous placement of two surface treated implants (Osseotite, 3i). The present article also reported clinical and radiographic results obtained at seven days, six months and seven years after the surgery. From the clinical and radiographic standpoint suitable healing was observed. The surgical procedure used in the present clinical case was considered a suitable option to place implants in atrophic maxillary areas.
Key words: Maxillary sinus elevation, sub-antral graft, dental implants, plasma rich in growth factors.
INTRODUCTION
Bone-integrated oral implants have shown long-term predictable results. The greatest failure rate in implants was found among those placed in the posterior region of the upper jaw. This is due to the anatomical characteristics of the region which include quality and amount of present bone.1 Bone availability in this area is reduced. This is due to several causes, which can include, among others: premature tooth loss causing thus sinus pneumatization, periodontal disease, iatrogenic or physiological bone resorption. All the aforementioned would preclude treatment of prosthetic rehabilitation supported by implants.2
Elevation of the maxillary sinus floor is a surgical procedure which consists on vertically increasing the amount of bone found in that location. This procedure was first designed and described by Hilt Tatum in 1976, at the Dental Implant Meeting held in Birmingham, Alabama. Nevertheless, the first published data on this subject matter were released by Boyne ad James in 1980.3
Elevation of the maxillary sinus is a recommended technique for edentulous areas of the maxillary posterior region lacking adequate bone. In that region, placement of dental implants is required in order to achieve successful prosthetic treatment.4 Different anatomical situations and different topography of the sinus with respect to the maxillary ridge give rise to establishing a classification with respect to the pneumatization and atrophy or resorption of the sub-antral maxillary area. Four grades are identified:
Grade I. The height of the sub-antral maxillary segment is 10 mm or more, thus allowing implant placement without having to elevate the sinus floor.
Grade II. Sub-antral maxillary segment height is lesser than 10 mm and over 8 mm; these cases can be treated with osteotomes.
Grade III. The height of the sub-antral segment is between 4 and 8 mm. In this case it is needed to increase the vertical volume of the bone. This is achieved by surgically elevating the floor of the maxillary sinus through placement of a sub-antral graft as well as implants.
Grade IV. The height of the sub-antral segment is under 4 mm. With these dimensions, obtaining acceptable implant primary stability is very risky. Therefore, a two-stage surgical technique was designed: the first involved elevation of the maxillary sinus and the second entailed implant placement.5
Contraindications to this procedure are: inadequate sinus transversal dimension, ostium location at the surgical site, excessive or inadequate inter-occlusal space, sinus disease, as well as all general contraindications to dental implant placement.6
The first grafting material used in sinus elevation procedure was autologous bone harvested from the iliac crest.7 Commonly used donor sites within the mouth are: maxillary tuberosity, mandibular retromolar area as well as mandibular ramus. Additionaly to auto-grafts, allografts, xenografts, alloplastic grafts or combinations of these have been used. Varied results of these techniques have been reported at the consensus of the 1996 Conference.4
Plasma rich in platelets (PRP) is an autologous human platelet (above normal) concentrate. It is considered a source rich in growth factors. It was introduced in 1998 by Marx et al. Combined with an autologous bone graft, it was used to reconstruct mandibular defects. Their research showed that PRP addition to bone grafts accelerated the rate of bone maturation, and radiographically increased bone density when compared to bone graft by itself.8 Since that point in time, it has been used in different clinical procedures such as, among others, sinus floor elevation, ridge increase, periodontal defect treatments, alveolus preservation.9
At a later point, plasma rich in growth factors (PRGF) would emerge. This technique was proposed by Eduardo Anitua, and several studies informed of their use as an additional option within the scope of several materials to achieve a sub-antral graft. This technique purported the aim of compacting particulate grafts and improving conditions for bone regeneration.10-12
The aim of the present research paper was to describe this technique and report clinical and radiographic results achieved in a patient after having conducted the surgical procedure entailing elevation of the maxillary sinus floor mucosa and simultaneous implant placement, with usage of PRGF, absorbable HA as well as FDBA as sub-antral bone graft.
CASE REPORT
43 year old female patient attended the Graduate School, National School of Dentistry, National University of Mexico (UNAM) seeking periodontal treatment. The patient exhibited good general health and had been diagnosed with moderate generalized chronic periodontitis.
Initial periodontal therapy was undertaken: it entailed personal control of oral hygiene, scaling and root planning as well as consultation with Oral Prosthesis Department to launch a comprehensive treatment.
Teeth 16 and 17 were deemed hopeless. Therefore, surgical phase consisted on extractions with alveolus preservation by placing 0.5 g of allograft (DFDBA) and using a collagen membrane. Tooth 15 was missing.
Teeth 44 and 45, 24, 25 and 27 were subjected to debridement surgery. Teeth 36 and 37 were subjected to regenerative periodontal surgery (Enamel-Derived Protein Matrix).
Eleven months after performing alveolus preservation surgery in the upper right posterior area, bone amount was radiographically and clinically assessed. According to the aforementioned classification presence of Grade III residual bone was established. Therefore, maxillary sinus elevation was programmed with simultaneous placement of two implants. Sub-antral graft was composed by Plasma Rich in Growth Factors (PRGF), absorbable hydroxyapatite (absorbable HA, Osteogen®) as well as mineralized lyophilized bone allograft MLBAG.
Before undertaking surgical procedure, and according to PRGF protocol established by Anitua in 1966, 30 cm3 of the patient's blood were obtained.10 Sterile tubes with 3.8% sodium citrate were used as anticoagulant. Blood was centrifuged for seven minutes at 1,700 rpm. After this, plasma was separated into fractions by means of meticulous pipetting to avoid creation or turbulence in obtained fractions. The first 500 µL (0.5 cm3, fraction 1) was a platelet-poor plasma, it was consequently poor in growth factors. The next 500 µL (fraction 2) corresponded to plasma containing similar number of platelets to those found in peripheral blood. Finally, the plasma fraction richest in growth factors was the 500 µL fraction, found to be immediately above the red series (fraction 3). 1 cm3 of PRGF was found to every 4.5 cm3 tube. Total was 6 cm3 which were then activated with 10% calcium chloride (50 µL per each PRGF cm3) as activator and platelet aggregation means. Obtained PRGF was combined with bone graft materials, 1 g of mineralized bone allograft (Pacific Coast Tissue Bank®) and 1 g of absorbable hydroxyapatite (Osteogen®).
Ad interim, at the surgical site, after having administered local anesthesia, a liberating mesial incision was performed on the alveolar ridge in order to gain improved surgical field visibility, lifting thus a full-thickness graft.
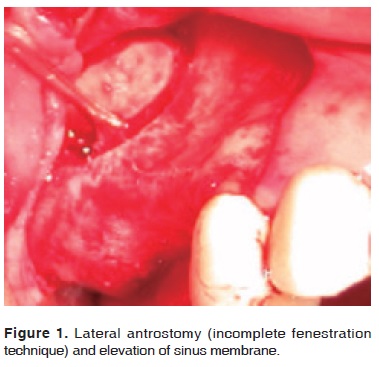
An antrostomy was performed following the technique described by Tatum, known as incomplete fenestration technique, in which approach is traced on the maxillary external or lateral side according to topographic projections of the radiographic study as well as sinus intra-oral transillumination.7 This type of osteotomy, due to the elevation of the bone segment, allows the transformation of a new maxillary sinus floor. To this effect a low speed, number six, ball-shaped, carbide burr was used.
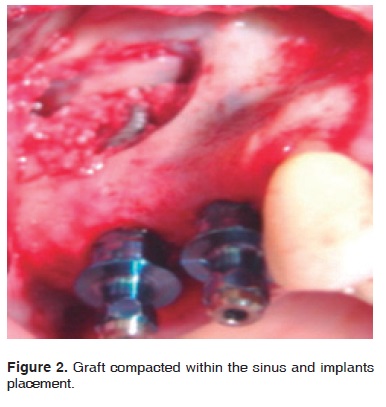
Once the access was elevated, the sinus membrane was detached (Schneider membrane) with specific curettes (Figure 1). The next step, with the assistance of the surgical guide, was to prepare the bed wherein to place the implants. Two 4 x 15 mm Osseotite 3® were used.
The graft was placed into the sinus cavity following a two-stage technique. The first stage involved placing the graft before the implants, so as to be able to reach the medial wall and thus easily compact the graft material. The remaining graft was placed after situating the implants in their final position (Figure 2).
Using the plasma's fraction 2, a fibrin clot was formed to be placed as biological membrane on the maxillary lateral wall and thus achieve sinus cavity sealing (Figure 3). The consistency of the membrane was achieved after placing this plasma fraction in a tube containing calcium chloride. This procedure was similar to that used when using the fraction rich in growth factors, with the difference that in this case, a thermal block was used to accelerate clotting, which took approximately 15 minutes.

The flap was repositioned and secured with horizontal mattress sutures as well as simple sutures, using 3-0 silk. Finally, the surgical site was dampened with the fraction of plasma poor in growth factors (fraction 1) so as to improve and accelerate epithelialization process in the area.
The patient was thoroughly informed on postoperative care to be observed. Antibiotic coverage was achieved with amoxicillin, 750 mg every 12 hours for seven days. Ibuprofen was equally prescribed to control pain and inflammation. 0.12% chlorhexidrine gluconate, 15 mL twice a day for two weeks was used as local antiseptic.
RESULTS
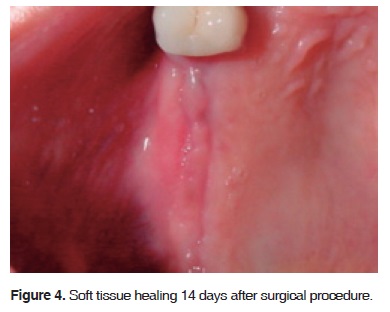
Obtained results were assessed at the time when sutures were removed, that is, seven days after surgery. Suitable soft tissue healing was observed. 14 days after surgery, the wound epithelialization was completed (Figure 4). No implant exposition was observed. The patient reported little post-operative discomfort.
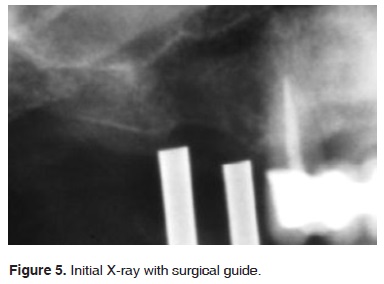
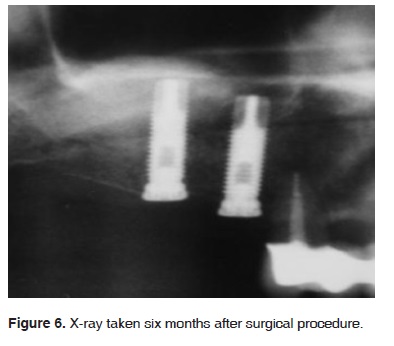
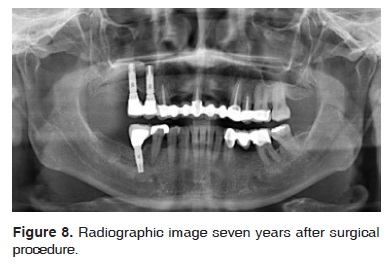
Six months after surgery results were deemed favorable (Figures 5 and 6). Radiographically, the area of the sub-antral graft appeared dense and compact, lacking radiolucent areas or bone sequestrations. The implants were uncovered ten months after surgical procedure Two months later prosthetic rehabilitation was undertaken. Presently, seven years after the sinus elevation surgical procedure, upon clinical assessment, the implants appear stable, without radiographic changes at the level of the bone crest (Figures 7 and 8).

DISCUSSION
Maxillary sinus elevation with sub-antral graft is a surgical procedure currently considered one of the most common and accepted methods to increase bone volume in the posterior lower jaw area in order to place implants. Reports in scientific literature show high success rates when using this technique. This technique is a safe, effective and predictable procedure.13
In some cases, guided bone regeneration (GBR) procedures can be undertaken to increase vertical ridge height, whenever the inter-occlusal space might allow it. GBR and maxillary sinus elevation technique can even be combined in cases of very severe bone loss in the region.
On the other hand, use of short implants in the posterior upper region can solve the problem. Nevertheless, this can result in a poor diagnosis, in cases of low bone density, as is often the case in that anatomical region.14 Due to the aforementioned reasons, use of implants exhibiting suitable length and diameter might require elevation of the sinus membrane and placement of a sub-antral graft.15
Suitable treatment plan, step-by step observance of one or two-stage surgical protocol, appropriate selection of sub-antral graft as well as proper medication and pre- and postoperative care are some of the factors essential for achievement of successful long and short term results of this procedure.16
For this technique, there are many surgical protocols as well as modifications.17 Nevertheless, when sinus elevation is conducted simultaneously to implant placement (one stage) there is a great advantage with respect to total restoration time, although it is important to achieve primary stability of the implant. This implies having appropriate amounts of remaining bone, if this were not to be the case failure rates would increase.
Increase of dental implants use and therefore, the need to improve bone conditions for successful placement, has driven clinicians in the search of better alternatives in the field of bone implants. There is wide variety of materials used for sub-antral bone grafts. To this day, the best option still is autologous bone, since, it not only provides osteoblastic cells, it also confers osteo-induction and osteo-conduction, offering organic and inorganic matrixes and viable bone cells, without incurring in antigenicity risks. Nevertheless, obtaining autologous grafts from extraoral donor sites involves longer recovery time, the need for general anesthesia and hospitalization of the patient, besides higher treatment cost. Reports indicate that intraoral sites yield suitable results, nevertheless, limitations in availability of donor sites constitutes a disadvantage, as well as increased procedure time, morbidity of another surgical site and increased patient discomfort. The amount of bone harvested intra-orally is generally insufficient for a complete increase of bilateral maxillary sinus floor.18,19
Therefore, many authors support the use of materials obtained from other sourcces (allografts, auto-grafts xeno-grafts and alloplastic) in combination with autologous bone. They further argue that with these techniques a more suitable resorption time is generated. Choice of one or more materials often depends on the amount of requered bone.4,13,16,20-22
Plasma rich in growth factors is one of the materials developed with the purpose of improving graft handling. This material improves soft tissue healing.10 Incorporation of this technique can bring benefits for the patient without incurring in any risk of spread or disease transmission. PRGF use entails no secondary effect. Use of PRGF allows simplification of the subantral graft compaction technique. Allowing thus to improve consistency and facilitating handling as well as increasing the amount of graft. Recent studies results have shown that PRGF as well as PRP (plasma rich in platelets) do not provide significant differences in the procedures' final results.23,24
With respect to the implants' inherent characteristics, it has been well established that there is greater survival rate whenever implants placed within the maxillary sinus come from a treated surface.13
Knowledge of complications which can arise as a result of a sinus elevation procedure such as membrane perforation or maxillary sinus infection will help us to avoid them, or, in case they were to occur, to then properly treat them.
It is important to take into consideration the fact that this surgical procedure requires a thorough treatment plan as well as a knowledgeable, skillful and experienced surgeon.25,26
CONCLUSIONS
In the present clinical case and based upon clinical and radiographic results obtained seven years after completing the surgical procedure, we could conclude that elevation of maxillary sinus using as sub-antral graft a combination of PRGF, absorbable HA and allograft with a simultaneous placement of dental implants provided good results. This procedure decreased as well total treatment time for the patient, and proved to be a predictable and effective procedure, in cases where a thorough treatment plan had been previously designed.
REFERENCES
1. Albrektsson T, Dahl E, Enbom L, Engevall S, Engquist B, Erikksson AR et al. Osseointegrated oral implants. A Swedish multicenter study of 8,139 consecutively inserted implants. Journal of Periodontology. 1988; 59: 287-296. [ Links ]
2. Bruggenkate C, Bergh J. Maxillary sinus floor elevation: a valuable pre-prosthetic procedure. Periodontology. 2000; 1998; 17: 176-182. [ Links ]
3. Boyne P, James R. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surgery. 1980; 38: 613-616. [ Links ]
4. Jensen O, Shulman L, Block M, Iacono V. Report of the sinus consensus conference of 1996. Int J of Oral and Maxillofacial Implants. 1998; 13: 11-55. [ Links ]
5. Salagaray V, Lozada J. Técnica de elevación sinusal. Unidad de Implantología Oral y Prótesis Biointegrada. España, 1993. [ Links ]
6. Baladrón J, Colmenero C, Elizondo J. Cirugía avanzada en implantes. Ed. Ergon. España 2000. [ Links ]
7. Tatum H. Maxillary and sinus implant reconstruction. Dent Clin North Am. 1986; 30: 227-229. [ Links ]
8. Marx R, Carlson E, Eichstaedt R. Platelet-rich plasma. Growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol. 1998; 85: 638-646. [ Links ]
9. Marx R. Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg. 2004; 62: 489-496. [ Links ]
10. Anitua E. Un nuevo enfoque en la regeneración ósea. PRFC. España: Puesta al día publicaciones; 2000. [ Links ]
11. Anitua E. Plasma rich in growth factors: preliminary results of use in the preparation of future sites of implants. Int J Oral and Maxillofacial Implants. 1999; 4: 529-535. [ Links ]
12. Anitua E. La utilización de los factores de crecimiento plasmáticos en cirugía oral, maxilofacial y periodoncia. Revista del Ilustre Consejo General de Colegios de Odontólogos y Estomatólogos de España. 2001; 3: 305-315. [ Links ]
13. Wallace S, Froum S. Effect of maxillary sinus augmentation on the survival of endosseous dental implants. A systematic review. Annals of Periodontology. 2003; 8: 328-343. [ Links ]
14. van den Bergh J et al. Anatomical aspects of sinus floor elevations. Clin Oral Impl Res. 2000; 11: 256-265. [ Links ]
15. Yamamichi N, Itose T, Neiva R, Wang H. Long-term evaluation of implant survival in augmented sinuses: a case series. Int J Periodontics Restorative Dent. 2008; 28: 163-169. [ Links ]
16. Del Fabbro M, Testori T, Francetti L, Weinstein R. Sistematic review of survival rates for implants placed in the grafted maxillary sinus. Int J Periodontics Restorative Dent. 2004; 24: 565-577. [ Links ]
17. Smiler D. The sinus lift graft: basic technique and variations. PP & AD. 1997; 9 (8): 885-893. [ Links ]
18. Mellonig J. Autogenous and allogenic bone grafts in periodontal therapy. Critical Reviews in Oral Biology and Medicine. 1992; 3 (4): 333-352. [ Links ]
19. Lang N, Karring T. Proceedings of the 3rd European Workshop on Periodontology Implant Dentistry. Ed. Quintessence Books; Switzerland. 1999; 535-543. [ Links ]
20. Kassolis J, Rosen P, Reynolds M. Alveolar ridge and sinus augmentation utilizing platelet-rich plasma in combination with freeze-dried bone allograft: case series. J Periodontol. 2000; 71: 1654-1661. [ Links ]
21. Jensen O. The sinus bone graft. Second Ed. Quintessence Books. 2006. [ Links ]
22. Gonshor A. Technique for producing platelet-rich plasma and concentrate: background and process. Int J Periodontics Restorative Dent. 2002; 22: 547-557. [ Links ]
23. Plachokova A, Nikolidakis D, Mulder J, Jansen J, Creugers N. Effect of platelet-rich plasma on bone regeneration in dentistry: a systematic review. Clin Oral Impl Res. 2008; 19: 539-545. [ Links ]
24. Torres et al. Effect of platelet-rich plasma on sinus lifting: a randomized-controlled clinical trial. J Clin Periodontol. 2009; 36: 677-687. [ Links ]
25. Kan J et al. Factors affecting the survival of implants placed in grafted maxillary sinuses: a clinical report. J Prosthet Dent. 2002; 87: 485-489. [ Links ]
26. Pjetursson B, Ching Tan W, Zwahlen M, Lang N. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. J Clin Periodontol. 2008; 35 (Suppl. 8): 216-240. [ Links ]
Note This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam Mailing address:
Mailing address:
Nayibe Hernández Tejeda
E-mail: nayiht@hotmail.com











 text in
text in 


