Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista odontológica mexicana
versión impresa ISSN 1870-199X
Rev. Odont. Mex vol.17 no.2 Ciudad de México abr./jun. 2013
Case report
Guided surgery in implantology practice
Iván Contreras Molina,* Gildardo Contreras Molina,§ Leonardo Bez,II Ricardo de Souza Magini,¶ Claudia Ángela Maziero Volpato**
* Masters student, Implantology-Dentistry, Universidad Federal de Santa Catarina.
§ Endodontic Professor Universidad Michoacana de San Nicolás Hidalgo, Morelia, México.
II Implantology-Dentsitry Master's Degree, Universidad Federal de Santa Catarina.
¶ Associate at Dentistry Department, Universidad Federal de Santa Catarina, Master and PhD Bauru School of Dentistry.
** Attached Professor, Partial Prosthesis Department, Operative Dentistry PhD, Dentistry-Implantology Masters Degree, Universidad Federal de Santa Catarina.
ABSTRACT
In the field of implantology, surgical procedures have been performed with the assistance of computerized tomographies associated to the CAD/CAM technology. Digital images thus obtained, allow professionals to perform virtual surgical planning in specific software. This results in a prototyped guide which enables surgical procedures to be achieved in lesser clinical time, without flaps or sutures, yielding excellent post-operative results. The aim of the present article was to present the sequence of a clinical case in which implants were placed using guided surgery.
Key words: Dental implants, prostheses, guided surgery.
INTRODUCTION
Guided surgical techniques based on classical predictability techniques have been widely used in the field of implantology with the aim of reducing surgical morbidity as well as offering the patient a less invasive surgical/prosthetic treatment.1-4
In 2002, Van Steenberghe et al suggested a guided surgery protocol which advocated planning based on data provided by a computerized tomography associated to tridimensional software. Transference from virtual planning into operative field was conducted following rigid guides obtained through rapid prototype processes. In this technology, liquid polymer is injected and laser-cured according to tomography data.1
Presently, computerized tomography as well as specialized software (Nobel Guide, Simplant, BTI Scan II, Implant Viewer, Dental Slice) have allowed virtual surgical/prosthetic planning based upon accurate tridimensional bone visualization and its relationship with the future prosthesis. When conducting virtual planning, it is possible to a) assess and measure bone density, b) select type, size and number of implants, c) determine implant location, inclination and depth level with respect to the bone, d) evaluate the possibility of implant bicorticalization) analyze intermediary characteristics as well as the emergence of the fixation screw of the future prosthesis and f) appraise proper positioning of rings in the surgical guide and ideal location of fixation pins or screws, responsible for the stability of the guide within the mouth during surgical procedure.5,6
When compared to conventional techniques, guided surgery provides multiple benefits for the patient as well as for the clinician. The post-operative prospect of a guided surgery procedure is excellent. It involves a minimally invasive process, devoid of surgical flaps or sutures; it also decreases pain and post-operative edema in the patient.7,8
In spite of being costlier and requiring more precise and detailed planning, the presence of a prototyped surgical guide helps to protect critical anatomical structures, simplifies clinical procedures and reduces surgical and prosthetic time.9-12 Nevertheless, to warrant guided surgery, case selection and preparation are essential.2 The patient must exhibit appropriate oral opening, sufficient amount of keratinized mucosa and adequate bone availability in height and thickness.13,14
The purpose of the present article was to present a clinical case where the main treatment option was manufacturing a guided surgery for implant placement in an edentulous mandible (lower jaw).
DESCRIPTION OF CLINICAL CASE
70 year old female patient, wearing conventional full upper and lower prostheses. Following classical techniques and concepts a new set of full dentures was manufactured, with the purpose of re-establishing maxillary-mandibular relationship, lips harmonious positioning and support. Once patient and operator were in agreement, the upper prosthesis was polymerized following the conventional system. Waxing of the lower prosthesis was replicated in transparent (clear) resin so as to obtain a tomographic guide. This guide received radio-opaque, gutta-percha markers, in the gingival, vestibular area, to serve as reference points to align tomographic images.
Manufacture of tomographic guide is an essential aspect for the success of the guided surgery. It is responsible for references transfer of the prosthesis, neighboring teeth and fiber-mucosa to the software. At a later point, based on this data, virtual surgical planning was conducted. It can then be suggested that classical stages of functional impression, working model manufacture and basal area effective waxing are essential to ensure tomographic guide precision.
The guide was tested within the mouth, to assess adaptation and occlusal stability (Figure 1). After this, a heavy silicon inter-occlusal record was manufactured to preserve the guide in proper position during the time of tomographic exam. This maneuver was important to preserve the guide's internal area properly supported in the basal area, in close contact with the mucosa, so that tomographic images showing relationship of guide with the ridge be as realistic as possible. Guide adaptation was confirmed by the uniform ischemic aspect established with the mucosa when the patient occluded upon the record.

During tomographic examination, shots were taken with the guide in position as well as with the guide outside of the mouth. Obtained images were exported to a 3D file, allowing thus manipulation in interactive navigation software (Dental Slice, Bioparts, Brazil). Due to double scanning, images can be visualized either individually or superposed, allowing thus to analyze existing relationship between bone structure and guide.
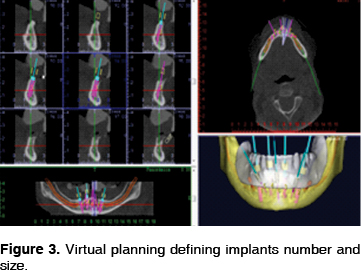
Virtual planning was undertaken after obtaining tomographic images. Implants were tri-dimensionally located according to prosthesis and bone anatomy. Implant depth, inclination and position were determined. When using 3D tools spatial perspective (view) was possible. 2D tools offer anatomical cuts (sections) where measurements were performed for the appropriate selection of implant, pin and fixation screws sizes (Figures 2 and 3).

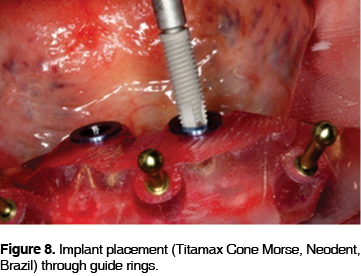
Virtual planning was sent to a manufacturing central; surgical guide was prototyped through a stereolythographic process (Bioparts, Brazil). This guide contains cylindrical projections where metal rings are inserted. They correspond to areas where implants will be placed. The surgeon will locate implant burrs and assemblers at the center of these rings.
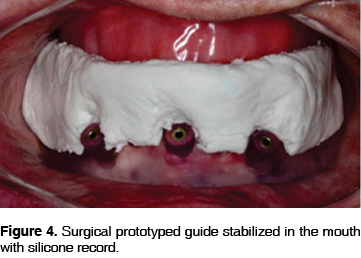
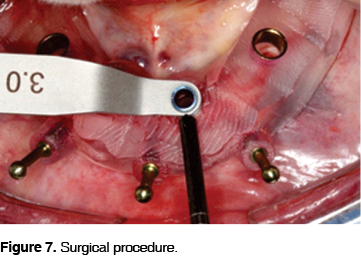
During surgical event, the silicon record formerly used to preserve the surgical guide in position is once more put into position with the aim of maintaining the guide in position for the placement of fixation pins (Figure 4). Three perforations were performed to install the pins (Figures 5 and 6). In a guided surgery, it is important for the guide not to move during clinical procedure. To install implants, all surgical instruments (burrs) must be used sequentially according to established surgical procedures (Figures 7 and 8). No surgical flap was raised, burrs perforated the mucosa, avoiding thus post-operative sutures. Four implants (Titamax Cone Morse, Neodent, Brazil) were placed in the edentulous lower jaw. Following implant installation, they were locked with 60N torque to receive prosthesis with immediate load protocol. Intermediaries were placed over positioned implants (Conical mini abutment, Neodent, Brazil) (Figure 9).



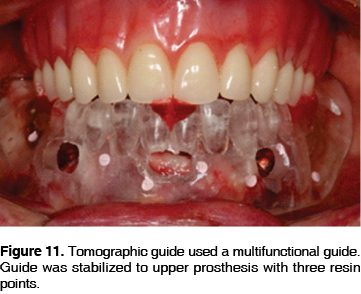
After this procedure, the tomographic guide, previously opened at its lingual region and with windows in the vestibular region, was used a multi-functional guide to impress the operated area and record maxillary-mandibular relationship.
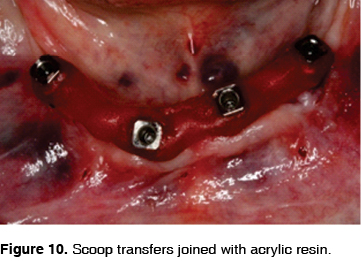
Open spoon impression transfers were screwed (short screws) on the intermediaries and joined together with acrylic resin (Patter Resin CG, USA) (Figure 10). The multifunctional guide was once more tested in order to analyze the presence of space for the impression material.
Three acrylic resin points (Pattern Resin, CG, USA) were created on the guide's occlusal surface (two posterior, one anterior) with the purpose of recording maxillary-mandibular relationship (Figure 11). With the patient in occlusion, the guide was adjusted to the transfers with acrylic resin. After this, impression was achieved with fluid addition silicon injected within vestibular windows of the lingual opening. Once the material was included into the impression, transfers were unscrewed and removed (Figure 12).

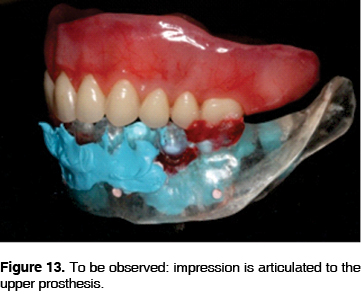
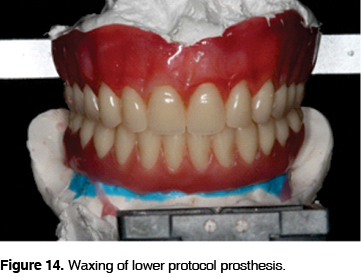
All laboratory stages were observed in traditional manner (Figures 13 and 14). At the clinical session, bar as well as mounted teeth were tested. After confirming the bar clinical and radiographic seating, balanced occlusion and facial harmony were assessed, to then direct the prosthesis for final polymerization. After a few hours, the prosthesis was installed upon the intermediaries with a new set of fixation screws (Figures 15 and 16).
DISCUSSION
Even though traditional protocol for bone-integrated implant placement establishes a two-stage surgical procedure,14 increasing numbers of clinicians and patients are seeking less invasive treatments yielding faster results, thus, security and mastery of immediate load surgical techniques would enable achievement of guided surgeries.4,6,8,11-13 In a similar fashion, tomographic examinations and specialized software give rise to proper surgical/prosthetic planning as well as surgical precision and guaranteeing tridimensional visualization of implants.1-3,5
In cases when patients exhibit adequate oral opening and there is sufficient amount of keratinized mucosa as well as bone availability, the possibility of successfully using this technique increases. Prototyped guides are adjuvant to performing simpler and faster surgical procedures, without prejudice to classic clinical results. In cases of excessive bone atrophy, conventional surgical technique is generally the best option to visualize surgical areas.6,11
Another factor to consider is the careful preparation of the tomographic guide, as well as virtual planning. Small alterations in guide positioning could elicit severe surgical compromises.5 Inadequate image, incorrect software navigation and human error are the main factors which can compromise the guided surgery success.3
Guided surgery planning allows monitoring of relationships between implant axis and positioning of the manufactured tooth, thus avoiding unforeseen use of angulated intermediaries used to compensate for future unfavorable inclination of the implants.12 Nevertheless, there are limitations when handling soft and hard tissues simultaneously to installing implants or incorporating biomaterials during the surgical event. Another critical situation when using implant placement techniques in guided surgeries is the intervention in subjects presenting high smile line, which could render the alveolar ridge visible. If this were the case, it would be necessary to perform an osteotomy to transfer the prosthesis transition area between mucosa and gums.10
CONCLUSION
Determination of anatomical structures real spatial position decreases surgical risks helps planning and execution of simpler faster surgeries prone to lesser surgical morbidity. When compared to traditional techniques placement of implants with guided techniques require substantially greater financial investment and effort. Nevertheless, guided technique favors excellent clinical results since it eliminates errors and allows systematizing treatment reproduction granting thus success and longevity.
REFERENCES
1. van Steenberghe D, Naert I, Andersson M, Brajnovic I, Van Cleynenbreugel J, Suetens P. A custom template and definitive prosthesis allowing immediate implant in the maxilla: a clinical report. Int J of Oral Maxillofac Implants 2002; 17: 663-667. [ Links ]
2. Di Giacomo GA, Cury PR, de Araújo NS, Sendyk WR, Sendyk CL. Clinical application of stereolithographic surgical guides for implant placement: preliminary results. Journal of Periodontology 2005; 76: 503-507. [ Links ]
3. Widmann G, Bale RJ. Accuracy in computer-aided implant surgery. A review. Int J Oral Maxillofac Implants 2006; 21:305-13. [ Links ]
4. Ersoy AE, Turkyilmaz I, Ozan O, McGlumphy EA. Reliability of implant placement with stereolithographic surgical guides generated from computed tomography: clinical data from 94 implants. Journal of Periodontology 2008; 79: 1339-1345. [ Links ]
5. Brief J, Edinger D, Hassfeld S, Eggers G. Accuracy of image-guided implantology. Clinical Oral Implants Research 2005; 16: 495-501. [ Links ]
6. Schneider D, Marquardt P, Zwahlen M, Jung RE. A systematic review on the accuracy and the clinical outcome of computer-guided template-based implant dentistry. Clinical Oral Implants Research 2009; 20: 73-86. [ Links ]
7. Rosenfeld AL, Mandelaris GA, Tardieu PB. Prosthetically directed implant placement using computer software to ensure precise placement and predictable prosthetic outcomes. Part 1: diagnostics, imagining and collaborative accountability. Int J Periodontics Restorative Dent 2006; 26: 214-221. [ Links ]
8. Nikzad S, Azari A. A novel stereolithographic surgical guide template for planning treatment involving a mandibular dental implant. J Oral Maxillofac Surg 2008; 66: 1446-1454. [ Links ]
9. Ewers R, Schicho K, Truppe M, Reichwein A, Figl M, Wagner A. Computer-aided navigation in dental implantology: 7 years of clinical experience. J Oral Maxillofac Surg 2004; 62: 329-334. [ Links ]
10. Balshi SF, Wolfinger GJ, Balshi TJ. Surgical planning and prosthesis construction using computed tomography, CAD/CAM technology and the internet from immediate loading of dental implants. J Esthet Restor Dent 2006; 18: 312-323. [ Links ]
11. Jabero M, Sarment DP. Advanced surgical guidance technology: a review. Implant Dent 2006; 15 (2): 135-142. [ Links ]
12. Assche NV, Quirynen M. Tolerance within a surgical guide. Clinical Oral Implants Research 2010; 21: 455-458. [ Links ]
13. Jung RE, Schneider D, Ganeles J, Wismeijer D, Zwahlen M, Hämmerle CH et al. Computer technology applications in surgical implant dentistry: a systematic review. Int J Oral Maxillofac Implants 2009; 24: 92-109. [ Links ]
14. Holst S, Blatz MB, Wichmann M, Eitner S. Clinical application of surgery fixation screws in implants prosthodontics. Part III. Indexing implant position. The Journal of Prosthetic Dentistry 2004; 92: 496-499. [ Links ]
Note  Mailing address:
Mailing address:
Iván Contreras Molina
E-mail: dr.ivancontreras@gmail.com
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam











 texto en
texto en 


