Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista odontológica mexicana
versión impresa ISSN 1870-199X
Rev. Odont. Mex vol.17 no.2 Ciudad de México abr./jun. 2013
Case report
Oral rehabilitation under general anesthesia of pediatric patient with diagnosis of epidermolysis bullosa. Clinical case report
Elizabeth Xóchitl García Cruz,* Eduardo de la Teja Ángeles,§ Luis Américo Durán GutiérrezII
* Student, Pediatric Stomatology Service, Instituto Nacional de Pediatría (National Pediatrics Institute), Mexico City.
§ Head of Pediatric Stomatology Service, Professor, Instituto Nacional de Pediatría (National Pediatrics Institute), Mexico City.
II Pediatrician and stomatologist, attached to the Pediatrics Stomatology Service, Instituto Nacional de Pediatría (National Pediatrics Institute), Mexico City.
ABSTRACT
Epidermolysis bullosa encompasses a group of infrequent skin diseases characterized by the appearance of ulcers and blisters after an event of minor trauma of tangential minimal pressure. This study presents the case of a child treated at the Instituto Nacional de Pediatría (National Pediatrics Institute). The patient was subjected to oral rehabilitation under general anesthesia. A specially tailored team participated; they used devices such as cotton based adhesives and gauze dressings to place vital signs monitors, as well as oil emollients on soft tissues. All the aforementioned items were used with the main objective of avoiding ulcers, blisters or bullae formation. For this group of patients, specific handling of the oral cavity as well as tissues within and around the mouth is required. Tailor made preventive programs must also be designed.
Key words: Epidermolysis bullosa, bullae, difficulties in care, prevention.
INTRODUCTION
Epidermolysis bullosa (EB) is a group of recessive or dominant autosomal hereditary (genetic) diseases, characterized by bullae formation. Bullae are associated to numerous defects, including anomalies in the chemical structure of keratin, hemidesmosomes, fibrils, filaments and physio-chemical components of the skin collagen. EB affects 1:50,000 live births.1,2
Dominant autosomal form is the most severe. It is characterized by bullae formation in skin and mucosa which produce severe scarring and contractures. As a result the following could result: tongue atrophy, microstomy and in some cases ankyloglossia. Normal feeding patterns can cause severe ulcerations in mouth and pharynx. As a consequence, these children frequently suffer nutritional restrictions. In these cases, gastrostomy at an early age is frequent.3
CLASSIFICATION
Based on clinical, genetic and histopathological characteristics assessed with electron microscope, histochemical analysis or molecular study of involved proteins, several types of EB have been identified .The use of electron microscope enables EB classification into three main groups: simple EB, dystrophic EB and union EB. EB subtypes are based on phenotype, structural characteristics and membrane antigen expression. Present studies on molecular genetics have shown a variety of defects in different types of EB.3,4
In the simple form, separation takes place caused by fractures due to mutations in citokeratin 5 and 14 filaments located in the lower portion of the epidermis basal keratinocytes. Due to lamina 5 mutations the blister is placed in the lucid lamina of the epidermoid basal membrane.
Dystrophic forms are caused by type VII collagen mutations. This collagen forms anchorage fibrils of the sublamina densa.
At birth, it is impossible to differentiate the epidermiolysis subtype, since all three forms present the same characteristics.4-6
CLINICAL MANIFESTATIONS
Cinical characteristics vary considerably and they can include scarring, erosions, milia, vesicles, granulation tissue, pigmentations, cicatricial alopecia as well as nail absence or atrophy. Skin characteristics can include: eyes, teeth, oral mucosa, esophagus, gastro-intestinal tract, anus, genitor-urinary tract as well as skeletal muscle system. In general terms, EB specific subtypes can present a combination of cutaneous and extra-cutaneous characteristics.6, 7
Dystrophic epidermiolysis. It can have dominant or recessive autosomal heritage. Bullous lesions are present between the lamina densa and the dermal layer of the skin, therefore, the separation is sub-dermal, taking place under the basal structure, due to breakage of anchoring fibers. This elicits changes in type VII collagen. It represents one of the most severe clinical presentations. Scarring can be observed in the skin, and mucosa, vesicles and scarring can be observed in the esophagus, sometimes causing secondary stenosis. Blisters found in skin and mucosa can elicit retraction of palm and sole skin of hands and feet. This case is known as pseudo-syndactyly, and is caused by repeated bloody ulcers and vesicles occurring in hands and feet.
In dystrophic EB patients scars, it is frequent to find spino-cellular carcinoma lesions. This elicits a fatal outcome (Table I).5
TREATMENT
EB compromises multiple organs and systems. Its treatment requires a multi-disciplinary team. The team should include pediatricians, dermatologists, nurses, nutritionists, geneticists, orthopedic surgeons, plastic surgeons, stomatological pediatricians, etc.
Treatment consists on palliative care, through the use of topic creams (salves) moisturizers, topical antibiotics, nutritional supplements with iron and zinc, especially for anemic children, as well as preparation of liquids with high content of protein and calories, which will help to improve the child's development. Surgical intervention helps correct finger deformities as well as esophageal stenosis. The final objective to achieve in this treatment is to help the patient attain quality of life, bearing in mind that this condition does not count with healing treatment, only treatment of symptoms.1,7
STOMATOLOGICAL CHARACTERISTICS
Clinical characteristics vary in accordance to the EB type. In half the EB forms, there are oral lesions, such as vesicles, which can disappear rapidly leaving no scars. In more severe cases, there is presence of ulcers, microstomy, and obliteration of the oral vestibules as well as ankyloglossia. In dystrophic EB cases, it is frequent to find squamous cell carcinoma in the tongue.
Depending on the EB subtype, other manifestations can be frequently observed. Such is the case of union epidermolysis, where enamel hypoplasia and rampant caries can be observed. Rampant caries can be associated to the prolonged retention of food matter in the oral cavity and to changes in saliva quality and quantity.8
A comparative study conducted on microflora exhibited by a group of dystrophic EB and a control group revealed absence of important changes. The same study, nevertheless, disclosed increase in caries prevalence which could be associated to difficulties encountered by the patient in performing suitable oral hygiene. In these cases, to facilitate hygiene, use of fluoride supplements and 0.2% chlorhexidine rinses were recommended.9,10
A comparative study on dental maturation in EB children conducted by Dr Kosara mentions a variation from 2 years and eight months to 3 years with respect to the control group; this fact led him to conclude that EB children present dental maturation and growth delays.10-12
STOMATOLOGICAL HANDLING
Handling of restorations and dental extractions generally follow a variety of anesthesia protocols, mainly directed to avoid trauma to the skin and oral mucosa. Clear and guided questions must be answered with respect to the disease subtype, its complications, the patients nutritional status, presence of infections, microstomy or vestibule obliteration, state of esophageal structures, etc. Anesthesia management follows several parameters according to the manual Guidelines for Anesthetic Management of Epidermiolysis Bullosa published by Stanford University.12-14
GENERAL MANAGEMENT PRINCIPLES
Avoidance of excessive pressure to the skin. To achieve this goal it is suggested to use special equipment, containing adhesives based on natural cotton, which allow soft removal (Webrill ®), elastic wristbands with Velcro adhesive ( Ace Wrap ®), latex-free micropore (Koban ® tape), Lubriderm ® , nylon and/or cotton elastic bands (Sur-o-flex ®) as well as adhesive electrodes.
Before the procedure, the skin is covered with cotton or gauze dressings to prepare for adhesives placement. It is recommended to lubricate with oleic emollients such as vaseline the anesthetist's specific instruments, such as the laryngoscope, oxygen mask, and intubation probes.
Electrodes coated with a soft adhesive band must be used to monitor signs. The oximeter should be placed in the palm before placing an elastic wristband with velcro adhesives. Oximeters with a clip can also be used.15-19
CLINICAL CASE
3 year old male patient with dystrophic type epidermolysis bullosa was referred to the pediatric stomalogical service of the National Pediatrics Institute to receive treatment for multiple caries. The patient's condition initiated at birth, presenting vesicular-bullous lesions on the proximal third of the right leg. The lesions presented a reddish fluid and left scars. At a later point, the patient presented vesicular-bullous lesions in hands, fingers, and oral cavity. Based on these facts, diagnosis emitted was dystrophic type EB.
Genetic and family history revealed it to be a single, isolated case in the family. Physical examination revealed multiple lesions in the legs as well as scars in the right leg.
Oral examination revealed full primary dentition, caries affecting dentin and enamel, secondary to prolonged usage of feeding bottle and to difficulties to perform suitable oral hygiene as well as carbohydrate-rich soft diet.
Extra-orally, limited oral opening was observed, secondary to presence of microstom (obliteration of the oral vestibule) as consequence of old scars.
Intra-orally, great amounts of bacterial plaque were observed and localized gingivitis at the attached gingiva of front upper teeth.
Due to the extension of caries, to the age of the patient and difficulties in behavior management, oral rehabilitation under general anesthesia was programmed.
INTRA-OPERATIVE PERIOD
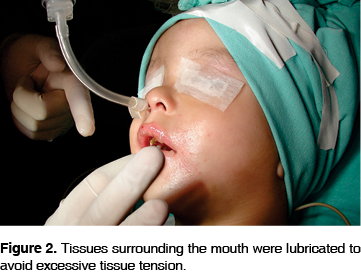
Nitrous oxide was used as inductor. The rim of the mask had previously been coated with Vaseline to avoid exerting pressure on the skin.
Vaseline was equally used to place electrodes, so as to facilitate removal. Micropore tape was used to fixate. Duo-Derm® patches were used to fixate the peripheral route; the patient was placed on a cotton base (under his body); eyes were protected with vaseline and micropore tape.
Naso-tracheal intubation was fixated on a base covered with gauze and adhesive tape. To handle the oral cavity, vaseline was applied to the mouth corners (Figures 1, 2 and 3).


The second molar had not fully erupted, therefore, it was decided to work without absolute isolation, by previously placing the retro-pharyngeal gauze thus avoiding excessive extension of the mucosa.
After performing pulpotomies, chrome-steel crowns were placed on first primary molars 84 and 74; a chrome steel crown was placed on tooth 52. Sealant and resin were placed on teeth 75, 85, 64, 54. Pit and fissure sealant was placed in teeth 65 and 75. 2% lidocaine with epinephrime was infiltrated in front upper incisors, and the teeth were extracted. Gelfoam was used as hemostatic agent.
POST-OPERATIVE CARE AND FOLLOW-UP
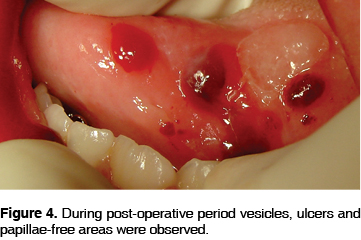
To finalize procedure, the oral cavity was carefully cleansed and the retropharyngeal gauze was removed. Upon examining the mouth, multiple ulcers and vesicles were found in the oral mucosa, as well as in the tip and dorsum of the tongue (Figures 4 and 5). Extubation was successfully accomplished; the anesthesiologist administered one single dose of dexamethasone (2 mg) ranitidine (30 mg) and metoclopramide (3 mg).

Patches were removed with the help of vaseline. No lesion caused by the anesthetic procedure was found in the skin. Nurses transferred the patient to the recovery room, where he received supplementary oxygen support.
Ninety minutes after the procedure, the patient was assessed by the anesthetist and pediatrician and discharged into the care of his family. House care, hygiene and nutrition type were recommended. The patient returned 8 days later, reporting slight discomfort in the mouth caused by the multiple ulcers inflicted during surgical procedure.
The patient was once more assessed 30 days after surgical procedure, at which point he exhibited better hygiene as well as lack of ulcers.
DISCUSSION
Epidermolysis bullosa is a disorder requiring comprehensive special care. Oral rehabilitation under general anesthesia implies monitoring management of surrounding tissue, as well as involved mucosa. Rehabilitation success is based upon precise knowledge of preoperative, intra-operative and postoperative care. We base our treatment upon the guide for this type of patients published by The Children's Hospital of Louisiana as well as the program of the Pedodontics Academy for special care patients. Different authors recommend use of moisturizers (Lubriderm, Eucerin®) adhesive patches (Duoderm®)18 so as to minimize skin trauma. It is important to protect oral mucosa with a rubber dam so as to avoid excessive damage to that tissue, protect it from the suction cannula, the ''flush'' of the high speed hand-piece, and retraction of specialized tissue. Previous application of oleic emollients on lips and corners of the mouth before the procedure is necessary to avoid formation of lesions around the mouth with their subsequent scar formation.
CONCLUSIONS
Management of this kind of patients is specific since it involves dermatologists, geneticists, anesthesiologists, pediatric surgeons, pediatric stomatologists, to mention only a few of the health professionals involved.
The oral cavity, specifically, experiences important changes in the soft tissues which then hinder adequate balanced nutrition and oral hygiene. As a result, these patients suffer a higher risk of developing caries.
The American Academy of Pedodontics recommends designing dental health prevention programs for office and home. As an example of this we have the ''dental home'' or home dental care based on a 12-month monitoring program. This program includes the understanding of oral diseases, oral habits, dental trauma, diet counseling, etc. It entails periodic visits to the dental office. With this care we could ensure specific prevention and close monitoring of the dental health of intra-oral and extra-oral tissues of this group of patients.20
REFERENCES
1. Lanier P, Posnik W, Donly K. Hereditary epidermolysis bullosa: oral manifestations and dental management and anesthetic consideration. Pediatric Dentistry 1990; 12 (4): 246-249. [ Links ]
2. Jobier-Al A. Hereditary epidermolysis bullosa: report of two cases. Departament of Preventive Dental Sciences 2001; 15 (2): 146-150. [ Links ]
3. Vargas A, Palomer L, Pallison F. Manifestaciones orales de la epidermólisis bulosa en el niño. Rev chil pediatr 2005; 76 (6): 612-616. [ Links ]
4. Presland B, Juveric J. Making sense of the ephitelial barrier: what molecular biology and genetics tell us about the funtions of oral mucosal and epidermal tissues. Journal of Dental Education 2002; 66 (4): 564-572 [ Links ]
5. Salas-Alanis JC, McGrath JA. Las epidermólisis bullosas distróficas en México: 2470 presentan la mutación más común en 21 familias. Gac Méd Méx 2006; 142 (1) 29-34. [ Links ]
6. Kao C, Chen S, Hwang, Yang B, Hsu C. Juctional Epidermolysis Bullosa. Journal Chinesse Medical Association 2006; 6 (10): 503-506. [ Links ]
7. Kosmidou A, Hector MP, Roberts GJ .Epidermolysis bullosa and dental developmental age. Int J Dent 2005; 15 (5): 335-341. [ Links ]
8. Timothy W, Fine J, Johnson L. Dental caries risk in hereditary epidermolysis bullosa. Pediatric Dentistry 1994; 16 (6): 427-432. [ Links ]
9. Timothy W, Fine J, Johnson L. Hereditary epidermolysis bullosa: oral manifestation and dental management. Pediatr Dent 1993; 15 (4): 242-248. [ Links ]
10. Kostara A, Roberts G, Gelbier M. Dental maturity in children with dystrophic epidermolysis bullosa. Pediatric Dentistry 2000; 22 (5): 385-388. [ Links ]
11. Harris CJ, Lucas VS. Dental disease and caries related microflora in children with dystrophic epidermolysis bullosa. Pediatr Dent 2001; 23 (5): 438-443. [ Links ]
12. Silva LC, Cruz RA, Abou-Id LR, Brini LN, Moreira LS. Clinical evaluation of patients with epidermolysis bullosa: review of the literature and case reports. Spec Care Dentist 2004; 24 (1): 22-27. [ Links ]
13. Kirkham J, Robinson C, Strafford SM, Shore RC, Bonass WA. The chemical composition of tooth enamel in junctional epidermolysis bullosa. Arch Oral Biol 2000; 45 (5): 377-386. [ Links ]
14. Ames W, Mayou B, Williams K. Anaesthetic of epidermolysis bullosa. British Journal of Anesthesia 1999; 82 (5): 746-751. [ Links ]
15. American Academy of Pediatric Dentistry. Guideline on management of person with special health care needs. Pediatric Dent 2004; 26: 77-80. [ Links ]
16. De la Lastra JL, Estrada N. Epidermólisis bullosa en el niño y anestesia. Rev Cubana Pediatr 1999; 71: 24-27. [ Links ]
17. Elliot Krane. Guidelines for the anesthetic management of epidermólisis bullosa . Lucile Packard Children's Hospital. Pediatric Anesthesia and Pain Management. Stanford University Medical Center. 2000. [ Links ]
18. Wright JT. Epidermolysis bullosa: dental and anesthetic management of two cases. Oral Surg Oral Med Oral Pathol 1984; 57: 155-157. [ Links ]
Note  Mailing address:
Mailing address:
Elizabeth Xóchitl García Cruz
E-mail: Eli_gc_66@hotmail.com
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam











 texto en
texto en 


