Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista odontológica mexicana
versión impresa ISSN 1870-199X
Rev. Odont. Mex vol.17 no.2 Ciudad de México abr./jun. 2013
Case report
Dental characteristics of hypophosphatemic rickets. Case report
Gabriela Godina Hernández,* Francisco Belmont Laguna§
* Graduate, Pediatric Stomatology Specialty, National Pediatrics Institute (Instituto Nacional de Pediatría), Mexico City.
§ Attached to the Pediatric Stomatology Specialty, National Pediatrics Institute, Mexico City.
ABSTRACT
Hypophosphatemic vitamin-D resistant rickets is characterized by persistent hypophosphatemia and hyperphosphaturia. This metabolic disorder causes deficient calcification of mineralized structures such as bones and teeth. One of the most important oral alterations elicited by this condition is the recurrent formation of ''spontaneous'' abscesses. These affect multiple caries or trauma to free primary o permanent teeth and are related to a deficient dentin mineralization. We report a case of hypophosphatemic vitamin-D resistant rickets in a patient who reported multiple dental abscesses and who required treatment consisting in pulpectomies, pulpotomies and chrome-steel crowns in molars and composite resin in anterior teeth. The aim of the present article was to raise awareness on the characteristics of this disorder, as well as its treatment and dental considerations.
Key words: Hypophosphatemic rickets, globular dentin, dental abscess, pulpotomy.
INTRODUCTION
Hypophosphatemic rickets (HR), also known as refractory, vitamin D resistant rickets, is a hereditary disease linked to the X chromosome. It is characterized by the metabolic disturbance of calcium and phosphate, which causes defective calcification of mineralized structures such as bones and teeth.1,2 It is the most common type of rickets found in developed countries. Its incidence can be counted at 1 in 20,000 individuals. It was first described in 1937 by Albright et al who reported that patients afflicted by this disease did not respond to usual vitamin-D treatment. Vitamin D is essential for the mineralization of bone matrix synthesized by osteoblasts.3
Pathophysiology of the disease consists on a decrease of phosphate resorption at the level of the kidney's proximal tubule. This elicits phosphate loss through urine, and therefore, persistent hypophosphatemia joined by anomalies in the calcium and phosphate intestinal resorption. Low phosphate levels in the blood cause bone mineralization defects with rickets signs and symptoms, which are frequently evident when patients reach about 18 months of age.4-6 This is a hereditary disease, with dominant transmission linked to sex chromosome X, therefore, affected males transmit the disease-responsible gene, located at the distal section of the short arm of the X chromosome (Xp22.1-p22.2) to all his female offspring and to none of the male ones, while an affected female transmits the gene to half her male offspring and half her female offspring, therefore, all her offspring, regardless of gender will have 50% probability of receiving the hypophosphatemic rickets gene.1,7,8
In 1995 HR gene was finally cloned, and the product of this gene, called PHEX gene (phosphate regulating gene with homologies with endopeptidases of the X chromosome) was an enzyme of unknown substrate. Nevertheless it is known that it expresses in osteoblasts and causes phosphate loss.9
SIGNS AND SYMPTOMS
Children afflicted with hypophosphatemic rickets present lower limbs arching, which initiates at around 18 months of age when their bones start supporting the load of their corporal weight as the child starts walking. These patients present duck-like gait (waddle), frontal bone bulging due to sagittal suture synostosis, costochondral joint enlargement, coxa vara, genu varum, genu valgum , and low body height.4,5,7,10,11
TREATMENT
Medical treatment consists on oral administration of phosphate in the form of neutral phosphate plus vitamin D solution, in the shape of calcitriol.6,7,10,11
DENTAL MANIFESTATIONS
In 1960 Harris and Sullivan reported for the first time dental characteristics of vitamin D-resistant hypophosphatemic rickets. They acknowledged them as the first perceivable signs of the disease.2,12
The disease is responsible for a defect in teeth mineralization, which causes a poorly mineralized and dysplastic dentin, with a non-calcified matrix which is called globular dentin. In these cases, there is also presence of tubular defects which can reach the dentin-enamel junction.13,16
In 1991, Seeto and Seow reported that dentin of HR patients was characterized by the presence of a great number of calcospherites separated by irregular zones of inter-globular dentin. During the normal mineralization process of dentin surrounding the pulp, calcospherites are formed through mineral deposits foci. Local mechanisms promote greater mineral apposition around deposit foci. These calcospherites created during pre-dentin growth, grow in a uniform manner through mineral increments, until contacting each other, therefore, in normal and totally mineralized dentin, appearance is homogeneous and external lines of each calcospherite are undistinguishable. In contrast to this, the incomplete fusion of calcospherites produces areas of inter-globular dentin. Based on this fact, we can suggest that calcospherite sites represent normal mineralization areas, and inter-globular spaces represent a non-mineralized matrix.6,8,11-13,17
Besides mineralization alterations, other reported characteristics are: normal but thin enamel, and especially enlarged pulp chambers as well as very high placed pulp horns extending until the dentin-enamel junction which are clearly visible in X rays.
The main dental finding of hypophosphatemic rickets cases, frequently reported in scientific literature, is the recurrent formation of dental abscesses which can affect caries or trauma free primary or permanent teeth. That is to say, apparently healthy teeth which develop ''spontaneous'' periapical abscesses.
This susceptibility to unexplained dental abscesses is related to the defect in dentin mineralization. It can only be histologically determined. This is also the case for pulp horns and chamber alterations. They explain the fact that the combination of these factors causes dental abscesses formation once the enamel integrity is compromised. Incipient caries or even simple physiological attrition can remove the thin enamel coating the pulp horn and thus allow microorganisms access to the pulp, through poorly calcified dentin, thus allowing pulp tissue infection and abscess formation in apparently unexplained, spontaneous manner.1,2,13,18-23
CLASSIFICATION
In 1986 Seow and Latham reported that dental characteristics can be present within a spectrum of manifestations, ranking from mild to severe, based on the number of abscesses as well as radiographic appearance of teeth.7
Grade I: presents minimum or lack of dental manifestation.
Grade II: moderate pulp enlargement with few dental abscesses.
Grade III: extremely large pulp chambers and multiple dental abscesses.
In 1989 Seow Seow et al coined the name of globular dentin to poorly mineralized dentin of HR patients. They conducted a biological study by analyzing the amount of globular dentin and inter-globular spaces so as to establish a histological classification and then find correlation among clinical manifestation classification published by Seow and Latham in 1986 and compare it with a classification governed by histological findings.4
Grade I: the amount of globular dentin is lesser than 50% of total dentin thickness and inter-globular spaces are small.
Grade II: the amount of globular dentin constitutes more than half the dentin thickness, inter-globular spaces are very large and there is greater tendency to find dentin fissures extending from the pulp up to the dentin-enamel junction.
Seow et al determined in this research the fact that severity spectrum of grade I, II and III previously reported by Seow and Latham in 1968 based upon clinical and radiographic findings was intimately related to the severity spectrum based upon globular dentin formation found in patient's histological studies.
In 1991, Seeto and Seow conducted a study in which they determined that the degree of dentin mineralization can be quantified by examining the size and fusion stage of the calcospherites. This in turn can be directly correlated with clinical and histological manifestations found in both previously conducted studies.17,23,24 A scanning electron microscope analysis was performed on calcospherites of HR patients to establish the degree of severity of dental manifestations.
Grade I: calcospherite fusion surpasses 75%, with relatively normal dentin. The limits of each calcospherite was hard to find, therefore size could not be assessed.
Grade II: fusion is from 50% to 75%. The diameter of each calcospherite is larger than 50 nm.
Grade III: fusion is under 50%. The diameter of each calcospherite is under 50 nm.
Based on results, the researchers determined that severity spectrum, established with the help of electron microscope, was correlated to clinical and histological findings found in previous studies. Patients with large pulp chambers and greater number of dental abscesses (grade III) showed smaller calcospherites and lesser degree of fusion. Contrarily, patients with normal-sized pulps and minimum number of dental abscesses (grade I) showed the largest calcospherites, which were found to be well-fused and with undistinguishable limits.
DENTAL TREATMENT
When treating hypophosphatemic rickets patients, prevention of abscesses plays a very important role. For this reason, Seow and Latham recommended that grade II and III patients should receive ''aggressive preventive'' treatment, which could include prophylactic pulpotomies, as well as placement of chrome-steel crowns in posterior teeth and resin restorations in anterior teeth. Grade I severity patients could only require routine preventive treatments such as pits and fissure sealants as well as topical application of fluoride.1-3, 7,12,13,21
CASE REPORT
4 year old male patient was referred from the National Rehabilitation Institute (Instituto Nacional de Rehabilitación) to the National Pediatrics Institute (Instituto Nacional de Pediatría) due to suspected hypophosphatemic rickets. Upon arrival it was reported the patient was under treatment of vitamin D and calcium supplements as well as sunbathing, which had yielded no improvement. The patient was examined at the genetic service, where x-ray and laboratory studies were requested. Studies revealed 2.4mg/dL phosphate in serum (normal values being 3.3 to 5.4 mg/dL) as well as a 147.60 mg/dL increase of phosphorus in urine (normal values being 16-20 mg/kg/day). The aforementioned findings corroborated a case of persistent hypophosphatemia, therefore the diagnosis of hypophosphatemic rickets was confirmed. Once the diagnosis was emitted the patient was referred to the stomatology service to receive dental treatment.
Extra-oral exploration revealed a male patient with clinical characteristics of base diagnosis emitted: bulging frontal bone, lower limb bow and genu varum (Figures 1 and 2).


Intra-oral examination revealed upper arch with caries-free, incomplete primary dentition, absence of teeth 51 and 61 due to extractions performed by a private dentist, scarring of fistulae at attached gingival level of those same teeth. The mother informed of multiple appearance of abscesses, which was the reason behind the extractions. Nevertheless the mother reported no history of trauma or caries (Figures 3 and 4).


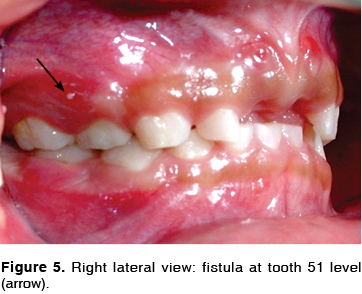
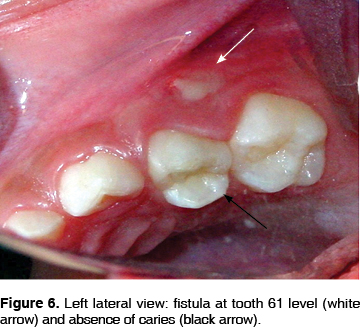
The patient presented presence of fistulae at the level of teeth 54 and 64, with purulent material egress. Nevertheless, affected teeth were found to be caries-free (Figures 5 and 6).
The lower arch showed complete, caries-free primary dentition, with probable fusion of teeth 72 and 73 (Figure 7). The mother reported that the patient experienced dental pain at the right lower molar for two days. The pain was soothed with analgesics administration. Nevertheless, there was no observed volume increase or color change in the attached gingiva, nor was there loss of muco-gingival fold in the affected region. The remaining structures were unaltered. Dento-alveolar x-rays revealed enlarged pulp chambers with pulp horns extending up to the dentin-enamel junction as well as fusion of teeth 72 and 73. The remaining structures were unaltered (Figure 8).

The base diagnosis of the patient was considered, as were clinical findings found in scientific literature. On the strength of that information, it was decided to conduct treatments recommended by several authors.
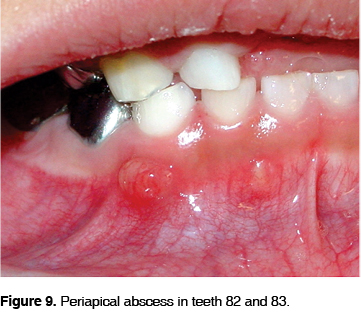
At the first appointment, a pulpotomy was performed in tooth number 84 and a pupectomy was conducted in tooth number 85. This was decided because, at the moment of gaining access, a necrotic distal conduct was found. At a later time chrome-steel crowns were placed on both molars. At the second appointment, the pulpectomy of tooth number 54 was performed, due to the presence of a fistula with egress of purulent material. The pulpotomy of tooth number 55 was performed with chrome steel crown. At the third appointment, an increase in volume was observed at the level of teeth 83 and 82. This was caused by periapical abscesses (Figures 9 and 10); it was then decided to perform pulpectomies of those teeth. Glass ionomer and resin restorations were then placed.

It is important to mention that, once the formation of new abscesses on the aforementioned teeth was observed, it was decided to extend preventive treatment with pulpotomies to the remaining canines which, so far, had not presented abscesses. Therefore, at the fourth appointment a pulpotomy with restoration made of glass ionomer and resin was performed on tooth 53.
At the fifth appointment, pulpotomies of teeth 74 and 75 were performed with later placement of chrome-steel crowns. Pulpotomies were performed in teeth 72 and 73, which were fused with glass ionomer and resin obturations.
At the sixth appointment, pulpotomy of tooth 63 was performed with resin and glass ionomer obturation as well as pulpectomy on tooth 64 and pulpotomy on tooth 65.Chrome-steel crowns were placed on both molars. Bands were adapted and upper and lower impressions were taken to build a prosthesis. Finally, the upper prosthesis was put into place. This provided restitution of teeth 51 and 52 and restored patient's function and aesthetics (Figures 11 and 12)
DISCUSSION
Hypophosphatemic rickets has been related to several primary and permanent teeth alterations. The most commonly reported include normal but thin enamel, globular dentin and enlarged pulp chambers with pulp horns extending up to the dentin-enamel junction. The aggregation of all these factors contributes to the formation of dental abscesses in cases when enamel is lost due to attrition or incipient caries and pulp infection takes place through poorly calcified dentin.6,7,9,13,20
Our patient was classified as a Grade III based upon clinical findings, since there were multiple dental abscesses in teeth 51, 61, 64, 54, 82 and 83. Histological classification proved to be impossible since we did not have formerly extracted teeth to be able to perform histological studies. Nevertheless, according to studies conducted by Seow and Seeto, there was an intimate relationship among clinical and histological characteristics found in studies conducted by the authors. We therefore consider our patient as histologically belonging to grade III.
Prophylactic pulpotomy and pulpectomy treatment initially recommended by Seow and Latham was later supported by McWhorter in 1991. In a study on abscess prevalence in a group of HR patients, he reached the conclusion that an abscess in one tooth indicates that at least one additional tooth will be equally affected. He therefore recommended that in cases when patients present more than one abscess in the absence of caries or trauma, choice treatment would be to perform prophylactic pulpotomies with chrome-steel crowns o all primary molars.1-3,7,11-13
Our patient presented abscesses in molars 64, 54, 51 and 61. During the course of treatment, abscesses occurred in teeth 83 and 82. I was then decided to extend prophylactic pulpotomy treatment to the rest of the canines which were, as yet, unaffected.
At the Instituto Nacional de Pediatria (National Pediatrics Institute) experience gained when treating this group of patients has allowed us to observe the fact that, when patients reach advanced stages of the disease, either due to a late diagnosis or lack of parental follow-up, their orthopedic alterations hinders proper stomatological treatment. One must consider that these are patients subjected to multiple kinds of treatment, surgeries, and orthopedic devices used to correct deformities. Behavioral management in these patients plays an essential role, firstly, because they are uncooperative as a result of the multiple treatments they have already been subjected to, and secondly due to parental over-protectiveness; both these factors unsettle patients behavior.
CONCLUSIONS
Hypophosphatemic rickets presents dental manifestations which must be known to the pediatric dentist, since timely treatment can prevent abscess formation, and therefore preserve teeth by performing adequate pulp treatment.
1. Patients afflicted with vitamin D-resistant hypophosphatemic rickets present multiple dental abscesses in the absence of caries or trauma history; they present as well pulp horns extending up to the dentin-enamel junction.
2. In cases when the patient presents abscesses in at least two teeth, according to experience gained at the Instituto Nacional de Pediatría (National Pediatrics Institute) it is recommended to perform pulpectomies in teeth presenting abscesses and prophylactic pulpotomies in the remaining as yet unaffected teeth. This can be achieved by placing chrome-steel crowns in molars and resin restorations in anterior teeth.
3. It is important to keep control of the patients, since there is the possibility they might suffer abscesses in other primary teeth, or even in permanent ones. Therefore, for a proper follow-up of this condition, parents must be made fully aware of its characteristics.
REFERENCES
1. McWhorter AG, Seale NS. Prevalence of dental abscess in a population of children with vitamin D-resistant rickets. Pediatr Dent 1991; 13 (2): 91-96. [ Links ]
2. Shroff D, McWhorter A. Evaluation of aggressive pulp therapy in a population of vitamin D-resistant rickets patients: a follow-up of 4 cases. Pediatr Dent 2002; 24: 347-349. [ Links ]
3. Cleverton RA, Maranhão CP. Endodontic treatment in patients with X-linked hypophosphatemic rickets. Braz J Oral Sci ; 1 (3): 129-132. [ Links ]
4. Seow WK, Romanink K, Sclavos S. Micromorphologic features of dentin in vitamin D-resistant rickets: correlation with clinical grading of severity. Pediatr Dent 1989; 11 (3): 203-208. [ Links ]
5. Demay MB, Sabbagh Y, Carpenter TO. Calcium and vitamin D: what is known about the effects on growing bone. Pediatrics 2007; 119 (Suppl 2): 141-144. [ Links ]
6. Goodman JR, Gelbier MJ, Bennett JH, Winter GB. Dental problems associated with hypophosphataemic vitamin D resistant rickets. Int J Paediatr Dent 1998; 8 (1): 19-28. [ Links ]
7. Seow WK, Latham SC. The spectrum of dental manifestations in vitamin D- resistant rickets: implications for management. Pediatr Dent 1986; 8 (2): 245-250. [ Links ]
8. Chaussain M, Sinding C. Dental abnormalities in patients with familial hypophosphatemic vitamin D-resistant rickets: prevention by early treatment with 1-hydroxyvitamin D. J Pediatr 2003; 142 (3): 324-331. [ Links ]
9. Econs MJ, Friedman NE, Rowe PS, Speer MC, Francis F, Strom TM. A PHEX gene mutation is responsible for adult-onset vitamin D-resistant hypophosphatemic osteomalacia: evidence that the disorder is not a distinct entity from X-linked hypophosphatemic rickets. J Clin Endocrinol Metab 1998; 83: 3459-3462. [ Links ]
10. Gallardo M, Arroyo G. Raquitismo hipofosfatémico. Presentación de un caso. Med Oral 2002; 4 (2): 42-44. [ Links ]
11. Larmas M, Hietala EL, Similä S, Pajari U. Oral manifestations of familial hypophosphatemic rickets after phosphate supplement therapy: a review of the literature and report of case. ASDC J Dent Child 1991; 58 (4): 328-334. [ Links ]
12. Breen GH. Prophylactic dental treatment for a patient with vitamin D- resistant rickets: report of case. ASDC J Dent Child 1986; 53 (1): 38-43. [ Links ]
13. Rakocz M, Keating J, Johnson R. Management of the primary dentition in vitamin D-resistant rickets. Oral Surg Oral Med Oral Pathol 1982; 54 (2):166-1671. [ Links ]
14. Ozkan S, Ucok Z, Alagöl F. Dental manifestations of familial hypophosphatemic vitamin-D-resistant rickets: report of case. J Dent Child 1984; 51 (6): 448-450. [ Links ]
15. Herbert FL. Hereditary hypophosphatemia rickets: an important awareness for dentists, case reports. J Dent Child 1986; 53 (3): 223-226. [ Links ]
16. Seow WK. X-linked hypophosphatemic vitamin D-resistant rickets. Aust Dent J 1984; 29 (6): 371-377. [ Links ]
17. Seeto E, Seow WK. Scanning electron microscopic analysis of dentin in vitamin D-resistant rickets: assessment of mineralization and correlation with clinical findings. Pediatr Dent 1991; 13 (1):43-48. [ Links ]
18. Tulloch EN, Andrews FFH. The association of dental abscesses with vitamin D-resistant rickets. Br Dent J 1983; 154: 136-138. [ Links ]
19. Murayama T, Iwatsubo R, Akiyama S, Amano A, Morisaki I. Familial hypophosphatemic vitamin D-resistant rickets: dental findings and histologic study of teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 90 (3): 310-316. [ Links ]
20. Hillmann G, Geurtsen W. Pathohistology of undecalcified primary teeth in vitamin D-resistant rickets: review and report of two cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996; 82 (2): 218-224. [ Links ]
21. Batra P, Tejani Z, Mars M. X-linked hypophosphatemia: dental and histologic findings. J Can Dent Assoc 2006; 72 (1): 69-72. [ Links ]
22. Kawakami M, Yamamoto T. Orthodontic treatment of a patient with hypophosphatemic Vitamin D resistant rickets. J Dent Child 1997; 64(6): 395-399. [ Links ]
23. Abe K, Ooshima T, Lily TS, Yasufuku Y, Sobue S. Structural deformities of deciduous teeth in patients with hypophosphatemic vitamin D-resistant rickets. Oral Surg Oral Med Oral Pathol 1988; 65 (2): 191-198. [ Links ]
24. Cohen S, Becker GL. Origin, diagnosis, and treatment of the dental manifestations of vitamin D-resistant rickets: a review of the literature and report of a case. J Am Dent Assoc 1976; 92 (1):120-129. [ Links ]
Note  Mailing address:
Mailing address:
Francisco Belmont Laguna
E-mail: fbelmont1@prodigy.net.mx
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam











 texto en
texto en 


