Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Revista odontológica mexicana
Print version ISSN 1870-199X
Rev. Odont. Mex vol.17 n.2 Ciudad de México Apr./Jun. 2013
Original research
Biocompatibility of n-butyl-cyanoacrylate compared to conventional skin sutures in skin wounds
Andrés Cáceres Barreno,* Carlos Cava Vergiú,§ José Robello Malatto,II Erika Alberca Ramos,* Jaime Rodríguez Chessa¶
* Teacher, Maxillofacial Surgery.
§ PhD in Dental Sciences, Dean of the School of Dentistry.
II PhD in Dental Sciences, Professor.
¶ Maxillofacial and Trauma Surgery Professor, Teacher at the School of Dentistry, San Martin de Porres University, San Luis, Lima, Peru.
School of Dentistry, San Martin de Porres University, San Luis, Lima Peru.
ABSTRACT
Introduction: N-Butyl-cyanoacrylate is a tissue-synthesis material. It offers countless advantages: short application time, easy execution, as well as possessing hemostatic character. This material is bacteriostatic, biodegradable, and exhibits suitable tensile strength. Objective: The objective of the present paper was the histological evaluation of n-butyl-cyanoacrylate biocompatibility on rats dorsum (spine), compared to braided black silk and Polyglactin 910. Materials and Methods: Thirty six Wixtar albino rats were used for the procedure. They were randomly divided into four groups (A, B, C, D) related to the time of sacrifice (3rd, 7th, 14th and 21st day) respectively. On the rats' spine, three 2 cm long incisions were performed. Histological parameters were as follows: polymorphonuclear cell inflammatory infiltrate, young fibroblasts and epidermis thickening. Results: N-butyl-cyanoacrylate caused lesser polymorphonuclear infiltrate when compared to other used materials. Fibroblast proliferation peaked in groups treated with n-butyl-cyanoacrylate when compared to the rest. Epidermis thickening showed high mitotic ability of keratocytes to remodel epithelium. At the 14th and 21st days most tissues treated with N-Butyl-cyanoacrylate were found to be completely remodeled when compared to the rest. Conclusion: N-butyl-cyanoacrylate was shown to be the most biocompatible material, since it elicited shortest healing time.
Key words: N-butil-cyanoacrylate, tissue adhesive, healing time.
INTRODUCTION
Cyanoacrylates (CAC) are tissue adhesives exhibiting the main objective of achieving coaptation of surgical wound borders, and thus eliciting healing.1 Ardis synthesized CAC for the first time in 1949. At a later point in time, in 1959, Coover informed on CAC adhesive properties. These compounds have been used in surgery since the 60's and 70's. Presently they are used in gastro-intestinal, abdominal, trauma, ENT, eye, cardiovascular, plastic and oral-maxillofacial surgeries.2-6
From the chemical perspective, CAC belong to the alkyl-cyanoacrylate family CH2 = C(CN)COOR. Differences among them lie in the composition of the lateral chain. We therefore have short-chain CAC (-ethyl, -methyl) and long chain CAC (-butyl and -octyl)CAC1-3.1-3 CAC are obtained from formaldehyde with cyanoacrylate synthesis in the presence of heat; they are vacuum carried. The monomer is formed, and then distilled, achieving a non-toxic, pure compound. When in contact with moisture or blood, CAC trigger a polymerization reaction between the CAC's lateral chain and serum proteins found in the liquid. Thus, microscopically, a tridimensional lattice (framework) is formed; resulting metabolites are then cyanoacetate and formaldehyde. Macroscopically, a thin and solid film can be observed which maintains closed the borders (edges) of the wound or incision.2-5
Ideal CAC exhibit many advantages, such as application time, minimal scarring, easy implementation. It also exhibits hemostatic, bacteriostatic and biodegradable characteristics.1-4 This composite material also exhibits suitable tensile strength against biological fluids and preserves tissues bonded during the whole of the healing process, without altering its immunology.7
The biocompatibility of this compound has been the subject of many research projects. Given the premise that it is a chemical compound and releases metabolites, it can then elicit the following histological changes: exacerbated inflammatory infiltrate, reaction to foreign body, necrotic areas in surrounding tissues, scar fibrosis in conjunctive tissue new formation as well as blood vessels genesis. All the aforementioned alterations bear effect upon the healing process, which is an essential phase for new tissue formation. CAC are used to seal esophageal bleeding, hepatic biliary fistulae sealing, synthesis of pediatric skin lacerations, sealing of perforated tympanic membranes, as well as in oral-maxillofacial surgery in procedures such as suture after removing retained teeth and soft tissue grafts.2-8Nevertheless, results obtained from the aforementioned research projects are not entirely clear. This is probably due to different methodologies employed as well as to the different chemical composition of each tissue adhesive. It can also be attributed to the performance of lax controls with respect to tissue healing periods, or to the fact that sometimes different numbers of days are used to conduct respective histological studies. Therefore, the aim of the present study was to assess, from the histological point of view, the biocompatibility of Butil-cyanoacrylate (B-CAC) in the dorsum of albino rats and compare it to braided black silk and polyglactin 910.
MATERIALS AND METHODS
The sample consisted of 36 Wixtar albino rats, ages ranking from 10 to 12 weeks, weight 150-200 grams respectively. Rats were randomly divided into four, 9 specimens groups (A, B, C, D), correlated to sacrifice times (3er, 7th, 14th and 21st day respectively). Animals were kept and manipulated according to norms established by the Biotery of the Research Institute, Human Medicine School, San Martín de Porres University. The present research project was approved by the Research Institute, School of Dentistry, San Martín de Porres University. Specimens were kept at the same temperature and humidity conditions in individual metabolic cages.
Specimens received 3-6 grams balanced feed and 3-7 mL filtered potable water.
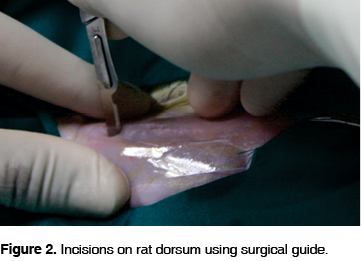
Specimens were anesthetized with intra-peritoneal infiltration of sodium pentobarbital (HALATAL ®) dosed at 1 mL/2.5 kg weight. They were placed in a prone position in a positioning device specifically designed for the research project. A plastic surgical guide was used to standardize the sample (Figures 1 and 2). Three 2 cm incisions were performed on the rats' dorsum. Incisions exhibited a 2 cm separation among them (Figure 3).


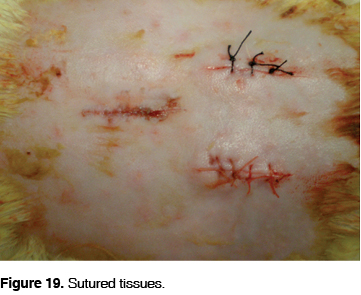
At a later point, a tissue synthesis of every incision was conducted. In all groups, different materials were used for each separate incision: butyl CAC (2 drops) and braided black silk suture thread 5/0 (BBS) and polyglactin 910 5/0 respectively. Animals were euthanized with a sharp blow to the cervical vertebrae at the 3rd, 7th, 14th, and 21st days respectively.
Harvested tissue samples were fixated, processed and included in paraffin.
At a later point, cuts were performed with a 6 µm microtome. After this, dyeing with hematoxilin and eosin was conducted, to then be subjected to histopathological analysis with high power optical microscope (40X). Methodology used for the research was counting high power (40X) visual fields (VF). Thus the following was assessed: number of VF polymorphonuclear cell inflammatory infiltrate (Mild: 0-1 VF, moderate: 1-3 VF and severe: 4 or more VF). Presence or absence of young fibroblasts and thickening of the epidermis were also assessed.
RESULTS
HISTOPATHOLOGICAL EVALUATION
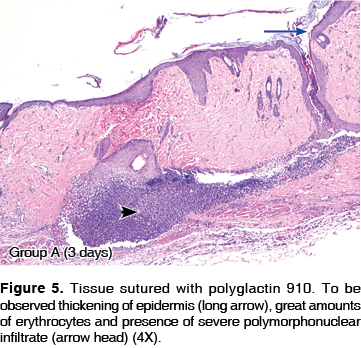
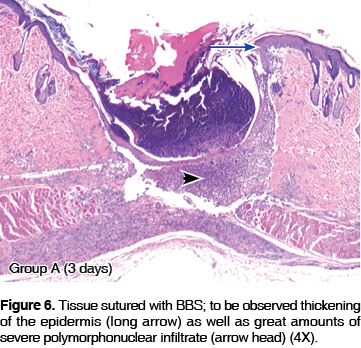
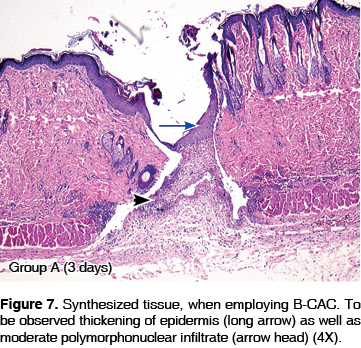
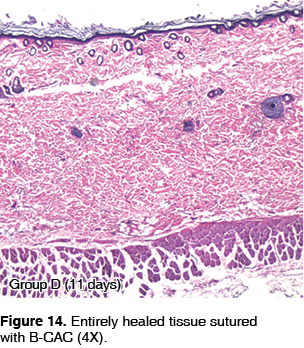
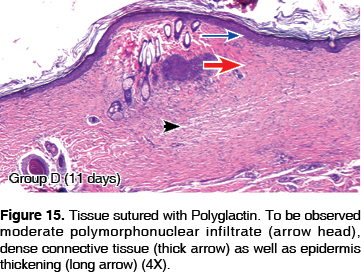
On the 3rd day, it was observed that 54% of cases exhibiting severe polymorphonuclear infiltrate belonged to the polyglactin 910 group (Figures 4 and 5) when compared with 37% BBS (Figure 6) and 9% B-CAC (Figure 7). On the 7th day, 50% of cases presenting severe polymorphonuclear infiltrate belonged to the BBS group (Figures 4 and 8) followed by polyglactin 910 with 40% (Figure 9) and finally B-CAC with 10% (Figure 10). On the 14th day, 40% of cases sutured with BBS (Figure 11) and 60% of cases sutured with polyglactin 910 (Figure 12) still exhibited severe polymorphonuclear infiltrate, as opposed to tissues synthesized with B-CAC which did not present, in any of the cases, severe inflammatory infiltrate (Figure 13). On the 21st day there was no evidence of severe polymorphonuclear infiltrate as a response to B-CAC (Figure 14), as opposed to cases sutured with polyglactin 910 (Figure 15) and BBS (Figure 16), which respectively still represented 56 and 44% of all cases.
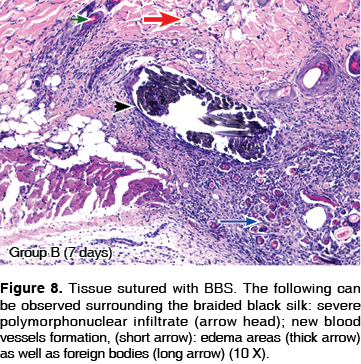
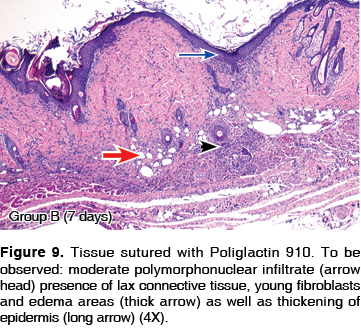
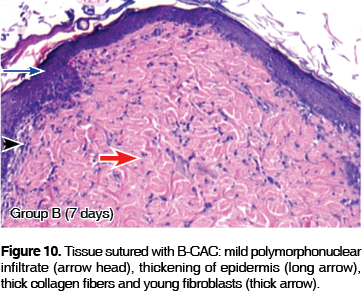
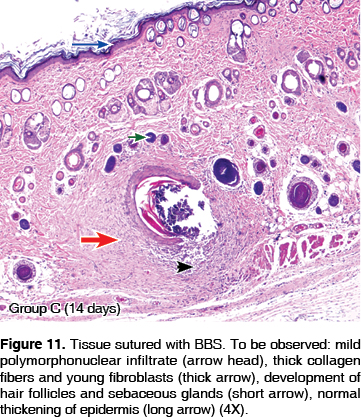
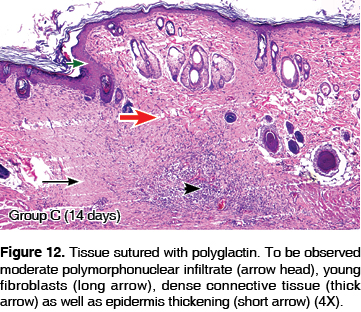
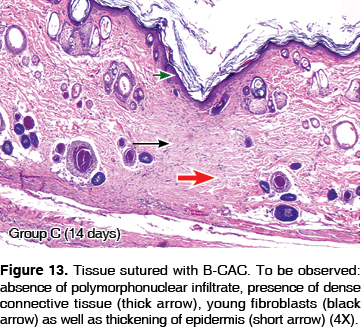

With respect to presence of young fibroblasts, on the 7th day it was observed that 67% specimens presenting young fibroblasts belonged to the B-CAC group (Figures 10 and 17), while the polyglactin 910 group represented 33% (Figure 9). SNT did not present any case (Figure 8). At the 14th day, 39% of cases belonging to the polyglactin 910 group presented young fibroblasts (Figure 12); SNT (Figure 11) and B-CAC (Figure 13) represented 33 and 28% of cases respectively.
Finally, at the 21st day, only 8% of the cases in the B-CAC group exhibited young fibroblasts (Figure 14) when compared to BBS (Figure 16) and polyglactin 910 (Figure 15), which represented 42% and 50% respectively of cases experiencing remodeling process.
On the third day, thickening of the epidermis was observed in 50% of all cases sutured with synthesis materials (Figures 5, 6 and 7) while the remaining 50% did not show any changes (Figure 18). On the 7th day, 46% of cases belonging to B-CAC group showed thickening of the epidermis (Figure 10). polyglactin 910 (Figure 9) and BBS (Figure 8) represented each 27% of all cases. On the 14th day, 17% of specimens belonging to the B-CAC group presented epidermis thickening (Figure 13) as opposed to groups treated with BBS (Figure 11) and polyglactin 910 (Figure 12), whose percentages were 33% and 50% respectively. On the 21st day none of the B-CAC group specimens showed increase of the epidermis and tissues appeared totally healed (Figure 14) The opposite was the case of BBS group cases (Figure 16) and polyglactin 910 cases (Figure 15) whose percentages were 38% and 62% respectively (Figure 18).
DISCUSSION
There is a great variety of absorbable and non-absorbable synthesis materials; they can be of animal or synthetic origin, and in turn can present single or multiple stranded design.8 CAC are considered an alternative to tissue synthesis materials. Among them butyl cyanoacrylate is the most biocompatible. This was supported with methodology used in this research project, since no evidence of necrotic areas was found as well as exacerbated inflammatory infiltrate; they exhibited suitable fluidity, and good hemostasis control was observed during surgical events, they also presented bacteriostatic properties.9-11 This product was selected due to the aforementioned properties. Nevertheless, Moretti et al1 proceeded to sub-cutaneously implant 3 cyanoacrylates: ethyl cyanoacrylate, alfa-cyanoacrylate and butyl-cyanoacrylate. The procedure was performed with a sponge soaked in the material. Tissue reaction elicited by all three materials was compared. Results favored alpha-cyanoacrylate, which exhibited better biocompatibility. When compared to our research, this was confronted to skin suture, simulating daily clinical practice events.
According to De Souza et al,15 in his search to contribute with an effective healing process, where synthesis material should not represent an interference with cell biology, butyl cyanoacrylate allowed metabolic exchange at the level of connective and epithelial tissues, since it did not cause needle micro-trauma which could elicit severe inflammatory response. In the present research project corroboration of aforementioned facts was established, as well as the fact that suture permanence in tissues, in spite of having used absorbable suture material, delayed healing processes at 14 and 21 days. This might be due to the fact that the body, striving to eliminate foreign bodies, secretes polymorphonuclear inflammatory cells to expel sutures, prolonging thus tissue remodeling period.12-13
Each healing phase involves a particular type of cells to achieve specific functions. On the third day (acute inflammatory phase), at epithelial level, epidermis thickness was increased in all cases. In connective tissue, it was observed that polyglactin 910 presented greater number of severe polymorphonuclear infiltrate cases, whereas butyl cyanoacrylate and braided black silk elicited moderate to mild polymorphonuclear infiltrate. Yaltririk et al6 reported otherwise: they informed that polyglactin 910 was the material originating less polymorphonuclear infiltrate on the 3rd day. This was probably due to the fact that the aforementioned material was compared to chromic catgut, which itself elicits a more severe tissue friction, producing thus more severe polymorphonuclear response in acute stages.
At connective tissue level, on the 7th day, which corresponded to a transition period between inflammatory and proliferative healing, polymorphonuclear cells were still found in lesser number of visual fields. In addition, young fibroblasts were observed forming a lax connective tissue (young connective tissue with thin collagen fibers which will constantly thicken to maturity). Notwithstanding, Kulkami et al5 reported that in their research, upon the 7th day, there were great amounts of polymorphonuclear cells, predominantly moderate to severe: they did not observe young fibroblasts. Nevertheless, in the present research, 13% of all studied cases presented the aforementioned cells at that stage. This could be due to the fact that in methodology used by these authors, incisions were intra-oral, at the level of dental papillae, therefore, harvesting of minute portions became a difficult task. Furthermore, a 1.5 cm margin on both sides of the incision (so as to observe histological changes) was not observed. To all the aforementioned, aggregated factors could be the accumulation of plaque and hygiene, which would extend the inflammatory phase, and elicit only on the 21st day, the appearance of young fibroblasts and greater amounts of dense connective tissue.2, 14-15
Upon the 14th day, clearly pertaining to healing proliferative phase, no instances of severe inflammatory infiltrate were found in tissues sutured with B-CAC. Absence of young fibroblasts in 65% of these cases showed connective tissue maturation process. With respect to epidermis thickening, Kulkani et al5 as well as Moretti et al1 did not consider this parameter for their respective research projects. Additionally, the aforementioned authors did not count with a 14th day study group. Yatltirik et al,6 only provided assessments up to the 7th day; Kulkarni et al5 and Moretti et al1 conducted their second control on the 21st day. The fact of lacking control precludes proper fibroblastic proliferation assessment, since, from the physiological point of view, this would represent their highest point of activity. In the present research project, on the 7th and 14th day, in histological slides, great fibroblastic proliferation was observed, and differences originated by each synthesis material at proliferative stage could be determined.
On the 21st day, healing process was in a final remodeling phase in which absence of young fibroblasts indicated that they were mostly in their mature phase. Several research projects used different assessment periods. Such was the case of Yaltirik et al6 who assessed healing in the first 7 days, but did not include neither the proliferative nor the remodeling tissue phases. In contrast, Moretti et al1 left synthesis materials in situ for periods up to 45 days; originating thus great amounts of histiocytes caused by excessive exposition times. Macrophages encapsulated all elements foreign to the body, forming thus a large-sized, multinucleated cell called histiocyte1-4, 12-15. This histiocyte migrated towards the epidermis' stratum corneum, to be later eliminated. It can be deduced that not all formed histiocytes are necessarily originated by the synthesis material itself, but rather to the prolonged exposition time to the tissues. This fact was confirmed in our study. The thickening of the epidermis, evident in all slides, can be construed as an innovative datum of the present research. This thickening was produced due to the increase of keratinocytes, which reproduce through mitosis, with the aim of helping healing processes.
The epidermis of albino rats was composed of three well defined layers. On the 3rd and 7th days, the size of all layers was noticeably increased. This was due to the intense mitotic activity caused by keratocytes' attempt to repair damage. On the 14th to 21st day, layers would gradually return to normal thickness, since healing process was coming to an end. This was not apparent in groups treated with sutures due to the fact that there still was a polymorphonuclear infiltrate which was engulfing synthesis material, delaying proliferative and remodeling phases.
Healing time of tissues treated with B-CAC was lesser, and acted as a barrier against micro-organism penetration, reducing tissue coaptation time, and the material being biodegradable, later removal was not necessary. The present research project established B-CAC properties in the skin of test animals. It is recommended to conduct further clinical research on the behavior of this product in the mouth of human beings, bearing in mind it is a different material associated to other organics states such as salivary pH, organic substances as well as the probable influence of lingual muscle forces which could cause dehiscences.
CONCLUSIONS
According to research parameters and used methodology we can conclude the following:
1. Butyl cyanoacrylate was a biocompatible material which allowed normal healing of incised tissues.
2. During studied time intervals, tissue polymorphonuclear infiltrate, where B-CAC was used, considerably decreased when compared to BBS and polyglactin 910
3. When B-CAC was used, the number of young fibroblasts was noticeably higher than in the rest of cases. Dense reparative connective tissue was observed at shorter times.
4. Epidermis thickening considerably decreased in tissues treated with B-CAC, when compared to BBS and Polyglactin 910.
REFERENCES
1. Moretti Neto R, Mello I, Silveira Moretti A, Colombo Robazza C, Costa Pereira A. In vivo qualitative analysis of the biocompatibility of different cyanoacrylate based adhesives. Braz Oral Rev 2008; 22 (1): 43-47. [ Links ]
2. Fotiadis C, Leventis I, Adamis S, Gorgoulis V, Domeyer P, Zografos G et al. The use of isobutylcyanoacrylate as a tissue adhesive in abdominal surgery. Acta Chir Belg 2005; 105 (4): 392-396. [ Links ]
3. Dilege E, Deveci U, Erbil Y, Dinççağ A, Seven R, Ozarmagan S et al. N-butyl cyanoacrylate versus conventional suturing for fixation of meshes in an incisional hernia model. J Invest Surg 2010; 23 (5): 262-266. [ Links ]
4. Samuel PR, Roberts AC, Nigam A. The use of Indermil (n-butyl cyanoacrylate) in otorhinolaryngology and head and neck surgery. A preliminary report on the first 33 patients. J Laryngol Otol 1997; 111 (6): 536-40. [ Links ]
5. Kulkarni S, Dodwad V, Chava V. Healing of periodontal flaps when closed with silk sutures and N-butyl cyanoacrylate. A clinical and histological study. Indian J Dent Rest 2007; 18 (2): 72-77. [ Links ]
6. Yaltirik M, Dedeoglu K, Bilgic B, Koray M, Errev H, Issever H et al. Comparison of four different suture materials in soft tissues of rats. Oral diseases 2003; 9: 284-286. [ Links ]
7. Marques Batista C, Colloni Neto R, Lopes Filho G. Comparative study of the healing process of the aponeurosis of the anterior abdominal wall of rats after wound clousure using 3-0 nylon suture and N-butyl-cyanoacrylate tissue adhesive. Acta Cir Bras 2008; 23 (4): 353-363. [ Links ]
8. Bloor BK, Tidman N, Leigh IM, Odell E, Dogan B, Wollina U et al. Expression of keratin K2e in cutaneous and oral lesions: association with keratinocyte activation, proliferation, and keratinization. Am J Pathol 2003; 162 (3): 963-75. [ Links ]
9. Guerra Bretaña R, Pérez Ávarez M, Roque Gonzales R, Bomant Cuang E, Gonzales Rodriguez Y, Palenzuela Mauriz T. Efectividad del adhesivo tisuacryl en el cierre de heridas cutáneas. Rev Cub Cir 2005; 50 (2): 179-186. [ Links ]
10. García Simons G, Cañizares Graupera M, Arteaga Hernández E. Efecto del tisuacryl sobre la mucosa bucal. Rev. Cenic Ciencias Biológicas 2006; 37(3): 153-155. [ Links ]
11. Castro H, Della A, Avila V. Physical properties of suture threads used in dentistry. Cienc Odontol Bras 2007; 10 (2): 85-90. [ Links ]
12. Abdallah E, Barbosa F, Zenobio E, Soares R. Cyanoacrylate based tissue adhesives: literature review. Rev Saude 2008; 2 (1): 36-40. [ Links ]
13. Mo X, Iwata H, Ikada Y. Tissue adhesives evaluated in vitro and in vivo analysis. J Biomed Mater Rest 2010; 94 (1): 326-332. [ Links ]
14. Gonzales Y, Guerra R, Durán I, Prieto E. Esterilización, estabilización y estudio del carácter antimicrobiano del Tisuacryl. Rev CENIC 2006; 37 (3): 137-141. [ Links ]
15. Souza SC, Oliveira WL, Soares DF, Briglia CH, Athanázio PR, Cerqueira MD et al. Comparative study of suture and cyanoacrylates in skin closure of rats. Acta Cir Bras 2007; 22 (4): 309-316. [ Links ]
LECTURAS RECOMENDADAS
1. Saska S, Gaspar AM, Hochuli-Vieira E. Adhesivos a base de cianoacrilatopara sintese de tecido mole. An Bras Dermatol 2009; 84 (6): 595-92. [ Links ]
2. Hyvarinen K, Richardson R, Rihtneemi J, Teronen O. Comparison between monofilament suture and braided suture and their influence on oral wound healing. International journal of oral & Maxillofacial Surgery 2007; 36 (11): 1092-1096. [ Links ]
3. Banche G, Roana J, Manchas N, Amario M, Gallerio C, Allizond V et al. Microbial adherence on various intraoral suture materials in patients undergoing dental surgery. Journal of oral & Maxillofacial Surgery 2007; 65 (8): 1503-1507. [ Links ]
 Mailing address:
Mailing address:
Esperanza Raquel Ayón Haro
E-mail: eayonh@usmp.pe
Note
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam











 text in
text in 


