Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista odontológica mexicana
versión impresa ISSN 1870-199X
Rev. Odont. Mex vol.16 no.2 Ciudad de México abr./jun. 2012
Case reports
Upper jaw chronic osteomyelitis. Report of four clinical cases
Alberto Wintergerst Fish,* Carlos Javier Iturralde Espinosa,§ Vladimir de la Riva Parra,II Santiago Reinoso QuezadaII
* Oral Surgery Professor, Graduate Department of the National School of Dentistry, National University of Mexico (UNAM), Maxillofacial Surgeon, the Maxillofacial Surgery Service, Hospital 20 de Noviembre, National Medical Center, ISSSTE, Mexico City.
§ Teacher, School of Dentistry, Universidad Latinoamericana, Mexico City.
II Maxillofacial Surgeon, private practice.
ABSTRACT
Osteomyelitis is an inflammatory bone disease commonly related to an infectious origin caused by germs, mainly pyogenic staphylococcus, and occasionally, streptococci, pneumococci and enterobacteriae. Several treatments and classifications for osteomyelitis have been established. These are based on clinical course, pathologic-anatomical or radiologic features, etiology and pathogenesis. Chronic osteomyelitis is a complication of non-treated or inadequately treated acute osteomyleitis. It can also be caused by a low grade prolonged inflammatory reaction. This study presents four cases of maxillary osteomyelitis treated between 2007 and 2009. Cases were treated with antimicrobial therapy. Preoperatively, patients were prescribed Clindamycin, 300 mg every eight hours, Cefriaxone, 1 g IV every 12 hours. Cases were surgically treated with subtotal hemi-maxillectomy. Postoperatively, cases were treated with Penicillin G 800,000 units IM per day, for 30 days. All cases evolved satisfactorily without relapse.
Key words: Maxillary chronic osteomyelitis, subtotal hemi-maxillectomy.
INTRODUCTION
Osteomyelitis is an inflammatory bone disease affecting bone marrow. It frequently compromises cortical bone and periosteum.1-8 Before the advent of antibiotics, it was a life-threatening disease; in our days, if adequately treated, it can resolve satisfactorily. One of the first reports on osteomyelitis was written in 1832 by British physician Sir Benjamin Brodie, who for the first time described a type of abscess, which in our days is known as the Brodie abscess, and which represents one of the chronic features of osteomyelitis.9
Inflammation has its origin in the bone marrow, and extends to cancellous bone spaces. It then spreads through blood vessels, fibro-elastic tissues, and eventually to the periosteum. When the vascularity of bone tissue is compromised, it induces bone necrosis and sequestration.2,3,6-8
Osteomyelitis typically appears during the 5th and 6th decades of life. It is associated to systemic diseases such as diabetes mellitus, auto-immune diseases, agranulocytosis, leukemia, anemia, nutritional deficiencies, syphilis, cancer, chemotherapy and radiotherapy, as well as habits of alcohol or tobacco consumption.7
In the maxillofacial region, the lower jaw is more frequently affected than the upper one. This is due to the fact that, in the upper jaw, there is cancellous bone tissue with greater vascular supply, which hinders bacterial colonization, since cellular response is enhanced and has greater blood flow which thus counteracts bone invasion.10,11
Notwithstanding, in the upper jaw anterior region, vascular supply is juxta-terminal thus favoring bone sequestration, this is due to blood being compromised and eliciting as a consequence oral-nasal communication.12,13
Upper jaw osteomyelitis shows predilection for infants and children in their first decade of life. This is due to the fact that the upper jaw includes dental buds and therefore there is a more intense vascular irrigation, which can become the origin of hematogenous osteomyelitis or by a neighboring skin process due to a staphylococci infection in the infant.2
Lower jaw vascular supply is very singular: when there is an intense osteomyelitic infection, there is greater probability to develop bone sequestrations. This is due to a terminal type irrigation which cannot compensate peripheral vascular supply of gums and periodontium. Due to vascular thromboses and endoarteritis or sympathetic and parasympathetic vegetative reflexes, a vasoconstriction of these vessels is produced. As a result of odontogenic infection, osteomyelitis can be generated in upper or lower jaws.8
Lew and Waldvoger14 classify osteomyelitis into suppurative and non-suppurative, depending on its infectious character or hematogenous origin (Table I).7
Habitually, clinical background reveals history of odontogenic infection of periodontal or dental pulp tissue origin; it might also reveal history of facial trauma, especially poorly consolidated fractures.7
In chronic osteomyelitis cases, the background is normally related to previous acute osteomyelitis, with presence of old fistulae, or active fistulae with purulent secretion, with a segment of poorly vascularized, pigmented, atrophic skin, found adhered to the bone and which ulcerates easily. Pain to palpation and soft tissue induration are also present.1,7
Osteomyelitis treatments require antibiotics and surgery. Treatment principles consist of the following: stabilizing systemic conditions of the immune-compromised patient, culture of associated microorganisms, sensitivity tests, image assessment to determine lesion extension, empiric administration of antimicrobial drugs to combat predominant microorganisms, removal of septic foci such as teeth and bone sequestrations, drug prescription based on cultures and antibiogram, sequestration, debridement, decortication or resection according to the case.3,6-8,15
Several authors have described, with satisfactory results, adjuvant treatments for chronic osteomyelitis such as use of non-steroid anti-inflammatory drugs, corticosteroids, biphosphonates and hyperbaric oxygen therapy.1,7,10,12-14,16,17
CLINICAL CASES
CASE 1
60 year old male patient attending the Maxillofacial Surgery Service at the National Medical Center ''20 de Noviembre'' I.S.S.S.T.E., Mexico City. The patient describes the onset of his affliction as dental pain, previously treated with upper left second molar extraction. The patient received non-specific pharmacological therapy as well as unknown surgical treatment. Clinically, the patient presented the following: a 2 x 1 mm fistula in upper left premolar region, severe halitosis, asthenia, adynamia, left cranial headache, chronic periodontal disease, as well as several missing teeth. Computed tomography showed lytic areas with sclerotic borders, periosteal reaction and bone sequestration (Figure 1). CBC revealed the following: haemoglobin: 14 g/dL, leukocytes 7.44 cpm, glucose: 109 g/dL. Pharmacological treatment was undertaken with Clindamycin 600 mg IV every 8 hours, and Ceftriaxone, 1 g IV every 12 hours. It was decided to perform subtotal hemi-maxillectomy under balanced inhalation general anesthesia. A 6 cm circular-vestibular approach was carried out, dissecting tissues until exposing the lesion. Bone necrosis areas were observed (Figure 2). A 3 x 3 cm surgical specimen was obtained, finding foul smelling, black necrotic areas. Macroscopically, lesion free borders were verified, and tissues were sutured with triple cero polyglycolic acid sutures.


The surgical specimen was sent to the oral pathologist, who reported the presence of maxillary chronic osteomyelitis with lesion free borders. The patients continued with ambulatory antimicrobial treatment with Procaine G Penicillin, 800,000 U, IM, every 24 hours during 30 days. At a later stage, the patient was sent to the maxillofacial prostheses service for rehabilitation. Presently, the patient remains asymptomatic after a 21 year control period. No relapse was observed (Figure 3).

CASE 2
44 year old female patient, with 15 year evolution type II diabetes mellitus history, controlled with Glibenclamide. The patient reported her present condition was triggered by the extraction of an upper anterior tooth. The patient experienced a torpid healing process, of poor evolution, which persisted during 6 months, with periods of lesion exacerbation and purulent material egress. The patient received curettage treatment. Drug therapy consisted on administration of Ampicilin, Amoxicilin and Clindamycin. Painful symptoms did not remit. The patient was then referred to the Maxillofacial Surgery Service, National Medical Center ''20 de Noviembre'' I.S.S.S.T.E, Mexico City. At this service, a computed tomography was performed, where lytic borders and maxillar affectation with hypo-dense zones and maxillary sinus invasion were observed. CBC revealed the following: hemoglobin 14 g/dL, leukocytes: 6.3 cpm, glucose, 105 g/dL.
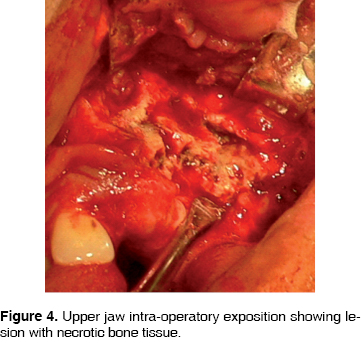
Treatment was initiated with Clindamycin 600 mg, IV every 8 hours and Ceftriaxone 1 g IV every 12 hours. Following this, a subtotal hemimaxillectomy was performed under balanced inhalation general anesthesia. The procedure was carried out performing a circum-vestibular approach. During the procedure, necrotic and lytic bone areas were observed (Figure 4). Resection of the lesion was then undertaken: a 2 x 4 cm surgical specimen was harvested. Suturing was performed with treble cero polyglycolic acid. The surgical sample was sent to the oral pathologist who reported upper jaw chronic osteomyelitis with lesion free borders. The patient followed a 30 day treatment with Procain G Penicillin, IU IM every 24 hours. The patient shows currently no relapse when examined through imaging or clinically examined (Figures 5 and 6).


CASE 3
46 year old male with history of uncontrolled type II diabetes mellitus and uncontrolled, 15 year evolution. Systemic arterial hypertension. The patient's condition initiated 3 months prior to the visit; he informed of pain in the upper tooth, which he proceeded to extract himself. Two weeks after this event he experienced painful symptoms in the upper anterior region, informing of halitosis and foul taste in the mouth. He evolved for three months with peri-orbital edema, palpebral occlusion, skin fistula in the left nostril, 0.5 mm fistula intra-orally in the maxillary vestibule, with no egress of purulent matter. A computerized tomography was performed, where lytic areas were observed in the maxillary ascending process and maxillary process of malar bone, the maxillary sinus was invaded (Figure 7). CBC values were as follows: hemoglobin 11.3 g/dL, leukocytes 8.92 cpm, glucose 123 g/dL. Pharmacological treatment was undertaken with clindamycin 600 mg IV every 6 hours and Ceftriaxone, 1 g IV every 12 hours. At a later point, a subtotal hemimaxillectomy was performed preserving the lower orbital ridge. Surgery was performed under balanced inhalation general anesthesia, observing a 5 cm circum-vestibular approach, dissecting tissue until reaching bone exposition. Bone necrotic areas were observed. A 4.5 x 4 cm surgical specimen was harvested. Lesion free bone borders were clinically observed. Sutures were performed with treble cero polyglycolic acid material. The surgical sample was sent to the oral pathologist, who informed of maxillary chronic osteomyelitis with lesion free borders. The patient continued with the following out-patient pharmacological treatment: Procain G Penicillin, 800,000 IU every 12 hours for 30 days. Currently, after 8 months, the patient shows no relapse (Figure 8).


CASE 4
64 year old male, allergic to penicillin. He informed of a history of prostate carcinoma, treated with prostatic radiotherapy and surgery 5 years before. The patient's condition initiated two months before the visit, after extraction of upper right second premolar and first molar. There was an untoward evolution with presence of pain, halitosis, facial peripheral edema, as well as volume increase in the posterior right maxillary region. CBC values were as follows: hemoglobin 11.3 g/dL, leukocytes 4.44 cpm, glucose 84 g/dL. Pharmacological treatment was initiated with right subtotal hemi-maxillectomy. Surgery was performed under balanced inhalation general anesthesia, through a 6 cm circum- vestibular approach, dissecting tissue until reaching bone exposition (Figure 9). Necrotic bone areas were observed. A 7 x 6.5 bone resection was performed (Figure 10). Lesion free bone borders were clinically verified. Suturing was performed with treble cero polyglycolic acid material.


Histopathologically, maxillary chronic osteomyelitis was confirmed, presenting lesion free borders. Out-patient treatment was initiated with Clindamycin 300 mg, every 8 hours for 30 days. Currently the patient is at a two year control phase, showing no relapse.
DISCUSSION
Chronic osteomyelitis is an inflammatory disease generally involving several bones, and is commonly encountered in long bones metaphysis.5,16 In many cases, extensive bone resection and reconstruction are standard treatments. Chronic osteomyelitis shows predilection for the lower jaw. The most frequently found complication is bone fracture.3,6,8,14-16
Radiographically, chronic osteomyelitis mainly appears as a radio-transparent lesion which sometimes shows opaque focal areas. Lesions are normally quite extended, often with undistinguishable borders.3,6,8,15,16
In vascular phase gammagraphy, early arterial hyperemia is observed, with increase of focal or diffuse tracer uptake. In delayed imaging markers, progressive focal accumulation is observed in the affected bone7,15,16
In chronic osteomyelitis hystopathological microscopic examination, an inflammatory-like bone reaction is observed, which can vary from mild to severe. In mild cases microscopic diagnosis can be difficult due to existing similarities with osteo-fibrous anomalies such as ossifying fibroma and fibrous dysplasia.3,7,8
Leukocyte count can be normal, or slightly raised up to 20,000 Cs/mm3. Erythrocyte sedimentation rank can be slightly accrued, but, differing from long bones involvement, in the maxillofacial region, it is rarely a valid indicator during the clinical course of the disease. Blood cultures have little diagnostic value.7,15
The specific infectious agent responsible for chronic osteomyelitis is difficult to identify. Previously administered antibiotics also reduce the possibility of obtaining a culture of the accountable microorganism. Even though an etiologic agent is frequently not confirmed, most researchers consider that bacteria (staphylococci, streptococci, bacteroids, actinomyces) are responsible for the best part of chronic osteomyelitis cases; especially Staphilococcus aureus and Staphylococus epidermis which are found present in 80 to 90% of cases. There is also an associated mixed flora, like hemolytic streptococci, pneumococci, Escheriquia coli and Actinomyces. 7
Topazian et al7 use antimicrobial treatments for long periods of time, from 6 to 12 months. They recommend treatment mainly with Beta lactam, Clindamycin, and Metronidazol. Many microorganisms responsible for osteomyelitis are penicillin resistant; such is the case of Prevotella, Porphyromonas and Fusobacterium. For this reason, Metronidazol should be incorporated to penicillin to counteract penicillin-resistant aerobic and anaerobic streptococci.10 Some examples of these combinations could be: Penicillin + Metronidazol, Amoxicillin + Metronidazol, Amoxicillin + clavulanic acid, Ampicillin + Sulbactam, Clindamycin, Metronidazol, Cephalosporin. Schemes are used for penicillin as first drug, due to its antimicrobial specter. Reccomended dosage is 4,000,000 UI of crystallized sodium G penicillin every 4 to six hours, combined with Metronidazol, 500 mg, every 6 hours for 48 to 72 hours. Treatment is then followed by oral administration during 4 to 6 weeks. This drug management must be combined with surgical drain procedures. Surgical treatment purpose is twofold: harvesting culture material and removal of infected, necrotic and poorly vascularized material.7,14,15
Marx15 suggest that in osteomyelitis cases, minimum antibiotic treatment should be 2 weeks. Nevertheless, Bamberger et al16 recommend a 4 week antibiotic course to achieve satisfactory evolution.
Treatment of osteomyelitis in chronic phase requires removal of involved teeth and bone sequestering achieved through wide resection, thus preventing infection dissemination and bone loss.7
Saucerization implies freeing the upper cortical section to expose medullar cavity and debride necrotic tissue; which is useful in chronic phases.
Decortication implies removal of infected bone cortex. This promotes resolution since the procedure removes non-vascular tissues and surrounding microorganisms.
Resection with reconstruction, be it immediate or secondary, is useful for low degree or refractory stages.7 In the present case, a subtotal hemi-maxillectomy was performed following Cordeiro et al s classification17 (Table II), which includes 3-5 walls including the palate.
Lentrodt et al10 point out that hyperbaric oxygen therapy is an adjuvant in osteomyelitis therapy since it elicits tissue hyper-oxygenation effect, antimicrobial activity, fibroblast proliferation, neo-vascularization, bone matrix formation increase, mineralization increase, as well as osteoblastic function improvement. Lentrodt & al10 observe a protocol of 60 to 90 minute daily sessions with 100% oxygen at 2.2 and 2.4 ATM pressure during at least 15 days.
CONCLUSION
Several therapies are described for osteomyelitis treatment. They range from simple antibiotic treatment up to wide resections, and combination of both. In theses series of cases, it was primarily decided to achieve systemic stability, to be later followed by antibiotic therapy prior to surgical treatment. Antibiotic agents used were: Clindamycin, 600 mg IV, every 8 hours and Ceftriaxone, 1 g IV every 12 hours. Encompassing surgical treatment implied performing subtotal hemi-maxillectomy to remove the lesion, followed by a prolonged post-surgical specific pharmacologic treatment with Procaine G Penicillin in treated cases. We hereby conclude that timely treatment of this disease is paramount, and this must be based upon specific diagnosis and pharmacological and surgical treatment so as to guarantee total removal of the lesion.
REFERENCES
1. Harvey B, Ephros H, DeFalco R. Tetracycline bone labeling in surgical management of chronic osteomyelitis: a case report. J Oral and Maxillofac Surg 2004; 62 (6): 752-754. [ Links ]
2. Eyrich G, Baltensperger M, Bruder E, Graetz K. Primary chronic osteomyelitis in childhood and adolescence: A retrospective analysis of 11 cases and review of the literature. J Oral and Maxillofac Surg 2003; 61 (5): 561-573. [ Links ]
3. Marx R, Stern D. Oral and maxillofacial pathology . A rationale of diagnosis and treatment, 1st Ed. Quintessence. 2003. [ Links ]
4. Barry C, Ryan L, Stassen. Osteomyelitis of the maxilla secondary to osteopetrosis: A report of 2 cases in sisters. J Oral Maxillofac Surg 2007; 65 (1): 144-147. [ Links ]
5. Cotran R, Kumar V, Collins T. Robbins patología estructural y functional . 6ta ed. McGraw-Hill Interamericana. 2002. [ Links ]
6. Regezi J, Sciubba J. Patología bucal . Correlaciones clinicopatológicas, 3a ed. Mc Graw-Hill Interamericana. 2007. [ Links ]
7. Topazian R, Goldberg M, Huup J. Oral and maxillofacial infections , 4th ed. W.B. Saunders. 2002. [ Links ]
8. Neville B, Damm D, Allen C, Bouquot J. Oral and maxillofacial pathology . 3rd ed. Elseviere. 2002. [ Links ]
9. Brodie BC. An account of some cases of chronic abscess of the tibia. Med Chir Trans 1832; 17: 239-249. [ Links ]
10. Lentrodt S, Lentrodt J, Kübler N, Mödder U. Hyperbaric oxygen for adjuvant therapy for chronically recurrent mandibular osteomyelitis in childhood and adolescence. J Oral Maxillofac Surg 2007; 65: 186-191. [ Links ]
11. Dich VQ, Nelson JD, Haltalin KC. Osteomyelitis in infants and children. A review of 163 cases. Am J Dis Child 1975; 129: 1273-1278. [ Links ]
12. Marx R. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: A growing epidemic. J Oral Maxillofac Surg 2003; 61: 1115. [ Links ]
13. Achar M. Acute osteomyelitis of the superior maxilla in an infant. AMA Arch Otolaryngol 1957; 66 (3): 248-256. [ Links ]
14. Lew D, Waldvogel F. Osteomyelitis. N Engl J Med 1997; 336: 999. [ Links ]
15. Marx R. Chronic osteomyelitis of the jaws. En: Laskin D, Strass R, eds Oral and Maxillofacial surgery clinics of North America . Philadelphia: Saunders 1992: 335-366. [ Links ]
16. Bamberger D. Osteomyelitis. A commonsense approach to antibiotic and surgical treatment. Postgrad Med 1993; 94: 177-182. [ Links ]
17. Cordeiro P, Disa J. Challenge in midface reconstruction. Semin Surg Oncol 2000; 19: 218-225. [ Links ] Note  Mailing Address:
Mailing Address:
Alberto Wintergest
E-mail: agerst@hotmail.com
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam











 texto en
texto en 


