Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista odontológica mexicana
versión impresa ISSN 1870-199X
Rev. Odont. Mex vol.15 no.2 Ciudad de México abr./jun. 2011
Case report
Hybrid prostheses in total maxillectomy
José Federico Torres Teran,* René Jiménez Castillo,§ Rubén Bernal ArciniegaII
* Maxillofacial Prostheses Speciality student, National University of Mexico.
§ Coordinator of the Maxillofacial Prostheses at the National University of Mexico.
II Professor of Oral Prostheses, at the Graduate Department of the National University of Mexico.
ABSTRACT
Maxillectomies triggered by cancer lesions leave as sequels the communication between oral and nasal cavities. This allows for the exchange of oral and nasal fluids which hinders speech, mastication and deglutition (swallowing) It also causes facial deformities which lower the patient's self esteem. To restore these functions, we need unconventional, modified, and hard to build prosthetic devices such as the design of a hybrid retention prosthetic obturator (swing lock).
Key words: Maxillectomy, prosthetic obturator, swing lock, hybrid prostheses.
Introduction
Head and neck cancer accounts for 17% of all cancer cases. It affects physical structures of the face and oral cavity. It leaves oroantral and oronasal communications as well as communication with the outside. This affects functions like swallowing, phonation, breathing and aesthetics. It also affects the individual's quality of life. In rehabilitation, there are surgical limitations in which the only viable option is a prosthesis.1-4
Maxillofacial prosthesis is the basic branch of dentistry dealing with the rehabilitation through artificial means of congenital or acquired defects of mouth and face affecting function and aesthetics.1,5
Obturators belong to the hybrid prosthesis type. This term is used for non conventional, mixed composition designs,6 which are functional for the rehabilitation of partial defects or total loss of the jaws. These devices are manufactured to re-establish mastication, phonation, deglutition and aesthetics.7
Treatment plans and the design principles for a partial removable prosthesis (PRP) are devised bearing in mind the morphology and classification of the defect.8,9
The design has to first consider the state of the periodontium and the remaining teeth. The design must also consider the design and access retention to the defect, the oral opening and the change experienced by soft tissues, both inside and outside of the mouth.
Other factors of the treatment plan besides the patient's motivation, must consider the following: age of the patient, general health state, tumour prognosis, and functional and aesthetic requirements. All these factors will determine the treatment plan of the final PRP.7
AJ Ackerman described in 1955 the swing lock prosthesis. This was also described at later dates by Simmons, 1963, Brown, 1970, Sprigg, 1977, and Armany.10
The use of the design and construction of these frameworks has been studied by many authors.11,12 Some of them do not agree and have discarded the use of these designs.13 Swing lock design incorporates conventional and special design hinge retainers in the same structure. Gate retainers are not the only retention source for prosthesis. Conventional retainers are used on posterior teeth, and with few exceptions, in anterior teeth as well. Hinge retainers are placed in anterior teeth and sometimes in posterior teeth. In distal location, generally we find space in the tooth next to the defect where we can place the lock or hinge of the gate.8 One of the advantages of these designs is the use of multiple serrations to evenly distribute retention tension. This helps to maintain and stabilize the prosthesis against vertical displacement. It is achieved with a bar going from labial to oral, this bar is attached to a larger conventional connector. The bar's design consists in vertical projection small retainers shaped as a I, Y, T and half T. These make contact on labial or lingual surfaces on the equator of the teeth. Low labial vestibules, high frenums and high smile lines are considered contraindications when designing the hinge. This design is not recommended for patients with deficient vision, poor manual dexterity or for those who rate aesthetics to a high degree.14,15
METHOD
Clinical case presentation
The patient is a 47 year old male, born and residing in Mexico City. He is single, catholic, merchant. The patient did no middle university education. Family history reveals a paternal grandfather deceased because of bronchogenic cancer.
Non pathological personal history (NPPH) reveals that the patient smokes and drinks alcohol. Condition: the patient first experiments the condition five years ago, after a right, upper third molar extraction. He experiences pain and feels a tumour in this site. He underwent a surgical hemimaxillectomy. The histopathological (HPR) report revealed a grade two chondrosarcoma.
Supporting treatment is begun. A course of 70 Gys radiotherapy is initiated, after which the patient suffered a relapse. Four lines of chemotherapy are then applied, the patient was unresponsive. A total maxillectomy is then carried out with the rebuilding of the orbits floor. The patient is monitored. By 2005 the patient presents tumoral activity (TA) with exophthalmous and chondrosarcoma HPR. The patient is then prepared for orbital exenteration and resection of the lesion. The lesion expands towards the right posterior lateral part of the skull. In July 2006 the patient arrives at the Maxillofacial Prosthesis Department of the Graduate School, School of Dentistry, National University of Mexico. Physical exploration revealed the following, the patient is calm, conscious, self-sufficient, well oriented, hydrated, with no visible pallor , with no lymphadenopathies, no metastasis, a wide facial defect communicating the oral cavity with the outside, he also presents an unimpeded oro-nasal communication, fistula of nose and skin, maxillectomy scar with irregular borders, irritation oedema and bleeding due to a provisional, unstable, irregular and porous prosthesis lacking retention, which is discoloured and with foul smell. The patient has teeth, the majority of which are in good condition (Figure 1).

All these reasons lead us to decide on the manufacture of an oral prosthesis.
To be able to build a permanent obturator we need to consider the following aspects: support surface, retentions, gaps, number of teeth, position, size of crown and root. After assessing these aspects, we decide to build a swing lock hybrid obturator prosthesis. The construction of this type of prosthesis requires the following.
Primary impression of dental arches, including the defect. These are conventional impressions; the only variable is the application of gauzes to cover the exposed nasopharyngeal communication. These impressions are cast in type III plaster. Once obtained the model, we analyze it, and individual impression trays are blocked and manufactured. For the physiologic impression taking.
Dental requirements: manufacturing of occlusal niches and interdental grooves. We must also eliminate possible retention and dental angles which could hinder insertion. We take impressions and obtain the physiological model with conventional techniques and materials. Once we achieve the physiological model we block it and duplicate it twice with a phosphate lining, which has been dehydrated and hardened in well known laboratories. In the first model, we wax a partial palatine plaque as major connector with its elements. We then take the model to the parallelometer to insert a tube where we will place the hinge (female section), exactly on the posterior gap. We will also insert a bar, for the closing component on the anterior defect. We must have sufficient depth in the oral groove to allow the placement of these devices. Once we lineally achieve this, we place cast connectors, we line them, we cast them, we recuperate them, we adjust them and we polish them.
This structure is placed in the second duplicated model, and we assess whether it is its properly settled. It is fixed on the grid with a coating, and a fine coating is applied with a brush to the rest of the structure. We then start modelling the rest of the hinge (male component) and the closing clasp. The gate must be pear shaped, broad and thick towards the free gingival margin. Vestibular depth must be at least 7 to 8 mm from the gingival margin. The bases of retainers in front teeth are placed at the same level to minimize forces. Retainers must be narrow, placed at a minimum of 0.25 mm from the labial equator of the tooth. They must be centered in the gingival third at the same level than the reciprocal component. We detail and rectify the waxing, we place the cast connectors, we coat it, we cast it, we recover it, we polish it, we remove it, and we adjust the gate with the rest of its components. We check the opening and closing of the gate (Figure 2).

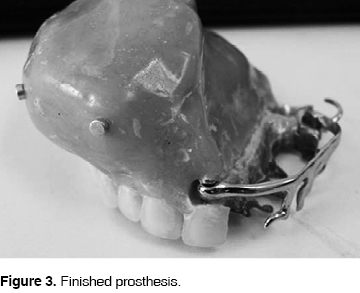
We try the device on the patient and we begin the conformation of the record base. With physiological means like deglutition and phonation we confirm the depth of the palate. We proceed then to place rods. We record craniomandibular relations. We place the model on the articulator and then adjust it. We select and articulate teeth. We carry out a final occlusion test, where we initiate bulb physiological rectification and conformation. We achieve this by placing soft modelling composition on the surface next to the defect until we reach the zones of interest. This is done to seal, give volume and provide the necessary retentions required by the defect. We trim the elongated, sharpened extensions and the areas of greater pressure. Especially in these modifications we apply polisulphide rubber and we bring the device to its position. We ask the patient to reproduce movements of opening, closing, lateral movements, deglutition, gesticulation, as well as phonetic maneuver, so we can rectify and seal the spaces reproduced by these movements. In a period of three minutes. After this period we wait for another six minutes with no movements. We withdraw the device from the mouth and we directly muffle the rectified zone, we sink it in the plaster, we retouch the waxing, we place it against the muffle, we remove the wax once the plaster hardens and finally we apply acrylic. After this we recuperate it, we trim it, and we clean it. At this point we hollow it and seal the bulb to be able to finish polishing (Figure 3).
We proceed to insertion. After this procedure the patient showed a good oral-nasal barrier, with its corresponding and evident change in aesthetics, phonation, deglutition mastication and self-esteem (Figure 4).

After building the obturating prosthesis, we can proceed to manufacture the facial prosthesis to finish full prosthetic rehabilitation.
DISCUSSION
Post surgical defects leave sequels that can compromise the patient's mastication, phonation, deglutition, aesthetics and self esteem. Since there is no oronasal barrier, the patient is predisposed to utter a nasal speech, and experiment an exchange of fluids between oral and nasal cavities, which alter chewing, and causing in some cases aesthetic deformations. With the prosthetic obturator we immediately minimize or eliminate the oral problem. Using the prosthesis of hybrid retention, the obturator provides sufficient retention and stabilization.
CONCLUSIONS
When all technicalities of all stages of treatment are observed, we can achieve a successful prosthetic rehabilitation. Using knowledge, will and determination we will achieve a better design for the prosthetic obturator, providing therefore a better quality of life for the patient.
REFERENCES
 Address correspondence:
Address correspondence:
José Federico Torres Terán
Clínica de Prótesis Maxilofacial de la
División de Estudios de Postgrado e
Investigación de la Facultad de Odontología, UNAM
E-mail: renejimenez@gmail.com
Note
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam
1. Beumer III J et al. Maxillofacial rehabilitation, prosthodontic and surgical considerations. Ishiyaku EuroAmerica Inc 1996. [ Links ]
2. Instituto Nacional de Cancerología. Manual de Oncología . Procedimientos medicoquirúrgicos. Mc Graw-Hill. México, D. F. 2da. Edición 2003: 259-271. [ Links ]
3. Leanne MS, Johan FW, Ashwin S. Prosthodontic rehabilitation of a patient with total avulsion of the maxilla: A clinical report. J Prosthet Dent 2002; 88: 362-6. [ Links ]
4. Jack WM, John RA, Mark SC, James CL. Postoperative care of the maxillectomy patient. Orl – head and neck nursing 1994; 12: 3.
5. Trigo JC, Trigo GC. Prótesis restauratriz maxilofacial . Argentina 1987. [ Links ]
6. The Academy of Prosthodontics. The Glossary of Prosthodontic Terms. The Journal of Prosthetic Dentistry 1999; 81 (1): 76. [ Links ]
7. Marunick M. Hybrid gate design frameworks for the rehabilitation of the maxillectomy patient. The Journal of Prosthetic Dentistry 2004; 91: 315-318. [ Links ]
8. Mohamed AA. Basic principles of obturator design for partially edentulous patients. Part I: Classification. J. Prosthet Dent 1978; 40: 554-7. [ Links ]
9. Mohamed AA. Basic principles of obturator design for partially edentulous patients. Part II: Design principles. J. Prosthet Dent 1978; 40: 656-62. [ Links ]
10. Ackerman AJ. The prosthetic management of oral and facial defects following cancer surgery. J Prosthet Dent 1955; 5: 413-32. [ Links ]
11. Simmons JJ. Swing-lock stabilization and retention. Tex Dent J 1963; 81: 10-2. [ Links ]
12. Parr GR, Gardner LK. Sing-lock design considerations for obturator frameworks. J Prosthet Dent 1995; 74: 503-11. [ Links ]
13. Elin S, Glenn EM, Sandra lR. Incorporation of an ERA attachment for obturator framework design: A clinical report. J Prosthet Dent 2002; 87: 477-80. [ Links ]
14. Schwartzman B, Caputo A, Beumer J. Occlusal force transfer by removable partial denture designs for a radical maxillectomy. J Prosthet Dent 1985; 54: 397-403. [ Links ]
15. Padilla MT, Campagni WV. The swing-lock removable partial denture. J Calif Dent Assoc 1997; 25: 387-92. [ Links ]











 texto en
texto en 


