Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Revista odontológica mexicana
versión impresa ISSN 1870-199X
Rev. Odont. Mex vol.15 no.2 Ciudad de México abr./jun. 2011
Original research
Handicapping malocclusions with a potential to deteriorate, an index proposal and its application
Ricardo Elizondo Dueñaz,* Manuel Yudovich Burak,§ M Aguilar Saavedra,II Arcelia Melendez Ocampo¶
* 3rd year student, Orthodontics Department, General Hospital "Dr. Manuel Gea Gonzalez".
§ Head Orthodontics Department, General Hospital "Dr. Manuel Gea Gonzalez".
II Professor, Orthodontics Department, General Hospital "Dr. Manuel Gea Gonzalez".
¶ Professor of Preventive Dentistry and Public Health, School of Dentistry, National University of Mexico.
ABSTRACT
The Public Health Sector need to select patients requiring orthodontic treatment at the 2nd and 3rd hospital level has led several authors to devise indexes to determine occlusal problems of non dental origin. However, none of these indexes can reliably measure the need in patients with cranial, facial and dental anomalies, which, at institutional level are a priority due to their transcendence, impact, magnitude and severity. For the purpose of this study we determined the most frequent cranial, facial and dental alterations in patients receiving treatment at the Orthodontics Department of the General Hospital "Dr Manuel Gea González" in 1996. A format was devised incorporating new variables. Each variable had nominal and ordinal values, so that their final addition would suggest the level of possibility and need for hospital based orthodontic treatment. This format was named "Index for handicapping malocclusions with a potential to deteriorate" (Índice de Maloclusiones Invalidantes con Potencial de Deterioro IMICPDD). It was applied to 80 patients who came to the hospital for treatment. Using the classification and the points system proposed, the lowest score was given to a totally edentulous female, patient with dysfunction while the highest score was for a female patient with a diagnosis of multiple facial fissures. The patient with multiple fissures would deserve a program of hospital administered orthodontic treatment while the edentulous one would not receive this service.
Key words: Occlusal indexes, handicapping malocclusions, potential to deteriorate, craniofacialdental anomalies, oral health areas.
INTRODUCTION
Indexes are useful tools to determine and measure disease. They describe a relative situation of health or illness in a given population through a graduated scale with well defined upper and lower margins, which can also include qualitative information, thus, they can indicate the degree of severity.1-3
Many research efforts in several oral health areas have been made in a search to obtain reliable and orderly information for the pathological dental or handicapping conditions. An example of this would be Kleins scale for the determination of caries prevalence CPO. This instrument has been internationally validated by health regulating institutions like the World Health Organization WHO, and the Public Health Organization PHO.4,5
Dental occlusion is a scheme hard to classify since it is the recipient of muscular and squeletal influences.6-8 Some classifications like Angle's9 have been made and some other indexes have been devised to determine the need for orthodontic treatment. These indexes are widely used in countries like the USA and Northern Europe where access to orthodontic public treatment has to be determined,10-12 other indexes are also used to evaluate the effectiveness of orthodontic treatment.13 When dealing with cranial, facial and dental alterations, there are classification, such as Samuel Pruzansky's, to determine microsomic lower jaws, and Paul Tessier's for facial fissures, as well as many others in the bibliographic references mentioned in this paper.14-20
When dealing with malocclusions that require a different approach, and additional treatment from the usual ones administered in clinical orthodontics, Yudovich since 1978 uses the term Handicapping Malocclusion with a Potential to Deteriorate , in reference to patients with any type of cranial, facial and dental anomaly with dental, muscular or squeletal disorders, or any combination of these, and a degree of handicap. This means any type of limitation to carry on functional, physical, mental, occupational or social activity, and who show a potential to deteriorate , defined in the manual guidelines of the Orthodontics Department of the General Hospital Dr. Manuel Gea Gonzalez as "the possibility that the alteration has to develop to a greater degree of handicap than the one involved at the time, tending to become, at its maximum expression, an irreversible situation".21-23 Since we deem them important we include in our study malocclusions found in cranial, dental and facial alterations, which can be of a congenital or acquired origin. Some of these alterations are cleft lip or palate, hemifacial microsomia, Crouzon and Apert syndromes, prognathisms, traumatisms, burn sequels, pathologies, etc.24-27
In 1960, Draker published a preliminary report of Handicapping Labio-Lingual Deviations HLD, where 9 conditions are classified (seven dental conditons, one condition specific to cleft palate, and one condition for traumatic deviations (such as loss of the premaxilla, osteomyelitis, etc). The presence of any of these conditions, regardless of their severity or extension, is sufficient to include the patient in the treatment program.28
Grainger published in 1967 the Orthodontic Treatment Priority Index which we will call TPI. This research is based upon the study of the interrelations of ten malocclussion manifestations observed in 375 12 year old patients who had not received any previous orthodontic treatment. This index gives priority to patients with facial fissures and accepts them immediately29 This index was later reassessed by Slakter at al., who incorporated psychosocial variables into it.30
In 1968, Saltzman proposed a more comprehensive way to assess handicapping malocclusions, The Priority of Malocclusion Index , PMI, with a format of 72 boxes, divided in three sections: intra arch deviations, inter arch deviations and posterior segments. It also includes a supplementary form, which, according to their instructions, has to be filled at a later stage. The evaluation is made directly in the patient's mouth. In this section, 8 points are granted for each of the following deviations found:31,32
• Facial and oral fissures
• Lower lip encompassing of upper incisor
• Occlusal interference
• Limitation of mandibular function
• Facial asymmetry
• Speech impediments
Based on Grainger's Estimate of Malocclusion Severity and Treatment Priority Index, Chester J. Summers published in 1971 the Occlusal Index OI, which, based on dental parameters only, evaluates nine characteristics of occlusion.33
Years later, in 1981, Kinaan proposed Quantitative assessment of the occlusal features, in which the only variables considered are of dental origin, this method requires special gauges modified by him.34
In 1984 in the article Indices cuantitativos para determinar la anomalía ortodoncica y evaluar su necesidad y prioridad de tratamiento (Quantitative indexes to determine orthodontic anomaly and assessment for the need and priority of treatment) , Tenenbaum, Morales and Goto published a format in which dental values are assessed. In this format priority is given to all genetic, congenital, functional and traumatic alterations.35
In the same year, Yudovich contributed with guidelines on Diagnóstico y manejo ortodóncico de condiciones invalidantes dentofaciales (Diagnosis and orthodontic handling of dentofacial handicapping conditions). Here, the dental, squeletal functional, genetic, traumatic, family background and geographic location aspects of the patients were considered. From this a format was generated, called Indice de Maloclusiones Invalidantes con Potencial de Deterioro, IMICPDD (Index for Handicapping Maloclusions with a Potential to Deteriorate), this format is presently used at the Department of Orthodontics and Stomatology at the General Hospital Dr. Manuel Gea González.22
Another index known as IOTN (Index of orthodontic treatment need) was developed in the United Kingdom. This index is divided into clinical and aesthetical components; the clinical component assesses purely dental malocclusion requirements into five degrees. The aesthetical component assesses maloclusion based on 10 color frontal occlusion photographs to illustrate different levels of dental aesthetics.36
Many authors have later used this index and have applied it to different population segments.37-39
In 1992 the European Journal of Orthodontics published the Peer Assessment Rating Index , PAR. This is a British index divided into eleven components obtained from study models.40
In 1992, in the same Journal, 4 of the 6 authors responsible for the PAR Index publish an article in which they present this index as an instrument to objectively measure improvement in orthodontic treatments.41
The PAR index was validated in 1995. It can be concluded that this index is a valid instrument to determine the severity and difficulty of a malocclusion treatment, and that it can be used to appraise dental oclusal changes, as published by Richmond et al. previously.42 Green and O Brien of the University of Manchester realized the importance of measuring malocclusions. They studied the influence of establishing "limit points" into the indexes, so as to give them greater validity. They published their results in 1994. In this article they also emphasize the point that, to this date, none of the indexes took into account the factor of self-esteem. Self esteem is a very relevant factor and is described in different publications. We suggest the ones we studied to develop the proposed index in this study.30,43-56
Yudovich in several dissertations has considered the importance of mentioning the limitations created by psychological factors. This is one of the criteria used to evaluate when to accept patients at the Orthodontics Clinic of the General Hospital Dr. Manuel Gea Gonzalez.21,23
The Probability Index (Índice de Probabilidad) was published in 1 995. This index specifically classifies the degree of severity of Class II malocclusions and it does so by adding up values to 5 cranial and dental angles.57
There is another index called Índice de Estética Dental (Dental Aesthetic Index) DAI, which, in 1996 was compared to the IOTN. Apparently, they are both quite similar since both consider aesthetic and clinical criteria. Notwithstanding, Joanna Jenny, in this article, reaches the conclusion that they are quite different when one considers their development method, sensitivity, reliability, validity and their ability to sort priorities in orthodontics treatment.58
In other publications we found that in the USA, the states of California and Maryland have each made their own modifications to the HLD index. This produces two new indexes the HLD (CalMod)53 and the HLD (Md). Many articles have been later published in an effort to rate and compare their application.59-63
In 1998, the American Orthodontics Board designed the American Board of Orthdodontics Index , The purpose of this index is to assess dental alignment based on panoramic X rays and plaster study models of orthodontically treated cases.64
Incidentally, this index was used by Abei et al in 2004 with the purpose of comparing occlusal results gathered by specialists in orthodontics and general practitioners in Ohio. They found that cases treated by specialists obtained a significantly lower score than those treated by general practitioners.65
From another author comes the Índice de Complejidad y Éxito y Necesidad de Tratamiento (Index of complexity, outcome and need) ICON. In this index several factors are considered: the aesthetical components of the need of orthodontic treatment index, crossbite, crowding, or spacing in the maxilla, overbite, or open bite, and the relation of the anteroposterior oral segment to determine the need, success, complexity and degree of improvement of the orthodontic treatment.66
In September 2001, Eung-Know Pae et al. published an article where they reach the conclusion that the lateral X rays of the skull are important to determine the severity of some types of orthodontic malocclusions.67
In the same volume, Seppo Järvinen from Finland, describes some indexes for the need of orthodontics treatment and their uses in everyday practice. They show that the primary purpose of these indexes is to measure the priority for treatment, that is, to select which patients are to receive treatment and to give them preference according to the score, until all children have been treated.13
In 2003, the Programa de monitoreo de éxito clínico (clinical outcome monitoring program) COMP was published This program consists in a software which allows the user to take data from the PAR, ICON, and the IOTN so as to evaluate more accurately results after an orthodontic treatment.68
Based on this revision, one can conclude that, to this day, there are no specific indexes to reliably measure cranial, facial and dental anomalies. These anomalies are considered a priority at institutional level for several reasons:
a) They are handicapping (transcendence),
b) The number of patients afflicted by them in any given geographical area (magnitude) and specific groups (risk),
c) The stage in their natural longitudinal history when no timely treatment has been provided (severity).
If we consider the role of the orthodontic caregiver within the scope of the multidisciplinary team dedicated to the treatment of cranial, dental and facial anomalies, we can determine, that the orthodontist is the person who combines knowledge on growth and development and the ability to influence them with orthopedic devices.69-77,79 He can also achieve occlusion with orthodontic treatment and thus the stability required for orthognatic surgical procedures (segmental, upper and lower jaw advancement, etc), and cranial and facial surgical procedures such as block advancements.78,79 We undertook in this research the task of designing and applying the MICPDD index to detect and assess handicapping malocclusions with a potential to deteriorate, of the different cranial and dental anomalies. It is important to assess the disability level degree and the deterioration potential of the anomalies with the help of an index which can:
• Be used to unify and to determine the criteria of the severity, its transcendence (social and economic) and the degree of these malocclusions.
• To allow the fair distribution of human, physical and material resources of the institutions targeted to provide treatment to these type of patients.
• To establish a sound parameter for the development of Public Health Government Programs.
• To establish formal research lines in material resources in those therapies provided in these institutions.
In order to provide an example of the aforementioned, we show three photographs of children afflicted with unilateral cleft lip and palate. The three cases have similar diagnosis and encompass a similar age group. If we were in a position of only being able to provide care for one of these cases at institutional level, the MICPDD could help us make a more objective decision (Figure 1A and 1B).

METHODS
In this index design, the research is a descriptive, observational retrospective and transverse study and in regard to its application it is descriptive, observational prospective and transverse.
In 1996, one of the investigators obtained a random sample of 50 questionnaires submitted to patients seeking treatment at the Orthodontics Department of the General Hospital "Dr. Manuel Gea Gonzalez" (Table A). The craniofacial characteristics of the patients were described, as a posterior crossbite of skeletal origin, normally found in plagiocephalies.80 The skeletal Class III cases, in which it is important to determine if they are the result of mandibular prognathism or a sequel of cleft lip and palate, etc. We built up a database according to the frequency of these ailments, in order to be able to make up an Index for Handicapping Malocclusions with a Potential to Deteriorate (MICPDD). In this study, we incorporated variables and punctuations, different scores to measure the number of structural alterations to determine the possibility and level of orthodontic care required, we also incorporated the necessary variables to include any malocclusion (dental, skeletal, muscular and/or functional). Each of these received ordinal and nominal values, so that the final values based on the score obtained could show, a direct relationship which suggests the level of probability and the need of hospital administered orthodontic treatment. Score values are based on relative complexity and/or the consequences they could have in the future, that is to say, the deterioration potential Figure 1A and 1B show the index structure.
We now present the variables included in this index and we explain the reasoning used to include them. We also present the scoring for each one of them.
On the upper left section there is a space slot with the word Registro ( registration) to insert the number or code given by the institution to the patient. At the center section there is a space for the date in which the index is filled out, and at the right section a larger box to insert the total obtained at the index, it has this size so that the index can be easily seen.
The next section starts with the patient's name, then the socioepidemiological information is required. This section only accounts for the geographical location of the patient. It gives two points if the patient can come to the institution to receive treatment for the required time, and zero points if the patient is unable to attend with the required frequency. This last point is important since it would limit the treatment that could be offered to the patient.
In the next segment we locate alterations. We start with functional alteration s, where one point is given in cases of speech alterations, two points are granted for chewing alterations three points for swallowing alterations and four points for respiratory and breathing alterations.
Image is another facet contemplated in this index. Image is an important factor of social development. Since we considered it a handicap, it received four points in each one of the affected areas. If a patient suffers rejection when applying for jobs or schools due to his image, this is considered a social handicap; we consider it family handicap in cases where the family itself or any of its members reject the patient and they relegate or hide him, or simply do not give him the same attention as his other siblings. We consider personal handicap those cases where self image of the patient is affected, regardless of whether we consider severe or not the alteration the patients shows.
In this index, the following alterations to consider are skeletal alterations . To be able to fill out this section, it is necessary to clinically appreciate whether there is any skeletal disharmony between upper and lower jaws, since , at the time we are filling this index (form) probably no radiographic studies are available. One point is given in cases of transversal alteration, two points are given for anteroposterior alterations, and three for vertical alterations. We granted this score, because we consider easier the correction of transversal problems and more difficult to correct vertical problems. Double points are given in cases when both upper and lower jaws are altered.
Temporomandibular dysfunction. In cases when temporomandibular joints are affected, one point will be given if there are sounds only when the physical exploration is carried out, two points if there are deviations, either on the opening or closing of the jaw, three in cases where pain is present, and four in cases when it is ankylosed. When patients arrive in pain, they are considered emergency cases, and are directly channelled to the treatment program, regardless of the score obtained in the index.
Periodontium. It is important in orthodontic treatments to have a healthy periodontium. In this item two points were given in cases where the periodontium is found in a favorable state, and zero points are given in cases where the periodontium is compromised. In this section we consider as compromised a periodontium which presents bleeding, gingival resorption and /or periodontal pockets, as well as in cases of 2nd or 3rd degree dental mobility (even if it is only in one tooth). We consider the periodontium as not affected in cases where it rates lesser scores than the ones we just mentioned, since it is possible that following periodontic treatment, conditions become favorable. If there is any doubt in this respect, it is recommended to discontinue the application of the index, send the patient to the periodontist, and re-evaluate him at a later date. The score given in this item is based on the contraindication to submit the patient to orthodontic treatment when he is suffering from /with an affected periodontium.
Traumatic alterations. In this index, we consider traumatic alterations those of skeletal origin and those alterations of soft tissue which have completed their process of regeneration and reparation respectively, otherwise they would be considered emergencies and should receive immediate attention. Fractures receive a three point score, regardless of whether the patient is a child or an adult.
When we found scars, these scored three points in cases where the patients growth stages were completed, and five points in cases where the patient was a child, since in these instances, the scars can deteriorate and affect during the growth process.
Genetic alterations. Five points are scored in these cases regardless of whether the alteration is the result of a malformation, deformation or disruption.
For this index, we tried to take into consideration the greatest possible amount of dental data. We place them in the MICPDD in the slot Occlusal Analysis ; we then have the following variables:
Dentition. Patients with deciduous dentition received one point. The rationale behind it is that they should receive fewer points since, at a given point in time, they can wait for treatment. We granted the intermediate score for patients with permanent dentition. Patients with mixed dentition scored three points, since in these cases growth peaks could probably be found, and these could be taken as an advantage during treatment.
Angle class or terminal plane. Angle Class I and flat terminal planes received a zero point score, since they are considered to be an ideal "occlusion", two points were granted to Class II terminal distal plane, and Class III and terminal mesial plane received three points, considering the greater complexity of solving a Class III. If the same type of occlusion appears on both sides, the score is double. If the sides have different occlusion, the scores are added up.
Dentoalveolar discrepancies. Each arch is considered independently. A millimetric calculation is made of the difference between available and required spaces. The upper arch receives one point when the discrepancy lies between 2 and 4 mm; two points are scored when the discrepancy lies between 4 and 6 mm, and three points are given for discrepancies of more than 6 mm. In the lower arch, the same rationale was used, where two, three and four points were respectively assigned, the rationale behind this is the difficulty and complexity of recovering space in the lower arch.
Dental compensations. As a means to compensate bone based disharmonic growth, teeth tend to assume positions. These positions can be excessive labial or lingual inclinations, or even rotations. Bearing this in mind, two points were assigned to inclinations and three for rotations, regardless of the compensated teeth. Rotated teeth received a higher score due to the difficulty they present to be corrected.
Ectopic teeth. In this index we consider a tooth to be ectopic when it is clearly located in a place other than its corresponding alveolus, and it is out of the arch. Teeth out of place were considered for their number, and not for their location. One point is granted in cases when only one ectopic tooth is present; two points are given for two ectopic teeth, and three points are given in cases when there are three or more teeth out of place.
Supernumeray teeth. As in other cases, if radiographic material is not available, only clinical findings are taken into consideration. One point is scored when there is one extra tooth, two points are scored for two extra teeth, and three points are scored when there are three or more extra teeth.
Absence of teeth. It is important to take into consideration the number of missing teeth, since missing teeth will limit the application of orthopedic and orthodontic devices. Bearing this in mind, the more teeth that were missing, the lesser score was obtained.
Independently of the origin of teeth absence (loss, previously indicated extractions, or agenesis), five points were assigned in cases when only one or two teeth were missing, four points if three or four teeth were missing, and only three points in cases where there were five or more missing teeth.
Impacted teeth. Third molars are not considered in this section. One point is given to one impacted tooth, two points are scored if there are two impacted teeth and three points are scored in cases where there are three or more impacted teeth. To fill the form it would be extremely useful to have a panoramic X ray. If this is not possible, then this section will not be taken into consideration.
Midline deviation. We have to be extremely careful when we assess the location of the midline. It is necessary to determine first whether the midline deviation is of dental and/or skeletal origin. We must also determine whether it is of the upper jaw, the lower jaw, or both. To achieve this we can use a segment of dental floss or wire. One point is given to cases where the deviation is entirely of dental origin, two points are given when the deviation is of skeletal origin, and three points are given when the deviation is due to both dental and skeletal origins. Double points are scored if both upper and lower jaws present this condition.
Open bite. Here we also have to be extremely careful. First of all we must record the presence of the open bite. We then must clinically determine whether the open bite is of dental and/or skeletal origin, and whether it is anterior and/or posterior. After this has been determined, we can proceed to measure the alteration with a millimetric tape. Ordinal values were assigned in the following fashion: one point is scored when the open bite measures between 1 and 3 mm, two points are scored if the open bite varies between 3.1 and 5 mm, three points are scored if the open bite varies between 5.1 and 7 mm, and four points are scored for open bites in excess of 7.1 mm.
Crossbite. Here we proceed in a similar fashion to the open bite cases. We first determine the presence of the open bite. Then we must record whether it is dental and/or skeletal. Punctuation is as follows.
One point if it is posterior, two points if it is anterior; two more points have to be added if it is merely of dental origin and four more points will be added if it is of skeletal origin. This was determined so, according to the case complexity. It is easier to correct a purely dental crossbite than a crossbite of skeletal origin.
Horizontal overbite. We must first determine whether it is a positive overbite (Class II cases) or negative overbite (Class III cases). Then we must assess the size of the overbite with a millimetric tape. Once this is done, we assign two points in cases when the overbite ranges between 2 and 4 mm, three points if the overbite ranges between 4.1 and 6 mm, and four points in cases where the overbite is 6.1 mm and higher
Vertical overbite. In this slot, we register the percentage in which the upper incisor covers the lower one, regardless of whether there is crossbite or not, since this has been already previously recorded. The percentile punctuation is as follows: one point in cases when one third to one half of the incisor is covered, two points in cases where one half to two thirds of the incisor are covered, and three points in cases where more than two thirds of the incisor are covered.
Once designed this method for the diagnosis of handicapping malocclusions with a deterioration potential we applied it to 80 cases who came for treatment to the Orthodontics Department. Through the application of this method we determined the frequency of need for orthodontic treatment.
ANALYSIS AND RESULTS
We present the results for every one of the variables recorded in the format, based on the analysis of proportions, and averages.
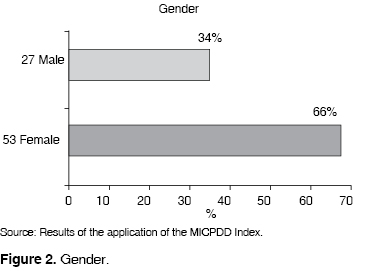
Gender
80 patients were surveyed. 27 were male (34%) and 53 female (66%) (Figure 2).
Geographic Location
75 (93%) out of the 80 patients, replied not having problems to attend on a regular basis their treatment appointments, while the other 5 (7%) mentioned difficulties to comply. It is important to mention that out of the 75, most of them lived in Mexico City, and in its outskirts in the State of Mexico, the others in neighboring states, 3 in Morelos, 1 in Hidalgo and 1 in Guerrero. All of them mentioned that according to their socioeconomic level chart prices they were willing to cover the expenses and could obtain the required work and studies leave permits to attend .Of the other 5, only one was from Mexico City and could not afford even the monthly transportation costs to the hospital (Figure 1A).
Functional alterations
From the total population to which the MICPDD was applied, 54% (43 patients) presented some type of functional alteration; 44% of these were speech alterations, 48% chewing alterations, 2% respiratory alterations and 5% belong to patients which presented functional alterations in more than one field (speech and chewing). None of the patients presented swallowing alterations. From the total number of patients presenting some type of functional alterations, 63% were female and 33% male. This shows that in this scope two females are affected per each male (Figure 3).
Image
38% of surveyed patients informed they are affected by one or several of these categories: 44% percent feel affected in their personal life, 12% in their family life, 38% in their social life, and 6% in all the aforementioned. Of all the patients, 60% of the females and 40% of the males felt affected in their image (Figure 4).
Skeletal alterations
65 of the surveyed patients presented some type of skeletal alteration; 61% suffered alterations of the upper jaw, 34% suffered alterations of the lower jaw, and 5% in both jaws. It is important to observe there are two patients with upper jaw alterations for each patient presenting lower jaw skeletal alterations (Figure 5).
Temporomandibular dysfunction
This variable was determined based on the presence of the following three indicators: articular sounds, deviations when opening or closing the jaws, and pain. 60% of the patients were affected by one or more of these indicators, either in isolation or combined. Of the body of patients, 5 reported pain with or without sounds and/or deviation, and they received immediate attention (Figure 6).
Periodontium
According to the parameters established in this study 10 cases (13%) presented a compromised periodontium (Figure 7).

Traumatic alterations By the time this study was carried out, of the 80 cases which came to the Orthodontics Department of the General Hospital Dr. Manuel Gea Gonzalez, only 3,(4%) presented some traumatic sequel. All these sequels were skeletal in nature and none of them presented soft tissue scarring (Figure 8).

Genetic alterations
These were present in 56% of the surveyed patients. According to the origin of the alterations these were classified into the following: Malformations (42% of patients) Deformations, (0%) and Disruption (58%) (Figure 9).
Dentition
The dentition types were distributed as follows: 11% deciduous dentition (9 cases); 18% mixed dentition (14 cases) and 71% (57 cases) permanent dentition (Figure 10).

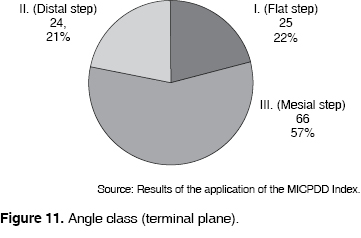
Angle class (Terminal Plane)
Class I and II Angle and/or distal and flat step were present in almost the same proportion (22 and 21% respectively) while Class III and or mesial step were present in 57% or the patients surveyed with this index (Figure 11).
Dentoalveolar discrepancy 66% of patients presented insufficient space in one or both arches. The percentile distribution is as follows: Upper arch 29% of cases, lower arch, 17% of cases, both arches, 54% of cases (Figure 12).
Dental compensations
Of the 80 surveyed patients, 60 presented dental compensations in different combinations of lingualization, labialization and rotation (Figure 13).

Ectopic teeth 20% of patients presented teeth out of location. Of this percentile value, 62 percent had one tooth out of place, 19% two teeth in this situation, and the 19% remaining had 3 or more displaced teeth (Figure 14).
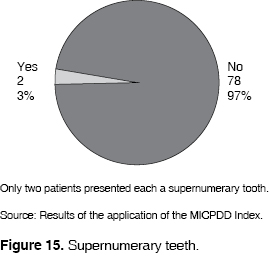
Supernumerary teeth
Only two patients (3%) presented each a supernumerary tooth (Figure 15).
Absence of teeth 55% of the surveyed cases presented absence of teeth; of these, 64% were missing one or two teeth, 14% were missing 3 to 4 teeth and 22% were missing 5 teeth or more (Figure 16).
Impacted teeth
No corroboration could be made in any of the cases of impacted teeth in the surveyed patients, for none of them presented radiographic studies that could provide evidence of their presence.
Midline deviation
When applying this index to surveyed cases, the following information could be gathered: 60 percent of cases presented this variable in any of its manifestations, according to their location, 21% were in the upper jaw, 28% in the lower jaw, and 51% in both jaws We also observed that 11% were of skeletal origin, 23% of dental origin, and 66% a combination of both (Figure 17).
Open bite
From the total surveyed cases open jaw prevalence represents 18%, 93% of the aforementioned percentile value is of skeletal origin and 7% of dental origin. As we can observe, it is easy to estimate the degree of severity, since the correction of skeletal open bite requires a higher financial investment and more complicated procedures when compared to open bite cases of dental origin (Figure 18).
Crossbite 40%of surveyed cases presented some type of crossbite. The higher percentage (37%) pertained to cases of skeletal anterior open bite (Figure 19).
Horizontal overbite
We found horizontal overbite was altered in 57 patients. This represents 71% of the total. 37 of these overbite cases were considered positive (65%) and 20 were diagnosed negative (35%) 60% of the negative overbites spanned between 2 and 4 mm, 15% from 4.1 to 6, and 25% 6.1 or more. We must mention that the 23 remaining patients (29%) are not included in the horizontal bite category, for they present border to border bite, an overjet of less than 2 mm or absence of anterior teeth. Of the 37 positive overbites, 70% are in the 2 to 4 mm group, 27% in the 4.1 to 6 mm group and 3 % in the 6.1 mm or more group. This last percentage is represented by one single patient who was diagnosed as suffering from protrusion of the maxilla (Figure 20).
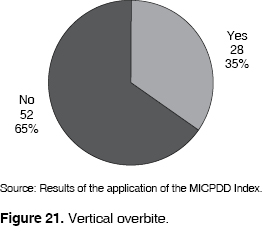
Vertical overbite
We recorded altered vertical overbite in 28 cases to which we applied the MICPDD (35%). From these cases, 9 patients (32%) the overbite present was in the range < 1/3 > 2/3, and in 5 patients (18%) it was < 2/3. In the remaining 50% (14 cases) of the patients vertical overbite was negative. This percentile values pertain to cases presented with open bite (Figure 21).
DISCUSSION
This paper aims at designing an index able to record and assign values to the characteristics of the patients affected by handicapping malocclusion with a potential to deteriorate. Social and demographic factors were not considered in any of the previous indexes, neither they contained variables and values as proposed in this study (MICPDD) for disorders of non dental origin. It is important to consider these factors since they determine the level of orthodontic treatment that can be offered to the patient. Malocclusions are often due to muscular and/or skeletal factors, which per force, make the treatment more complex. Another specifically important difference with the Draker HLD, Grainger and Tennebaum indexes, is that this study includes in the clinical attention program, facial fissures or other types of cranial, facial and some dental alterations. As well the Salzman's index, does not dwell in the degree of involvement and does not differentiate among types of craneofacial alterations. In the MICPDD they have higher or lower ordinal values according to the effect their presence could have in the dental health and in the stomatognathic function and facial appearance, and their application as a pilot test. These cases consider sequels and/or signs and symptoms present, there will be cases in which the fissure by its nature, or the previously received surgical or dental treatment warrants, immediate institutional attention, while in another case it can wait for treatment. There can even be cases in which required treatment doesn't have necessarily to be carried out at this level. To give an example, in figure 22 we show two cases of unilateral cleft lip and palate in two similar age patients. One of these patients, had received proper treatment since birth; the other received unskilled treatments. Here the images support the contention that not all cases of cleft lip and palate must be considered in institutional programs, at least, not be rated as urgent cases.

This index does not require sophisticated devices and instruments like in the indexes of PAR and Kinaan.
The index we propose here thoroughly assesses handicapping conditions. It differs from the previous existing Handicapping Malocclusion with a Potential to Deteriorate because it contains nominal and ordinal scales which allow the classification of malocclusion into low risk, middle risk and high risk, according to the degree of severity shown by the case. This enables us to distribute fairly according to priorities and need, hospital, institutional and clinical orthodontic treatment and services.
CONCLUSIONS
Results obtained in this research project allow us to assess clinical, social and demographic parameters which reflect occlusal conditions as regards to their different origins. They can predict the possibility of deterioration when observing the original state of the patient. It also determines the possibility and level of orthodontic care required. The patient with larger number of structural alterations received the highest punctuation while edentulous patients and those presenting purely dental malocclusion, according to the classification, do not necessarily require hospital or institutional based orthodontic treatment.
For comparison's sake it would be important to validate this instrument in a different population. This would allow it to be used to unify criteria and determine the severity, transcendence (social and economic) and magnitude of handicapping malocclusions requiring hospital based orthodontic treatment in government facilities and in institutions where all resources, physical, material or human have to be geared to those patients who are most in need o treatment.
REFERENCES
 Address correspondence:
Address correspondence:
Ricardo R. Elizondo Dueñaz MD
E-mail: drricardoelizondo@ortodonciamonterrey.com
Note
This article can be read in its full version in the following page: http://www.medigraphic.com/facultadodontologiaunam
1. Cuenca E. Manual de Odontología Preventiva y Comunitaria . Masson S.A., Barcelona, 1991. [ Links ]
2. Chávez M. Odontología Sanitaria . OMS-OPS, 1984. [ Links ]
3. Wilkins ME. Clinical practice of the dental hygienist. 6th Ed. 1981. [ Links ]
4. Klein H, Palmer CE, Knutson JW. Studies on dental caries. I. Dental status and dental needs of elementary school children. Pub Health Rep (Wash) 1938; 53: 751-65. [ Links ]
5. Organización Mundial de la Salud. Investigación de la Salud Oral Trillas, UNAM, 1990: 40-42. [ Links ]
6. Hellman M. Factors influencing occlusion. Angle Orthod 1942: XII(1). [ Links ]
7. Noyes HJ. Classification of malocclusion. Angle Orthod 1942: XII(1). [ Links ]
8. McNamara Jr. The biology of occlusal development. Monograph Number 7, Craniofacial Growth Series, Center for Human Growth and Development. The University of Michigan. Ann Arbor Michigan 1997: 89-111. [ Links ]
9. Angle. Treatment of malocclusion of the tooth. 1907. [ Links ]
10. Shaw WC, Richmond S, O'Brien KD. The use of occlusal indices: A european perspective. Am J Orthod Dentofacial Orthop 1995; 107: 1-10. [ Links ]
11. Järvinen S. Indexes for orthodontic treatment need. Am J Orthod Dentofacial Orthop 2001; 120: 237-9. [ Links ]
12. Han H, Davidson WM. A useful insight into 2 occlusal indexes: HLD (Md) and HLD (CalMod). Am J Orthod Dentofacial Orthop 2001; 120: 247-53. [ Links ]
13. Tang ELK, Wei SHY. Assessing treatment effectiveness or removable and fixed orthodontic appliances with the occlusal index. Am J Orthod Dentofacial Orthop 1990; 99: 550-6. [ Links ]
14. Pruzansky S. Not all Dwarfed mandibles are alike. Birth Defects 1(2): 120-129. [ Links ]
15. Vento AR, LaBrie RA, Mulliken JB. The OMENS classification of hemifacial microsomia. Cleft Palate J 1991; 28: 68-78. [ Links ]
16. Tessier P. Anatomical classification of facial, cranio-facial and clefts. J Maxillofac Surg 1976; 4: 69-92. [ Links ]
17. van der Meulen JC, Mazzola R, Vermey-Keers C. A morphological classification of craniofacial malformations. Plast Reconstr Surg 1983; 71 (4): 560-72. [ Links ]
18. Rodgers SF, Eppley BL, Nelson CL. Hemifacial microsomia: assessment of classification systems. J Craniofac Surg 1991; 2(3): 114-26. [ Links ]
19. Horgan JE, Padwa BL, LaBrie RA, Mulliken JB. OMENS-Plus: Analysis of craniofacial and extracraniofacial anomalies in hemifacial microsomia. Cleft Palate J 1995; 32 (5): 405-12. [ Links ]
20. Park S, Ock JJ. A new classification of palatal fracture and an algorithm to establish a treatment plan. Plast Reconstr Surg 2001; 107 (7): 1669-76. [ Links ]
21. Yudovich M. Criterio de aceptación de pacientes al Departamento de Ortodoncia del Hospital General "Dr. Manuel Gea González". Índice de maloclusiones invalidantes con potencial de deterioro y cuadros de información diagnóstica. Manual Interno del Dpto. de Ortodoncia, Hosp. Gral. Dr. Manuel Gea González ; México, D.F. 1978. [ Links ]
22. Yudovich M. Diagnóstico y manejo ortodóncico de condiciones invalidantes dentofaciales . 1984. [ Links ]
23. Yudovich M. Maloclusiones invalidantes con potencial de deterioro. Manual interno del Dpto. de Ortodoncia, Hosp. Gral. "Dr. Manuel Gea González" ; México, D.F. 1995. [ Links ]
24. Mutchinick O, Lisker R, Babinsky V. Programa Mexicano de "Registro y vigilancia epidemiológica de malformaciones congénitas externas". Salud Pública Mex 1988; 30: 88-100. [ Links ]
25. Cohen Jr MM, Kreiborg S. Birth prevalence studies of the Crouzon syndrome: comparison of direct and indirect methods. Clin Genet 1992; 41: 12-15. [ Links ]
26. Saavedra D, Torres M. Malformaciones congénitas de etiología multifactorial . Genética Clínica 2a Ed. Manual Moderno, México, 1994. [ Links ]
27. Yudovich M, Ramírez MG, Delgado G. Tratamiento ortopédico para la corrección vertical de la premaxila en niños preescolares con secuela de labio y paladar hendido bilateral. Rev Iberoamer de Ortod 1997; 16 (1): 18-24. [ Links ]
28. Draker HL. Handicapping labio-lingual deviations: a proposed index for public health purposes. Am J Orthod 1960; 46 (4): 295-305. [ Links ]
29. Grainger RM. Orthodontic treatment priority index . In: Public Health Service Publication No 1000, Series 2, No 25. Washington DC: US Government Printing Office; 1967. [ Links ]
30. Slakter MJ, Albino JE, Green LJ, Lewis EA. Validity of an orthodontic treatment priority index to measure need for treatment. Am J Orthod 1980; 78 (4): 421-25. [ Links ]
31. Salzmann JA. Handicapping malocclusion assessment to establish treatment priority. Am J Orthod 1968; 54 (10): 749-68. [ Links ]
32. Salzmann JA. Treatment priority index of malocclusion. Intern Dent J 1970; 20: 610-32. [ Links ]
33. Summers CJ. The oclusal index: a system for identifying and scoring occlusal disorders. Am J Orthod 1971; (6): 552-67. [ Links ]
34. Kinaan BK, Burke PH. Quantitative assessment of the occlusal features. Br J Orthod 1981; 8: 149-56. [ Links ]
35. Tenenbaum M, Morales M, Goto C. Índices cuantitativos para determinar la anomalía Ortodóncica y evaluar su necesidad y prioridad de tratamiento. Rev Iberoamer de Ortod 1984; 4 (1): 21-36. [ Links ]
36. Brook PH, Shaw WC. The development of an index of orthodontic treatment priority. Eur J Orthod 1989; 11: 309-20. [ Links ]
37. Üçüncü N, Ertugay E. The use of the index of orthodontic treatment need (IOTN) in a school population and referred population. J Orthod 2001; 28: 45-52. [ Links ]
38. Mattick CR, Gordon PH, Gillgrass TJ. Smile aesthetics and malocclusion in UK teenage magazines assessed using the index of orthodontic treatment need (IOTN). J Orthod 2004; 31: 17-19. [ Links ]
39. Kok YV, Mageson P, Harradine NWT, Sprod AJ. Comparing a quality of life measure and the aesthetic component of the index of orthodontic treatment need and concern. J Orthod 2004; 31: 312-18. [ Links ]
40. Richmond S, Shaw WC, O'Brien KD, Buchanan IB, Jones R, Stephens CD, Roberts CT, Andrews M. The development of the PAR index (peer assessment rating): reliability and validity. Eur J Ortod 1992; 14: 125-39. [ Links ]
41. Richmond S, Shaw WC, Roberts CT, Andrews M. The PAR index (peer assessment rating): methods to determine outcome of orthodontic treatment in terms of improvement and standards. Eur J Ortod 1992; 14: 180-87. [ Links ]
42. DeGuzman L. The validation of the peer assessment rating index for malocclusion severity and treatment difficultly. Am J Orthod Dentofac Orthop 1995; 107: 172-6. [ Links ]
43. Green J, O'Brien K. The influence of the setting of "cut-off" points for orthodontic treatment need upon the reliability of the index of orthodontic treatment need. Br J Orthod 1994; 21: 287-89. [ Links ]
44. Knorr JN, Hoopes JE. Psychiatric-surgical approach to adolescent disturbance in self image. Plast Reconstr Surg 1968; 41: 248-53. [ Links ]
45. Lefebvre A, Munro I. The role of psychiatry in a craniofacial team. Plast Reconstr Surg 1978; 61: 564-69. [ Links ]
46. Phillips J, Whitaker LA. The social effects of craniofacial deformity and its correction. Cleft Palate J 1979; 16: 7-15. [ Links ]
47. Pertschuk MJ, Whitaker LA. Psychosocial adjustment and craniofacial malformations in childhood. Plast Reconstr Surg 1985; 75(2): 177-184. [ Links ]
48. Harrison AM. Discussion of psychosocial adjustment and craniofacial malformations in childhood. Plast Reconstr Surg 1985; 75: 183-84. [ Links ]
49. Whitaker LA, Bartlett SP. The craniofacial Dysostoses: Guidelines for management of the symmetric and deformities. Clin Plast Surg 1987; 14: 73-81. [ Links ]
50. Pillemer FC, Cook KV. After surgery: the psychosocial adjustment of pediatric craniofacial patients. Cleft Palate J 1989; 26: 201-07. [ Links ]
51. Padwa BL, Evans CA, Pillemer FC. Psychosocial adjustment in children with hemifacial microsomia and other craniofacial deformities. Cleft Palate J 1991; 28 (4): 354-59. [ Links ]
52. Salier HF, Kolb E. Influence of craniofacial surgery on the social attitudes toward the malformed and their handling in different cultures and at different times: a contribution to social world history. J Craniofac Surg 1995; 6 (4): 314-26. [ Links ]
53. Mouradian WE. Who decides? Patients, or gatekeepers: pediatric decisions in the craniofacial setting. Cleft Palate J 1995; 32: 510-14. [ Links ]
54. Birkeland K. Orthodontic concern among 11-year-old children and their parents compared with orthodontic treatment need assessed by index of orthodontic treatment need. Am J Orthod Dentofac Orthop 1996; 110: 197-205. [ Links ]
55. Ravaglia C. Aspectos psico-clínicos para la atención odontológica de los pacientes con discapacidad. 22/09/2001 webodontologica.com [ Links ]
56. Motegi E et al. Health-related quality of life and psychosocial function 5 years after orthognathic surgery. Am J Orthod Dentofac Orthop 2003; 124: 138-43. [ Links ]
57. Gramling JF. The probability index. Am J Orthod Dentofac Orthop 1995; 107: 165-71. [ Links ]
58. Jenny J, Cons NC. Comparing and contrasting two orthodontic indices, the index of orthodontic treatment need and the dental aesthetic index. Am J Orthod Dentofac Orthop 1996; 110: 410-6. [ Links ]
59. Parker WS. The HLD (CalMod) index and the index question. Am J Orthod Dentofac Orthop 1998; 114: 134-41. [ Links ]
60. Parker WS. A study of 1,000 malocclusion selected by the HLD (CalMod) index. Am J Orthod Dentofac Orthop 1999; 115: 343-51. [ Links ]
61. Parker WS. Useful data from application of the HLD (CalMod) index. Short communication. Am J Orthod Dentofac Orthop 2000; 117: 435-37. [ Links ]
62. Beglin FM. A comparison of the reliability and validity of 3 occlusal indexes of orthodontic treatment need. Am J Orthod Dentofac Orthop 2001; 120: 240-6. [ Links ]
63. Han H, Davidson WM. A useful insight into 2 occlusal indexes: HLD(Md) and HLD(CalMod). Am J Orthod Dentofacial Orthop 2001; 120: 247-53. [ Links ]
64. Casko J, Vaden L, Kokich VG. American Board of Orthodontics: Objective grading system for dental casts and panoramic radiographs. Am J Orthod Dentofacial Orthop 1998; 114: 589-99. [ Links ]
65. Abei Y, Nelson S, Amberman B, Hans M. Comparing orthodontic treatment outcome between orthodontists and general dentists with the ABO index. Am J Orthod Dentofacial Orthop 2004; 126: 544-48. [ Links ]
66. Daniels C, Richmond S. The development of the index of complexity, outcome and need (ICON). Br J Orthod 2000; 27: 149-62. [ Links ]
67. Pae E. Role of lateral cephalograms in assessing severity and difficultly of orthodontic cases. Am J Orthod Dentofac Orthop 2001; 120: 254-62. [ Links ]
68. Weerakone S, Dhopatkar A. Clinical outcome monitoring program (COMP): a new application for use in orthodontic audits and research. Am J Orthod Dentofacial Orthop 2003; 123: 503-11. [ Links ]
69. Pruzansky S. The challenge and opportunity in craniofacial anomalies. Cleft Palate J 1971; 8: 239-50. [ Links ]
70. Ortíz-Monasterio F. La integración y el adiestramiento de un equipo multidisciplinario para cirugía craneofacial. Separata de La Prensa Médica Mexicana 1974; XXXIX: 183-88. [ Links ]
71. Vig KWL. Orthodontic considerations applied to craniofacial dysmorphology. Cleft Palate J 1990; 27: 141-45. [ Links ]
72. Parameters for evaluation and treatment of patients with cleft lip/palate or other craniofacial anomalies. Supplement to Cleft Palate Craniofacial J 1993; 30: S2-S15. [ Links ]
73. Moss ML. The functional matrix. In: Kraus B, Reidel R editors. Vistas in orthodontics . Philadelphia: Lea and Febiger, 1962:85-98. [ Links ]
74. Moss ML, Salentijn L. The primary role of the functional matrices in facial growth. Am J Orthod 1969; 55: 566-77. [ Links ]
75. Moss ML. The functional matrix hypothesis revisited. 1. Am J Orthod Dentofac Orthop 1997. [ Links ]
76. Moss ML. The functional matrix hypothesis revisited. 2. The role of an osseous connected cellular network. Am J Orthod Dentofac Orthop 1997; 112: 221-6. [ Links ]
77. Moss ML. The functional matrix hypothesis revisited. 3. The genomic thesis. Am J Orthod Dentofac Orthop 1997; 112: 338-42. [ Links ]
78. Epker BN, Stella JP, Fish LC. Dentofacial deformities . 2nd Ed. Mosby. 1995: I. [ Links ]
79. American Association of Orthodontists. Excerpts from American association of orthodontists clinical practice guidelines for orthodontics and dentofacial orthopedics 1996. Am J Orthod Dentofac Orthop 1996; 111: 443-449. [ Links ]











 texto en
texto en 


