Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
Migraciones internacionales
versión On-line ISSN 2594-0279versión impresa ISSN 1665-8906
Migr. Inter vol.2 no.4 Tijuana jul./dic. 2004
Artículos
The Unauthorized Residency Status Myth: Health Insurance Coverage and Medical Care Use among Mexican Immigrants in California
Enrico A. Marcelli *
* Harvard University
Fecha de recepción: 16 de junio de 2004
Fecha de aceptación: 25 de agosto de 2004
Abstract
Informed by recent developments in the behavioral model of medical care use and social epidemiology, this article employs survey data to estimate whether unauthorized residency status among non-elderly Mexican and other-Latino immigrant adults in California influenced the probability of having had health insurance and having received medical care. Unauthorized residency status is estimated to have decreased the probability of having been insured, and augmented the probability of having relied on public health insurance. However, after controlling for other individual characteristics, neighborhood context, and social capital, neither insurance nor residency status appears to have influenced whether a person obtained needed medical care. Rather, neighborhood context, difficulty locating a medical care facility, and civic engagement appear to be more important for understanding use of medical services.
Keywords: international migration, medical care, undocumented migrants, Mexico, United States.
Resumen
Tomando en cuenta los avances recientes en el modelo conductual del uso de asistencia médica y la epidemiología social, este artículo utiliza datos de encuestas para estimar si el estatus de residencia no autorizada entre los mexicanos que todavía no llegan a la vejez y otros inmigrantes latinos en California influyó en la probabilidad de que tuvieran seguro de salud y recibieran asistencia médica. se estima que el estatus de residencia no autorizada ha disminuido la probabilidad de que estuvieran asegurados y, a su vez, ha aumentado la de que recurrieran al seguro de salud pública. sin embargo, después de controlar otras características individuales, el contexto de vecindad y el capital social, ni el seguro ni el estatus de residencia parecen haber influido en que una persona obtuviera la asistencia médica necesaria. Finalmente, el contexto de vecindad, la dificultad para encontrar un lugar de asistencia médica y el compromiso cívico parecieran ser más importantes para comprender el uso de los servicios médicos.
Palabras clave: migración internacional, asistencia médica, migrantes indocumentados, México, Estados Unidos.
Political and Scholarly Context*
Public policy debate concerning unauthorized immigrants' use of publicly subsidized medical care and other public benefits during the past two decades has been accompanied by a paucity of statistically credible research on the subject.1 Proponents of California's November 1994 ballot initiative, Proposition 187, for instance, argued based almost exclusively on anecdotal evidence that providing subsidized medical care, education, and welfare to unauthorized immigrants was luring them north, draining state resources, and making it more difficult to serve other needy but authorized populations. Meanwhile, at the national level, the U.S. ("Barbara Jordan") Commission on Immigration Reform added labor market competition to the list of fiscal impact concerns, and recommended that Congress implement policy measures making it more difficult for unauthorized immigrants to enter and remain in the country (United States Commission on Immigration Reform, 1994).2 One result was the passage of the Personal Responsibility and Work Opportunity Act (PRWORA) and the Illegal Immigration Reform and Immigrant Responsibility Act (IIRIRA) in August and September 1996 (Fragomen, 1997). Together these laws and their amendments increased restrictions on access to public benefits available to authorized noncitizens residing in the United States and increased investments in personnel and technology to guard the border. By implication, unauthorized immigrants would begin to experience even greater difficulty obtaining public benefits than before the legislation went into effect in January 1997, partly due to heightened fears concerning possible detection and deportation, but also because states wishing to provide anything more than emergency care or immunizations were required to pass special eligibility laws or obtain permission from the U.S. attorney general (Berk et al, 2000; Kullgren, 2003). Before this legislation, of course, unauthorized immigrants had been ineligible for all entitlement programs except prenatal or emergency care and certain immunizations (Fragomen, 1997; Marcelli and Heer, 1998),3 and the immigrant health literature had long demonstrated a positive association between reductions in immigrant-minority entitlements and poor health outcomes (Riedel, 1998).
Skeptics of politicians' assessments of how noncitizens, and particularly unauthorized immigrants, were impacting the United States argued that medical care is a basic human right and that a more responsible, longer-term view would emphasize the negative fiscal and community health effects of not providing essential care to all U.S. residents regardless of residency status (Kullgren, 2003). Denying treatment to immigrants with communicable diseases, for example, could place U.S. citizens at risk, and as was anticipated (Stern, 2003), the debate concerning "universal" health insurance coverage became increasingly heated as the 2004 Bush-Kerry presidential election approached (Stevenson and Toner, 2004). Still, little is known about how many unauthorized immigrants are covered by a health insurance plan at any geographic level, about what proportion have publicly subsidized insurance, or about how many rely on public medical services.
Further obfuscating this relatively uninformed debate is the fact that existing studies are divided on whether unauthorized residency status influences health insurance coverage and medical care use. Ethnographic work and descriptive statistics generated from random data suggest that unauthorized residency status decreases the probability that a foreign-born person has health insurance or uses medical care (Berk et al., 2000; Brown et al., 1999; Brown et al., 2000; Brown and Yu, 2002; Capps et al, 2002; Chavez, 1986; Marcelli and Heer, 1998; Schur et al., 1999; Siddharthan and Ahern, 1996). The application of econometric techniques to random samples and controlling for other factors suggest no such influence, however (Halfon et al., 1997; Hubbell et al., 1991). Moreover, I know of no study that places the analysis of unauthorized immigrant insurance coverage or use of medical care within a firm theoretical context.
This article offers the first estimates of how individual characteristics, neighborhood environment, and socioeconomic factors influence health insurance coverage and medical care use among authorized and unauthorized Mexican immigrants in California. The work is conceptualized within the evolving behavioral or "health services" model of medical care use introduced in the 1960s, which emphasizes the influence of population characteristics, social and institutional context, and health behaviors (Aday, 1993; Aday and Andersen, 1974, 1975; Aday, Flemming, and Andersen, 1984; Andersen, 1968, 1995; Andersen and Davidson, 2001; Carillo et al., 2001; Institute of Medicine, 1993); and it employs a survey-based residency status estimation methodology, pioneered and developed by David Heer and colleagues in the 1980s and 1990s (Heer et al., 1992; Heer and Passel, 1987; Marcelli and Heer, 1997) using data from the 1994 and 2001 Los Angeles County Mexican Immigrant Residency Status Surveys (LAC-MIRSS) and the 19952002 February and March Current Population Surveys (CPS).
Specifically, I ask four questions: (1) What proportion of unauthorized Mexicans residing in California between 1994 and 2000 were uninsured? (2) What proportion of insured unauthorized Mexicans in California had employer-sponsored health insurance (ESHI), and were unauthorized Mexicans who were eligible for ESHI less likely than were other California residents to purchase it when the employer offered it? (3) How did individual characteristics, such as residency status, age, marital status, and labor market experience; geographic factors, such as minority concentration and homeownership rates; and social integration in the United States (e.g., civic engagement, remitting) influence the probability of health insurance coverage among foreign-born Mexicans in Los Angeles County? And (4) how did individual characteristics (including health insurance coverage), geographic factors, and social integration influence the probability of foreign-born Mexicans in Los Angeles County using medical care services when needed?
In addition to assessing the relative influence of population, neighborhood, and broader socioeconomic factors on health insurance coverage and the use of medical care among Mexican immigrants in general, the theoretical framework, data, and methodology employed here permit an estimation of whether unauthorized residency status among Mexicans living in the United States had an independent effect.
The Unknown Effect of Unauthorized Residency Status on Use of Medical Care
Although California continues its effort to increase the number of insured families residing in the state by expanding its Medical and Healthy Families programs (Lutzky and Zuckerman, 2002),4 one in five Californians and large numbers of immigrants and their children (many of whom are U.S. citizens) remain uninsured (Sorenson, 2001). In California, many immigrants and their children are uninsured because they fear that seeking publicly funded insurance may adversely impact their residency status (Berk and Schur, 2001) or because they work for an employer not offering insurance (Brown and Yu, 2002; Currie and Yelowitz, 2000). Although these two influences are likely to be especially acute among Mexican and other-Latino immigrants residing in California illegally (Aday, 1993; Maida, 2001; Riedel, 1998), decisions concerning what policy instruments may effectively increase coverage rates and receipt of needed medical treatment among this population and their children have had to rely on either (1) national (supra-state) or regional (sub-state) random samples that fail to capture state-level health coverage and care information, or (2) non-random ethnographic data that are not representative of the entire Mexican or other-Latino unauthorized immigrant population residing in California.
Whereas governments and private employers help provide health insurance for approximately 80% of all Americans (Seliger, 2001), most non-elderly uninsured Americans (Currie and Yelowitz, 2000; Glied, 2001) and the vast majority of California's seven million non-elderly uninsured residents work, or they live in families with at least one working adult (Sorenson, 2001). Thus, some researchers suggest that declining rates of health insurance coverage may be explained partly by (1) the 1996 Welfare Reform Act, (2) reduced ESHI availability due to rising medical costs beginning in the early 1980s, and (3) industrial restructuring away from manufacturing and toward service-sector employment. Recent Latino immigrants, both within California (, Flores, and Lopez-Garza, 1992; Maida, 2001; Schur and Feldman, 2001) and nationally (Brown and Yu, 2002; Seccombe, Clarke, and Coward, 1994; Valdez et al., 1993) have been negatively and disproportionately impacted by these trends.
However, systematic research examining whether these macro socioeconomic and political trends and unauthorized residency status impact health insurance coverage or medical care is surprisingly scarce (Hernández and Charney, 1998). In general, bivariate descriptive studies employing data from the 1980s and 1990s report that Mexican and other-Latino unauthorized immigrants had the highest uninsured rates in various locations throughout the United States. Moreover, although this insurance gap between unauthorized Latino immigrants and U.S. citizens narrows only slightly following the legalization of formerly unauthorized residents, it seems to disappear altogether once controlling for other individual, institutional, and broader socioeconomic factors using econometric methods. In short, there appears to be no direct influence of unauthorized residency status on having had health insurance despite an observed insurance coverage gap between unauthorized Latino immigrants and other U.S. residents.
The earliest and to date most statistically sophisticated study (Hubbell et al., 1991) compared health insurance coverage among lower-income unauthorized and authorized Latinos in Orange County, California, using random data collected from a telephone survey conducted in October 1987 and February 1988. Results of bivariate analysis suggest that more unauthorized Latinos (60%) were uninsured compared to other residents—a finding replicated by some of the same researchers when analyzing 803 randomly selected foreign—and native-born adult Latinas in the same county as part of a follow-up study ( et al., 1997).5
Collectively, four additional research projects, employing data from the 1990s rather than the 1980s, offer a wider proportional range of uninsured unauthorized Mexicans and other Latinos (46% to 90%), but these findings also have not been scrutinized econometrically. Work by E. Richard Brown and colleagues at UCLA's Health Policy Research Center in the late 1990s and early 2000s, for example, has generally confirmed the existence of an observed insurance gap between unauthorized Latinos and other U.S. residents at an expanded geographic level. Applying residency status predictors (Marcelli and Heer, 1998) to the 1998 CPS, one study reports that 74% of undocumented Mexican immigrants residing in the United States were without health insurance and only 23% were offered ESHI from their employer (Brown et al., 2000). A second study applying the same survey-based residency status predictors to the February 1997 and March 1998 Current Population Surveys (CPS) finds that not only were unauthorized Mexican immigrants much less likely to have had health insurance but more than half (56%) worked for an employer that did not offer health benefits to its employees (Brown and Yu, 2002). Using the 2001 California Health Interview Survey (CHIS), a third analysis (Brown et al., 2002) provides the first estimates for California, separately, and finds that 51.2% of noncitizens without a green card (a proxy for the unauthorized population) were uninsured. Furthermore, although only half of all employed unauthorized immigrants are estimated to have been offered employer-sponsored health insurance, compared to other workers (72% of authorized immigrants and 88% of U.S.-born citizens), a similar proportion were eligible and accepted the offer by purchasing ESHI. A final effort by this team (Brown et al., 1999) represents the only longitudinal (three-year) analysis of unauthorized immigrants' health insurance coverage to date. It analyzes formerly unauthorized immigrants who were legalized through one of several 1986 Immigration and Reform Control Act (IRCA) programs and were interviewed as part of the Immigration and Naturalization Services' and Department of Labor's Legalized Population Surveys (LPS) to assess whether health insurance coverage for this population changed between 1989 and 1992. Results suggest that Mexican and other-Latino unauthorized immigrants remained approximately one-third less likely to have had insurance before and after legalization compared to the general adult population. Specifically, whereas in 1989, 47% of all pre-amnestied unauthorized immigrants were uninsured and about 17% of the entire adult U.S. population was, by 1992, 46% of all amnestied immigrants remained uninsured, as did almost 19% of the total adult U.S. population. Taken together, these four UCLA-based studies suggest that 46% to 74% of unauthorized Latino immigrants in the United States were uninsured during the past decade.
A third team of scholars based in Washington, D.C., and a fourth representing a collaboration between UCLA and El Colegio de la Frontera Norte (El Colef), estimate similar or slightly higher uninsured rates among unauthorized immigrants. Using data from the Urban Institute's random-digit-dial Los Angeles-New York City Immigrant Survey (LANYCIS), the former group (Capps et al., 2002) reports that 71% of all undocumented immigrants residing in Los Angeles County did not have health insurance. When applying residency status predictors obtained from the 1994 Los Angeles County Mexican Immigrants Residency Status Survey (LAC-MIRSS) to 1994-95 March CPS data, the latter team (Marcelli and Heer, 1998) finds that more than 80% of unauthorized Mexican immigrants residing in Los Angeles County were uninsured.
Lastly, a study by researchers at the Project HOPE Center for Health Affairs in Bethesda, Maryland, employs randomly collected data during 1996-97 in four U.S. urban areas. It finds that the proportion of undocumented Latino immigrants who were eligible and accessed various public benefit programs varied considerably between Los Angeles and Fresno but was generally low (Berk et al., 2000). For instance, only 10% of undocumented Latino immigrants in Los Angeles and 25% in Fresno reported Medical enrollment.6 Assuming a small fraction of Mexican and other-Latino unauthorized immigrants were covered by private (e.g., ESHI) plans, descriptive analyses from studies using data collected in the 1990s intimate that somewhere between 46% and slightly less than 90% of all unauthorized Latino immigrants were uninsured during the past decade. Unfortunately, it appears that the only study to assess whether this observed residency status gap in insurance coverage remains after controlling for other demographic characteristics analyzed children of unauthorized immigrant parents rather than the unauthorized immigrants themselves (Halfon et al., 1997).
The estimated trivial relationship between having received amnesty and IRCA-legalized immigrants having obtained insurance coverage (Brown et al., 1999) may help explain why econometric analysis of the influence on medical care use of unauthorized residency status and having insurance points away from the former and toward the latter determinant. For instance, some of the work summarized above ( et al., 1997; Hubbell et al., 1991) estimates whether unauthorized residency status had an independent impact on the use of medical care. Unsurprisingly, a medical care use gap between unauthorized Latinos and other U.S. residents is found, but the gap is explained by differential employment, insurance coverage, and poverty rates as well as a younger demographic profile among unauthorized immigrants rather than unauthorized residency status per se.7 The story emerging from existing literature then is straightforward. If unauthorized residency status adversely influences the use of medical care facilities, it does so indirectly by reducing access to gainful employment, institutional information, or health insurance coverage.
Data and Estimation Methodology
Following the survey-based residency status estimation methodology pioneered in the 1980s and subsequently extended (Heer et al., 1992; Heer and Passel, 1987; Marcelli, 2004a, 2004b; Marcelli and Heer, 1997; Marcelli and Lowell, 2005), I employ the November 1994 and July 2001 Los Angeles County Mexican Immigrant Residency Status Survey (LAC-MIRSS) data, first, to generate residency status predictors for adults from four demographic variables (age, sex, educational attainment, time residing in the United States).8 In a second stage of the analysis, these predictors are applied to non-elderly adults (age 18 to 64 years) born in Latin America, according to the 1995-2002 February and March Current Population Survey (CPS) data, in order to estimate the number and characteristics of unauthorized Mexican (and other-Latino) non-elderly adult immigrants in California, as well as their health status and health insurance coverage. In a third and final stage, I analyze the 2001 LAC-MIRSS (and several census block-level variables from the U.S. Census Bureau's 1990 Summary Tape File 3 data) separately, to estimate how individual characteristics, geographic factors, and social capital influenced foreign-born Mexicans adults' insurance coverage and use of medical care services.
The 2001 LAC-MIRSS consists of 780 foreign-born Mexican adults who resided in one of 456 households within one of 125 census blocks located in Los Angeles County. Interviewers were instructed to collect data on as many foreign-born Mexican household members as possible, but to do so from only an adult member and for only those other members of the household for whom the respondent believed he or she could provide accurate information. The questionnaire was available in English and Spanish, took 35 minutes on average to administer, and was developed and piloted by researchers from UCLA, Colef, and the Coalition for Humane Immigrants Rights in Los Angeles (CHIRLA). Overall, the household response rate was 62%, and fully 98% of all respondents answered our relatively sensitive residency status questions. Slightly less than half of adult respondents admitted to residing in the United States without being a naturalized citizen, a legal permanent resident, or a temporary visitor (e.g., non-immigrant visa holder). For purposes of the analysis that follows, I employ the full adult sample, but we also reran all our regression models with a sample including one randomly selected adult from each household to check for possible statistical bias resulting from within-household clustering. We did not uncover any significant differences in our estimated parameters, however, and therefore report results produced only from the full sample below.
Specifically, we first generate demographic residency status predictors by regressing whether one was assigned the residency status of unauthorized Mexican immigrant (UMI) on AGE, SEX, educational attainment (EDUC), and years residing in the United States (YEARS) among those of the 780 Mexican-born adults in our 2001 LAC-MIRSS data who were not U.S. citizens (equation 1 below). We do this for household heads and other household members separately, and the percent concordant pairs produced from logistic regression analyses are 82 and 76 respectively. We also checked the robustness of these residency status predictors by rerunning our logistic regression models after randomly selecting one adult from each household, and the estimated parameters were almost identical. A similar process was undertaken using our 1994 LAC-MIRSS data (Marcelli, 2004b; Marcelli and Heer, 1997, 1998; Marcelli, Pastor, and Joassart, 1999).

Consistent with these earlier studies employing the 1994 LAC-MIRSS, when our predictors are applied to Census Bureau public-use data, they generate aggregate estimates of the number of Mexican and other-Latino unauthorized immigrants residing in Los Angeles County that are very similar to those imputed from Census Bureau and Immigration and Naturalization Service estimates (Heer and Passel, 1987; Marcelli, 1999; Marcelli and Heer, 1997). Below, we apply these residency status predictors to foreign-born Mexicans and other (non-Cuban) Latinos residing in California who were not U.S. citizens according to the 19952002 February and March CPS data for California.9
The 1995-2002 March CPS include the four demographic variables needed to produce a probability of having been unauthorized to reside in the United States. After separating individuals by residency status, the data then permit an analysis of self-reported health status and health insurance coverage for particular years.10 Although place of birth began to be asked of respondents in the 1994 March CPS, because of changes to the health insurance questions, we begin with 1995 (which reports insurance coverage in preceding year) (Swartz, 1997). The March CPS includes approximately 11,000 observations annually for California, but it does not include questions regarding whether one was offered employer-sponsored health insurance, whether one was eligible to buy it, and whether one actually purchased it; and some contend that the health status questions are unreliable (Swartz, 1997). Although the 1996, 1998, 2000, and 2002 February CPS data include questions on ESHI offers, eligibility, and take-up, neither they nor the March demographic files have any information below the metropolitan statistical area level. Due to relatively small sample sizes even at the metropolitan level, I concatenate the 1996 and the 1998 February CPS, and the 2000 and 2002 February CPS, to increase statistical power. A year is skipped in each concatenation (1997 and 2001, respectively) to avoid duplicate records in the resulting sample, and sample weights provided for each year are adjusted appropriately.
After estimating the proportion of uninsured Mexican and other-Latino unauthorized immigrants in California using this methodology, as well as their relative health status, uninsured rates, and ESHI access and coverage, I return to the 2001 LAC-MIRSS data to investigate how residency status influenced health insurance coverage and medical care while simultaneously controlling for other demographic characteristics, neighborhood effects, and broader socioeconomic factors.
The descriptive analysis of uninsured rates—and among employed adults, of ESHI take-up rates—below provides useful information regarding the possible effects of unauthorized residency status on health, health insurance coverage, and whether one was covered by ESHI in California. However, like most of the previous research summarized above on insurance coverage, it does not permit causal interpretation because of data limitations and because no econometric methods are employed. The purpose is simply to motivate the econometric estimation I undertake using our 2001 LAC-MIRSS data, and to stimulate future research.
Analyses of the determinants of Mexican and other-Latino immigrants' comparatively low rates of health insurance coverage and medical care use in the United States have emphasized two of the main hypotheses offered from the behavioral or "health services" model of medical care use (Andersen, 1995; Andersen and Davidson, 2001). A higher proportion of Latino immigrants are likely to be unauthorized residents, and Latino immigrants are less likely to work for an employer offering ESHI (Berk and Schur, 2001; Brown and Yu, 2002; Chavez, 1986; Chavez et al., 1997). Both determinants—work and residency status—are viewed as "predisposing demographic characteristics" within this framework, but the initial model also included structural factors and health beliefs (mediated by one's access to "enabling resources" and a perceived or evaluated "need" for medical treatment) as primary influences on family or individual use of medical services, and it has undergone decadal revisions (Andersen, 1968; Andersen and Anderson, 1967). Partly resulting from a series of criticisms from social scientists of various disciplines (e.g., neglect of psychological, cultural or social capital, and genetic factors, inattention to knowledge concerning the functioning of insurance and medical institutions, the need for better measures of beliefs concerning health), debate about what constitutes equitable access to medical care and how the model might accommodate this, and considerations of what components of the model lend themselves more readily to change (e.g., insurance benefits and health beliefs versus demographic characteristics and social structure), a second iteration of the model in the 1970s (Aday and Andersen, 1974) collapsed the three main categories of determinants from the original model of medical care use (e.g., predisposing characteristics, enabling resources, need) into a single category entitled "population characteristics," and introduced three new categories: (1) health care system, (2) use of health services, and (3) consumer satisfaction. Thus, population and health care system characteristics came to be viewed as acting simultaneously on each other and collectively on the use of health care services, which in turn influences consumer satisfaction. And consumer satisfaction replaced the use of medical services as the ultimate goal.
A third iteration during the 1980s and 1990s (table 1) essentially added "external environment" to the model, and provided a more nuanced picture of health outcomes, which included perceived and evaluated health status in addition to consumer satisfaction. Although a fourth iteration of the model that incorporates feedback paths from health outcomes to health behaviors and population characteristics is currently underway (Andersen, 1995), it will be useful to discuss the model I estimate below in the context of the third-phase development (Andersen and Davidson, 2001; Andersen, Davidson, and Ganz, 1994) for two reasons. First, it is the third iteration that explicitly includes a category for physical and economic contextual factors. Second, cross-sectional (e.g., the 2001 LAC-MIRSS) data do not permit the estimation of health feedback loops.
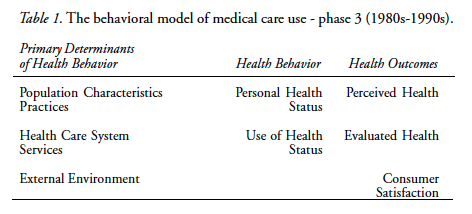
Within the theoretical framework outlined in table 1, unauthorized residency status and having ESHI—as well as a number of other potential demographic and economic determinants, such as educational attainment, sex, age, occupation, income, knowledge of available services, and social network quality—are considered population characteristics. Although inclusion of social network quality may be suspect here given its collective nature, it is important to remember that in phase two of the behavioral model "enabling resources" accompanied "predisposing chaacteristics" and "need" as potential explanations under the population characteristics category. It is not a stretch to view one's personal networks as possibly enabling or assisting one to seek or obtain medical care.
Research in the early 1990s suggested that both Mexican- and U.S.born persons residing in the United States sometimes travel to Mexico to obtain lower cost medical care and pharmaceuticals even though they would prefer to do otherwise (Bruhn and Brandon, 1997). Others, especially those without health insurance and unauthorized immigrants, either forgo seeking care in the immediate term or rely on the "safety net" of public (county, state, and district) hospitals; community health centers; free clinics; and special programs, such as mobile medical vans, school-based health centers, and immunization campaigns (Sekhri, Gomez-Dantes, and Macdonald, 1999). Some of these factors are also potential primary determinants of health behavior. The relative price of medical care in Mexico, for instance, fits neatly under the "external environment" subcategory, and the availability of community and public medical care is most closely aligned under the "health care system" subcategory.
The emerging field of social epidemiology—emphasizing the influence of social (Berkman and Kawachi, 2000) and neighborhood context (Kawachi and Berkman, 2003) on health outcomes—is complementary to what is suggested by the third-phase behavioral model of medical care use. Specifically, conceptualizing demographic characteristics and extra-individual factors as primary determinants that both directly (and indirectly through health behavior) influence health outcomes is consistent with social epidemiology's multicausal approach.11 Although some have argued, based on Aday's (1993) "vulnerable population" framework, that immigrants are most likely to be at risk of not having health insurance and not receiving needed medical care because of both individual and institutional factors (Bollini and Siem, 1995; Leclere, Jensen, and Biddlecom, 1994; Riedel, 1998), no previous work of which I am aware has attempted to investigate the role of residency status and extra-individual influences on health insurance coverage and medical care use among Latino immigrants simultaneously or with data collected in the 2000s. Taking a cue from the various literatures discussed above, I include individual, geographic, and social variables in several logistic regression models specified below to estimate whether unauthorized residency status influenced the probability (1) of having had any type of health insurance (INSURED) among all foreign-born Mexican adults, (2) of having had public rather than private health insurance (PUBLIC) among insured foreign-born Mexican adults, and (3) of having used medical services when needed among all foreign-born Mexican adults (CARE). Viewed from the phase-three behavioral model of medical care use, my focus is first on estimating how unauthorized residency status influenced health insurance coverage (both conceptualized as primary determinants of health behavior and termed "population characteristics") in equations 2 and 3. I next estimate whether unauthorized residency status influenced the use of medical services that were perceived as necessary by the Mexico-U.S. migrant (equation 4). This second focus straddles the behavioral model's health behavior and health outcome categories because use of medical services that were deemed necessary combines "use of health services" (which is considered a health behavior) and "perceived" or "evaluated" health status (which is considered a health outcome).
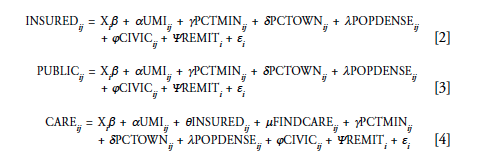
Equation 2 estimates (using logistic regression) whether a Mexican immigrant i, age 18 to 64 and residing in Los Angeles County census block j in July 2001, had health insurance depending on a vector of individual i's characteristics (Xi) other than having been an unauthorized Mexican immigrant (UMI); the percentage of a census block's population who were nonwhite (PCTMIN) or owned their homes (PCTOWN); the number of persons (in thousands) per square mile by census block (POPDENSE); the number of community, neighborhood, school, sports, union, religious or spiritual, and other social events and meetings attended during the year preceding the survey (CIVIC), ranging from 0 to 8 (higher values reflecting someone who is more socially connected or engaged); and whether a person remitted funds to someone in Mexico in 2000 (REMIT).
It is not possible using the LAC-MIRSS data or this empirical implementation to estimate all of the potential determinants of health insurance coverage or medical care use suggested by the behavioral model because of data limitations. It is possible, however, to analyze several potentially important factors ignored by past research on Mexican immigrants. Unauthorized residency status represents one, but our neighborhood environmental factors and social capital variables are others. PCTMIN, PCTOWN, and POPDENSE fit neatly under the "external environment" subcategory of primary determinants, and CIVIC and REMIT are subsumed under "population characteristics" or "external environment." Table 2 defines each variable used in the analyses that follow, and provides means and standard deviations.
Equation 3 estimates the probability that an insured Mexican immigrant i, age 18 to 64, residing in Los Angeles County census block j in July 2001 had public health insurance coverage using logistic regression. And equation 4 estimates the probability that Mexican immigrant i, age 18 to 64 and residing in Los Angeles County census block j in July 2001 received medical care for which there was a perceived need at some time during the previous year. In addition to the variables used to examine variance in having had health insurance in equations 2 and 3, equation 4 also includes whether a person was insured (INSURED) or had difficulty locating a medical care facility when needed (FINDCARE). The former variable is actually separated into public (PUBINSR) and private (PRIVINSR) insurance for estimation purposes. In addition, the latter variable, although measured at the individual level, may reflect geographical factors influencing the use of medical care services not captured by more traditional neighborhood characteristics.12 To correct for possible random effects that may exist because individuals in our data are clustered within census blocks, only results with robust standard errors are reported. In other words, rather than using multilevel statistical techniques to model potential within-block heterogeneity, we use STATA's "cluster" function to control for this.
Results
Uninsured and Employer-Sponsored Health Insurance Rates in California, 1994-2001
Applying the 1994 and 2001 LAC-MIRSS residency status predictors to the 1990 PUMS and 1995-2002 March CPS data, I estimate that the number of Mexican and other-Latino unauthorized immigrants residing in California between 1990 and 2001 rose from 1.2 to 2.3 million (not shown here), with Mexicans representing proportions ranging from 76% (before the passage of Proposition 187 in 1994) to 85% (in 2001) during any given year. Thus, Mexican and other-Latino unauthorized immigrant representation increased by 67.5%—from an estimated 4.0% of approximately 30 million Californians in 1990—to 6.7% of about 34.5 million in 2002.13
Non-elderly Mexican and other Latino unauthorized immigrants had the highest proportion without health insurance throughout the 1990s (between 50% and 70%), and authorized foreign-born Mexicans and other Latinos had the second highest rates (between 35% and 50%) (figure 1). All other ethno-racial groups, regardless of nativity, had fewer than 30% lacking health insurance. These outcomes are likely related to the finding, also not shown here, that during the 1990s and early 2000s, non-elderly unauthorized Latinos also had the lowest ESHI rates (16% to 33%) of any group, and authorized foreign-born Latinos had an ESHI rate of less than 50%. By comparison, more than half of California's entire population had ESHI.

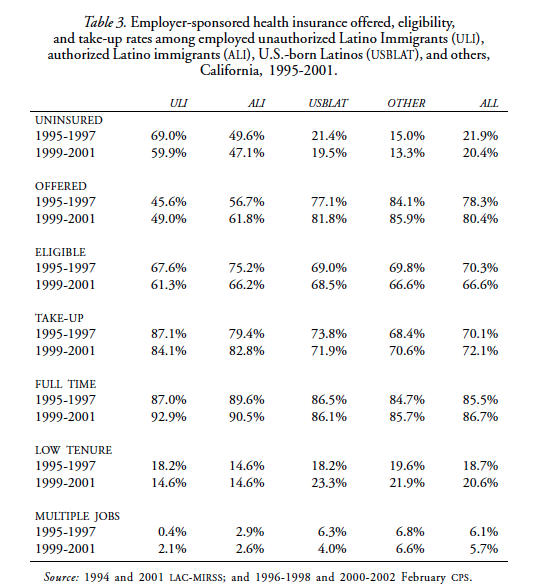
The relatively high uninsured rates and low ESHI rates among unauthorized Latinos in California require a deeper look into whether Latinos were less likely to (1) work for an employer who offered employees the opportunity to purchase ESHI, (2) be eligible to buy into such a program if offered (e.g., employed full-time), or (3) purchase ESHI when it was offered and they were eligible.
A lower proportion of employed unauthorized Latinos (ULI) were offered ESHI compared to authorized Latino immigrants (ALI), U.S.-born Latinos (USBLAT), and other workers (OTHER) in California (table 3). Additionally, a smaller proportion in firms offering ESHI claimed to have been eligible to buy into this benefit program, but surprisingly, when they were offered it and were eligible, a greater proportion bought it ("take-up"). Results further suggest that unauthorized Latinos' lower ESHI coverage rates may be related to relatively low job tenure rather than the inability to obtain employment that is likely to include health insurance benefits. For instance, a relatively high percentage was employed full-time (panel 5) in one job (panel 7), but a smaller fraction had been at their current job for at least one year (panel 6). This is a surprising finding that requires more attention than is possible here. We may tentatively conclude, however, that unauthorized Latinos' lower ESHI coverage is due in part to lower job tenure—not to an unwillingness to work full-time or to purchase insurance when offered at the workplace—and this, in turn, is one factor influencing their relatively low health insurance coverage rates in California.
Health Insurance and Medical Care among Mexican Immigrants in Los Angeles County
Although the foregoing analysis provides a descriptive and longitudinal portrait of unauthorized Latinos' and others' health insurance coverage in California, as well as the relative importance of job-based insurance, its usefulness for understanding whether social environmental factors outside the employment contract (e.g., neighborhood, social capital) influence insurance coverage and medical care use is quite constrained. A second major limitation is the absence of any medical care questions in the CPS. To estimate how several neighborhood context and social environmental factors may have affected Mexican immigrants' insurance coverage and medical care, I turn to the 2001 LAC-MIRSS linked to 1990 census data at the census block level.
According to the weighted 2001 LAC-MIRSS data, an estimated 1,669,620 foreign-born Mexicans aged 18 to 64 were residing in Los Angeles County in July 2001, and approximately 46% (or 764,000) are estimated to have been unauthorized to reside in the United States. This estimate of non-elderly foreign-born adult Mexicans is considerably higher than that reported using March 2002 CPS data (1,398,162),14 but the estimated number of unauthorized Mexicans falls within the current range of estimates interpolated from what is alternatively termed the components-of-change, composite, or residual methodology employed by the former Immigration and Naturalization Service (Warren, 2003), the Bureau of the Census (Costanzo etal., 2001) and leading demographers in the field (Bean et al., 2001).
Analysis of the final non-elderly adult LAC-MIRSS sample (i.e., only those observations with data for all variables) shows that approximately 55% of all foreign-born Mexicans residing in Los Angeles County in July 2001 were uninsured, as was a higher proportion of unauthorized compared to authorized Mexican immigrants (67% versus 46%). This residency status gap in insurance coverage is more consistent with that in the mid-1990sfor all non-elderly unauthorized and authorized Latino immigrant adults in California than it is for that population in the early 2000s (figure 1). Moreover, although the same proportion of authorized and unauthorized immigrants (36%) claimed to have needed medical care during the previous year, a higher proportion of unauthorized immigrants (23% versus 13%) did not receive medical care that they deemed necessary.
The first four "Have Health Insurance?" columns (table 2 above) show that a smaller proportion of those with health insurance were unauthorized, and in addition to being older and having graduated from high school, higher proportions of insured Mexicans were male, spoke English very well, were employed, were in a labor union, and sent remittances to Mexico during 2000. Those with health insurance also had higher incomes on average, and lived in less populated neighborhoods with higher homeownership rates.
Figure 2 provides additional detail concerning how authorized and unauthorized Mexican immigrants usually pay for medical care services received. Specifically, 18% of unauthorized Mexican immigrants usually relied on public insurance (Medi-Cal) compared to 13% of authorized Mexican immigrants, who relied on Medi-Cal or Medicare (e.g., the disabled); and although the proportions of unauthorized and authorized Mexican immigrants having had private health insurance is not tremendously different (72% and 80% respectively), a significantly higher fraction of unauthorized compared to authorized Mexicans were likely to pay "out-of-pocket" for medical services received (57% versus 39%) rather than with ESHI (12% versus 37%).
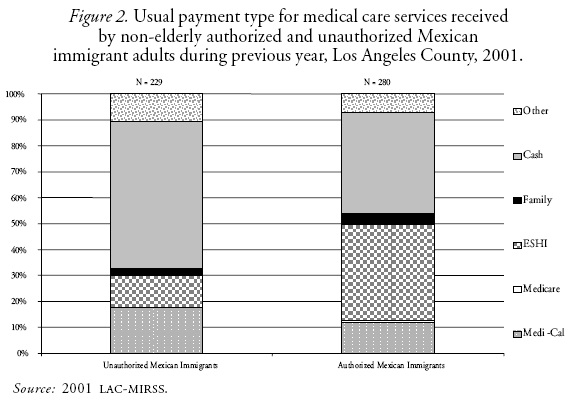
Among the insured, the 33% who had publicly subsidized health insurance (Medi-Cal or Medicare rather than ESHI, insurance provided by a family member, paying out of pocket, or other) were younger, had lower incomes, resided in more densely populated neighborhoods with lower rates of homeownership on average, and attended more meetings and events in their communities (see the four "Insurance Type" columns, table 2). Higher proportions of those with public insurance were also unauthorized females; and lower proportions had graduated from high school, were able to speak English very well, were employed, or were affiliated with a labor union.
Of those claiming that they had needed medical care during the year preceding the 2001 LAC-MIRSS, approximately 83% received it (final four columns, table 2). They tended to be older, male, authorized residents, more proficient with English, high school graduates, married, employed, and affiliated with a labor union compared to those who did not receive needed care. Those receiving needed care also had higher incomes on average, had either public or private health insurance, did not report experiencing any difficulties finding a medical care facility, resided in a neighborhood with higher rates of homeownership, participated more in their communities, and were less likely to remit funds to Mexico.
An examination of Mexican immigrants' source of medical care by residency status further reveals that a smaller proportion of unauthorized immigrants (78%) successfully obtained needed medical attention compared to their legal counterparts (87%). Among Mexican immigrants in Los Angeles County who needed care, unauthorized residents were almost twice as likely as authorized residents (59% versus 34%) to have accessed a publicly subsidized medical care facility, such as a community clinic, emergency room, or public hospital (see figure 3). Conversely, unauthorized Mexicans were less likely (33% versus 47%) to have visited a private doctor or an HMO/PPO medical care facility.

To draw reasonably confident inferences concerning the potential impact of unauthorized residency status on health insurance coverage and use of medical care—even if only for one place, at one point in time—it is necessary to estimate a regression model that controls for other possible individual, geographic, and social influences. Having estimated equations 2, 3, and 4, a fairly straightforward—if unanticipated—story emerges about the impact of unauthorized residency status on Mexican immigrants' health insurance coverage and use of medical care (see table 4). Although unauthorized residency status is estimated to have reduced the probability of a non-elderly Mexican immigrant adult residing in Los Angeles County in July 2001 having had any health insurance (INSURED) and to have increased the probability of having had publicly subsidized insurance (PUBLIC), it had no direct effect on the probability of having received medical care that was perceived to be necessary (nor did it have an indirect effect through insurance coverage). Rather, being married and more socially engaged in one's community were positively associated with having received needed care, and residing in a neighborhood that had a higher proportion of nonwhite residents and having difficulty locating a medical care facility were negatively related.
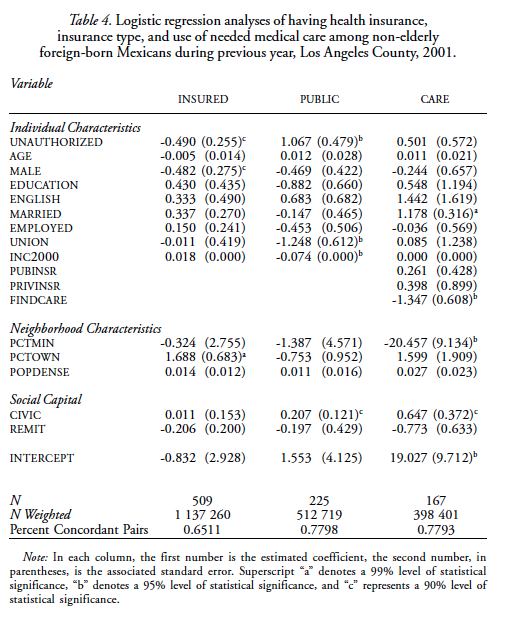
Converting each of the three statistically significant coefficients in the first group of columns into probabilities, we find that being an unauthorized resident or male reduced the probability of having had insurance by approximately 12%, but a one standard deviation increase in the neighborhood homeownership rate augmented it by 12%.15
Being affiliated with a labor union had the largest negative effect (-20%) on the probability that a non-elderly Mexican immigrant adult with insurance had public rather than private coverage, and being unauthorized had the largest positive effect (+26%) (see the second group of columns, table 4). Still, it appears that a one standard deviation rise in annual income (+$10,477) reduced the likelihood of having had public insurance by 17%, and attending 1.5 more neighborhood or community meetings or events was positively associated (+7%).
Although the influence of unauthorized residency status on insurance coverage is interesting, having insurance surprisingly does not appear to have altered the probability of having received needed medical care. Instead, the third group of columns in table 4 intimate that having difficulty locating a medical care facility lowered the probability of having received needed medical care by 27%, and a one standard deviation increase in the percentage of nonwhite residents in one's neighborhood (+0.047) raised it by 13%. Alternatively, two factors may have augmented the probability of having obtained needed care—being married (by 11%) and participating in an additional community activity (by 12%).
Conclusion
Conventional discourse regarding whether and how to expand access to medical care among unauthorized immigrants residing in the United States has focused on equity (ability to pay), equality (proportionate access), or need (relative health) assessments (Asch, Frayne, and Waitzkin, 1995). None of these foci—either alone or jointly—have been politically persuasive, however. Entertaining the possibility that maintaining a large uninsured or unhealthy lower-income population is likely to have broader social welfare effects (Kullgren, 2003) and that obtaining medical care perceived as necessary is influenced by both individual and extra-individual factors, the present study directly tests whether unauthorized residency status among Mexican immigrants independently influences health insurance coverage or use of medical care services, controlling for other demographic characteristics, neighborhood context, and social capital.
Motivated by recent extensions of the behavioral model of medical care (Andersen, 1995; Andersen and Davidson, 2001) and the emerging field of social epidemiology (Berkman and Kawachi, 2000; Kawachi and Berkman, 2003) that emphasize the role of neighborhood context and social environment, I estimate that between 55% and 70% of non-elderly unauthorized Latinos in California were uninsured between 1994 and 2001—a range that is well above both authorized Latinos (35% to 50%) and other Californians (less than 30%). I also find that although unauthorized Latinos had the lowest employer-sponsored health insurance (ESHI) rates in California, they were more likely to have purchased ESHI when employers offered it and when they had an ESHI-eligible job (e.g., full-time). This implies that encouraging employers to offer health insurance to more of their lower-income employees would likely boost insurance coverage rates among unauthorized Latinos in California.
Results generated using 2001 Los Angeles County Mexican Immigrant Residency Status Survey (LAC-MIRSS) data further suggest that implementation of a new amnesty program would both reduce the number of uninsured Mexican immigrants and reduce Mexican immigrants' reliance on publicly subsidized insurance. Whereas 55% of all Mexican immigrants are estimated to have been uninsured in Los Angeles County in 2001, a higher proportion of unauthorized (67%) than authorized (46%) Mexican immigrant residents were also. Unauthorized Mexican immigrants' greater reliance on Medical or their own financial resources rather than ESHI to cover medical expenses compared to their authorized compatriots makes sense in light of this observed 21% residency status insurance gap—but this narrows to 12% after controlling for other individual characteristics, neighborhood context, and social capital. Among these other factors, females and those residing in a neighborhood where a relatively high proportion of residents owned their homes were more likely to be insured. Moreover, results of a public-versus-private insurance logistic regression analysis reveal that although unauthorized Mexican immigrants were 23% more likely than authorized Mexican residents to rely on public health insurance, so, too, were those who participated more in neighborhood and community activities. By contrast, a higher income and being affiliated with a labor union appears to diminish the probability of relying on public health insurance. In summary, although unauthorized residency status appears to directly reduce the probability of health insurance coverage and increase that of relying on public health insurance, certain institutional and social environmental (i.e., employment, neighborhood, social capital) factors also were important. Two obvious implications of such findings are that greater access to better paying unionized jobs and policies designed to reduce homeownership costs may perhaps increase Mexican immigrants' investments in private health insurance.16
Caution at this point, however, is warranted. This analysis shows that neither residency status nor having public or private health insurance appears to influence the likelihood that a Mexican immigrant would have received medical care perceived as necessary by the immigrant. Rather, those who were married or who participated in an additional neighborhood or community activity were, respectively, 16% and 12% more likely to have obtained needed care. Alternatively, those who had trouble locating a medical care facility or who resided in a neighborhood with a relatively high proportion of nonwhite residents were, respectively, 19% and 13%, less likely to have obtained care. Such findings point away from conventional individualist interpretations of why people seek and get the care they think they need, and toward a multi-factorial social environmental interpretation emphasizing the importance of where one resides, the kind of work one does, and with whom one interacts. Based on these findings, it appears that implementing a new legalization program might increase insurance coverage rates and decrease dependence on public programs among unauthorized Mexican immigrants, but the policy lever for augmenting the likelihood that those immigrants receive the care they need appears to lie elsewhere. Neighborhood and network characteristics appear to be more important determinants than are having individual health insurance or residency status. One specific implication is that place-based strategies (e.g., local economic development) are likely to complement population-based policy efforts to increase access to publicly subsidized medical care (e.g., Medical, Healthy Families).
These results support conventional wisdom concerning the existence of an immigrant residency status insurance gap based on earlier descriptive analyses (Brown et al., 1999; Brown et al., 2002; Brown and Yu, 2002); previous findings that unauthorized residency status per se is relatively unimportant in determining medical care use among Mexican immigrants in southern California (Halfon et al, 1997; Hubbell et al., 1991); and the idea emanating from the behavioral model of medical care use (Andersen, 1995; Andersen and Davidson, 2001) and social epidemiology (Berkman and Kawachi, 2000; Kawachi and Berkman, 2003) that social environmental factors accompany individual characteristics as primary determinants of health outcomes.
The focus of this article, however, is not on health outcomes but on health insurance coverage and medical care use. One important direction for future research will be to investigate the relative influence of unauthorized residency status, access to health insurance, and medical care use— compared to neighborhood context and the character of one's social net-works—on specific health outcomes. Another useful effort will be to develop survey instruments that include questions concerning the frequency with which Mexican immigrants interact with those in their social networks (multiplexity) or attend social gatherings (e.g., church, sporting events), the structure of those networks (e.g., size, density, homogeneity, proximity), and metrics for neighborhood and other institutional environmental factors that are likely to influence access to medical care and health outcomes.
References
Aday, Lu Ann, At Risk in America: The Health and Health Care Needs of Vulnerable Populations in the United States, San Francisco (CA), Jossey-Bass Publishers, 1993. [ Links ]
––––––––––, and Ronald A. Andersen, "A Framework for the Study of Access to Medical Care", Health Services Research, 9, 1974, pp. 208-220. [ Links ]
-––––––––––, Development of Indices of Access to Medical Care, Ann Arbor (MI), Health Administration Press, 1975. [ Links ]
Aday, Lu A., Gretchen V. Flemming, and Ronald A. Andersen, Access to Medical Care in the U.S.: Who Has It, Who Doesn't?, Chicago, Pluribus, 1984. [ Links ]
Andersen, Ronald A., Behavioral Model of Families' Use of Health Services, Chicago, Center for Health Administration Studies, University of Chicago (Research Series No. 25), 1968. [ Links ]
Andersen, Ronald A., "Revisiting the Behavioral Model and Access to Medical Care: Does It Matter?", Journal of Health and Social Behavior, 36, March, 1995, pp. 1-10. [ Links ]
-––––––––––, and Odin W. Anderson, A Decade of Health Services, Chicago, University of Chicago Press, 1967. [ Links ]
Andersen, Ronald A., and Pamela Davidson, "Improving Access to Care in America: Individual and Contextual Indicators", in Ronald A. Andersen, T. H. Rice, and G. F. Kominski (eds.), Changing the U.S. Health Care System: Key Issues in Health Services, Policy, and Management, San Francisco, Jossey-Bass Publishers, 2001, pp. 3-30. [ Links ]
-––––––––––, and Patricia Ganz, "Symbiotic Relationships of Quality of Life, Health Services Research, and Other Health Research", Quality of Life Research, 3, 1994, pp. 365-371. [ Links ]
Asch, S., S. Frayne, and H. Waitzkin, "To Discharge or Not to Discharge: Ethics of Care for an Undocumented Immigrant", Journal of Health Care for the Poor and Underserved, 6(1), 1995, pp. 3-8. [ Links ]
Bean, Frank D., Rodolfo Corona, Rodolfo Tuirán, Karen A. Woodrow-Lafield, and Jennifer Van Hook, "Circular, Invisible, and Ambiguous Migrants: Components of Difference in Estimates of the Number of Unauthorized Mexican Migrants in the United States", Demography, 38(3), 2001, pp. 411-422. [ Links ]
Berk, Marc L., and Claudia L. Schur, "The Effect of Fear on Access to Care among Undocumented Latino Immigrants", Journal of Immigrant Health, 3(3), 2001, pp. 151-156. [ Links ]
Berk, Marc L., Claudia L. Schur, Leo R. , and Martin Frankel, "Health Care Access among Undocumented Latino Immigrants: Is Free Health Care the Main Reason Why Latinos Come to the United States? A Unique Look at the Facts", Health Affairs, 19(4), 2000, pp. 51-64. [ Links ]
Berkman, Lisa F., and Ichiro Kawachi (eds.), Social Epidemiology, New York, Oxford University Press, 2000. [ Links ]
Bollini, Paola, and Harald Siem, "No Real Progress Towards Equity: Health of Migrants and Ethnic Minorities on the Eve of the Year 2000", Social Science and Medicine, 41(6), 1995, pp. 819-828. [ Links ]
Brown, E. Richard, Victoria D. Ojeda, Lisa M. Lara, and Abel Valenzuela, Undocumented Immigrants: Changes in Health Insurance Coverage with Legalized Immigration Status, Los Angeles, UCLA Center for Health Policy Research, 1999. [ Links ]
Brown, E. Richard, Victoria D. Ojeda, Roberta Wyn, and Rebecka Levan, Racial and Ethnic Disparities in Access to Health Insurance and Health Care, Los Angeles, UCLA Center for Health Policy Research and the Henry J. Kaiser Family Foundation, 2000. [ Links ]
Brown, E. Richard, Ninez Ponce, Thomas Rice, and Shana A. Lavarreda, The State of Health Insurance in California: Findings from the 2001 California Health Interview Survey, Los Angeles, UCLA Health Policy Research Center, 2002. [ Links ]
Brown, E. Richard, and Hongjian Yu, "Latinos' Access to Employment-Based Health Insurance", in M. M. Suärez-Orozco and M. Päez (eds.), Latinos: Remaking America, Berkeley, University of California Press, 2002, pp. 236-253. [ Links ]
Bruhn, John G., and Jeffrey E. Brandon (eds.), Border Health: Challenges for the United States and Mexico, New York, Garland Publishing, Inc., 1997. [ Links ]
Capps, Randy, Leighton Ku, Michael Fix, Chris Furgiuele, Jeffrey S. Passel, Rajev Ramchand, Scott McNiven, Dan Perez-Lopez, Eve Fielder, Michael Greenwell, and T. Hays, How Are Immigrants Faring After Welfare Reform? Preliminary Evidence from Los Angeles and New York City, Washington (D.C.), The Urban Institute, 2002. [ Links ]
Carrillo, J. Emilio, Fernando M. Trevino, Joseph R. Betancourt, and Alberto Coutasse, "Latino Access to Health Care: The Role of Insurance, Managed Care, and Institutional Barriers", in M. Aguirre-Molina, C. W. Molina, and R. E. Zambrana (eds.), Health Issues in the Latino Community, San Francisco, Jossey-Bass, 2001, pp. 55-73. [ Links ]
Chan, Theodore C., Scott J. Krishel, Kenneth J. Bramwell, and Richard F. Clark, "Survey of Illegal Immigrants Seen in an Emergency Department", The Western Journal of Medicine, 164(3), 1996, pp. 212-216. [ Links ]
Chávez, Leo R., "Mexican Immigration and Health Care: A Political Economy Perspective", Human Organization, 45(4), 1986, pp. 344-352. [ Links ]
-––––––––––, Wayne A. Cornelius, and Oliver W. Jones, "Mexican Immigrants and the Utilization of Health Services", Social Science and Medicine, 12, 1985, pp. 93-102. [ Links ]
Chávez, Leo R., Estevan T. Flores, and Marta Lopez-Garza, "Undocumented Latin American Immigrants and U.S. Health Services: An Approach to a Political Economy of Utilization", Medical Anthropology Quarterly, 6(1), 1992, pp. 6-26. [ Links ]
Chávez, Leo R., F. Allan Hubbell, Shiraz I. Mishra, and R. Burciaga Valdez, "Undocumented Latina Immigrants in Orange County, California: A Comparative Analysis", International Migration Review, 31(1), 1997, pp. 88-107. [ Links ]
Costanzo, Joe, Cynthia Davis, Caribert Irazi, Daniel Goodkind, and Roberto Ramirez, Evaluating Components of International Migration: The Residual Foreign-born, Suitland (MD), U.S. Bureau of the Census (Population Division Working Paper #61), 2001. [ Links ]
Currie, Janet, and Aaron. Yelowitz, "Health Insurance and Less Skilled Workers", in D. Card and R. M. Blank (eds.), Finding Jobs: Work and Welfare Reform, New York, Russell Sage Foundation, 2000, pp. 233-61. [ Links ]
Fragomen, Jr., Austin T., "The Illegal Immigration Reform and Immigrant Responsibility Act of 1996", International Migration Review, 31(2), 1997, pp. 438-460. [ Links ]
Glied, Sherry A., "Challenges and Options for Increasing the Number of Americans with Health Insurance", Inquiry, 38, 2001, pp. 90-105. [ Links ]
Halfon, Neal, David L. Wood, R. Burciaga Valdez, Margaret Pereyra, and Naihua Duan, "Medicaid Enrollment and Health Services Access by Latino Children in Inner-City Los Angeles", Journal of the American Medical Association, 277(8), 1997, pp. 636-641. [ Links ]
Hayes-Bautista, David E., Werner Schink, and Gregory Rodríguez, Latino Immigrants in Los Angeles: A Portrait from the 1990 Census, Los Angeles, Alta California Policy Research Center/Community Partners, 1995. [ Links ]
Heer, David M., V. Agadjanian, F. Hammad, Y. Qiu, and S. Ramasundaram, "A Comparative Analysis of the Position of Undocumented Mexicans in the Los Angeles County Work Force in 1980", International Migration, 3(2), 1992, pp. 101-126. [ Links ]
Heer, David M., and Jeffrey S. Passel, "Comparison of Two Methods for Computing the Number of Undocumented Mexican Adults in Los Angeles County", International Migration Review, 21(4), 1987, pp. 1446-1473. [ Links ]
Hernández, Donald J., and Evan Charney (eds.), From Generation to Generation: The Health and Well-Being of Children in Immigrants Families, Washington (D.C.), National Academy Press, 1998. [ Links ]
Hubbell, F. Allan, Howard Waitzkin, Shiraz I. Mishra, John Dombrink, and Leo R. , "Access to Medical Care for Documented and Undocumented Latinos in a Southern California County", The Western Journal of Medicine, 54(4), 1991, pp. 414-17. [ Links ]
Institute of Medicine, Access to Health Care in America, Washington (D.C.), National Academy Press, 1993. [ Links ]
Kawachi, Ichiro, and Lisa F. Berkman (eds.), Neighborhoods and Health, New York, Oxford University Press, 2003. [ Links ]
Kullgren, Jeffrey T., "Restrictions on Undocumented Immigrants' Access to Health Services: The Public Health Implications of Welfare Reform", American Journal of Public Health, 93(10), 2003, pp. 1630-1633. [ Links ]
Leclere, Felicia B., Lief Jensen, and Ann E. Biddlecom, "Health Care Utilization, Family Context, and Adaptation among Immigrants in the United States", Journal of Health and Social Behavior, 35(4), 1994, pp. 370-384. [ Links ]
Loue, Sana, and Jonathon Foerstel, "Assessing Immigration Status and Eligibility for Publicly Funded Medical Care: A Questionnaire for Public Health Professionals", American Journal of Public Health, 86(11), 1996, pp. 1623-1625. [ Links ]
Lutzky, Amy Westpfahl, and Stephen Zuckerman, Recent Changes in Health Policy for Low-Income People in California, Washington (D.C.), The Urban Institute, 2002. [ Links ]
Lynch, John W., and George A. Kaplan, "Socioeconomic Position", in L. F. Berkman and Kawachi Ichiro (eds.), Social Epidemiology, New York, Oxford University Press, 2000, pp. 12-35. [ Links ]
Maida, Carl A., Access to Health Care for California's Immigrants, 2001. Accessed at www.healthcareoptions.ca.gov/default.asp (no longer available on the Internet). [ Links ]
Marcelli, Enrico A., "Undocumented Latino Immigrant Workers: The L.A. Experience", in D. W. Haines and K. E. Rosenblum (eds.), Illegal Immigration in America: A Reference Handbook, Westport (CT), Greenwood Press, 1999, pp. 193-231. [ Links ]
-––––––––––, "The Institution of Unauthorized Residency Status, Neighborhood Context, and Mexican Immigrant Earnings in Los Angeles County", in D. Champlin and J. Knoedler (eds.), The Institutionalist Tradition in Labor Economics, Armonk (New York), M.E. Sharpe, 2004a, pp. 206-228. [ Links ]
-––––––––––, "Unauthorized Mexican Immigration, Day Labour and Other Lower-wage Informal Employment in California", Regional Studies, 38(1), 2004b, pp. 1-13. [ Links ]
-––––––––––, and David M. Heer, "Unauthorized Mexican Workers in the 1990 Los Angeles County Labour Force", International Migration, 35(1), 1997, pp. 59-83. [ Links ]
-––––––––––, "The Unauthorized Mexican Immigrant Population and Welfare in Los Angeles County: A Comparative Statistical Analysis", Sociological Perspectives, 41(2), 1998, pp. 279-302. [ Links ]
Marcelli, Enrico A., and B. Lindsay Lowell, "Transnational Twist: Pecuniary Remittances and Socioeconomic Integration among Authorized and Unauthorized Mexican Immigrants in Los Angeles County", International Migration Review, 39(1) (forthcoming). [ Links ]
Marcelli, Enrico A., Manuel Pastor, jr., and Pascale M. Joassart, "Estimating the Effects of Informal Economic Activity: Evidence from Los Angeles County", Journal of Economic Issues, 33(3), 1999, pp. 579-607. [ Links ]
National Health Foundation and UCLA Center for the Study of Latino Health, Barriers to Health Care for U.S. Citizen Children of Undocumented Parents, Los Angeles (CA), 1994. [ Links ]
Riedel, Ruth Lyn, "Access to Health Care", in S. Loue (ed.), Handbook of Immigrant Health, New York, Plenum Press, 1998, pp. 101-123. [ Links ]
Schur, Claudia L., Marc L. Berk, Cynthia D. Good, and Eric N. Gardner, California's Undocumented Latino Immigrants: A Report on Access to Health Care Services, Washington (D.C.), The Henry J. Kaiser Family Foundation, 1999. [ Links ]
Schur, Claudia L., and J. Feldman, Running in Place: How Job Characteristics, Immigrant Status, and Family Structure Keep Hispanics Uninsured, New York, The Commonwealth Fund, 2001. [ Links ]
Seccombe, Karen L., Leslie Clarke, and Raymond T. Coward, "Discrepancies in Employment-Sponsored Health Insurance among Hispan-ics, Blacks, and Whites: The Effects of Sociodemographic and Employment Factors", Inquiry, 31, 1994, pp. 221-229. [ Links ]
Sekhri, Neelam K., Octavio Gómez-Dantes, and Tracy Macdonald, Cross Border Health Insurance: An Overview, Oakland, California HealthCare Foundation, 1999. [ Links ]
Seliger, Jerome, Health Care Options for California, 2001. Accessed at www.healthcareoptions.ca.gov/default.asp (no longer available on the Internet). [ Links ]
Siddharthan, Kris, and Melissa Ahern, "Inpatient Utilization by Undocumented Immigrants without Health Insurance", Journal of Health Care for the Poor and Underserved, 7(4), 1996, pp. 355-363. [ Links ]
Sorenson, R., Profile of the Uninsured in California, 2001. Accessed at www.healthcareoptions.ca.gov/default.asp (no longer available on the Internet). [ Links ]
Stern, Andrew L., "Labor Rekindles Reform", American Journal of Public Health, 93(1), 2003, pp. 95-98. [ Links ]
Stevenson, Richard W., and Robin Toner, "Bush says Kerry is Pushing Nationalized Health Care", The New York Times, September 17, 2004, p. A13. [ Links ]
Swartz, Katherine, "Changes in the 1995 Current Population Survey and Estimates of Health Insurance Coverage", Inquiry, 34, Spring, 1997, pp. 70-79. [ Links ]
United States Commission on Immigration Reform, U.S. Immigration Policy: Restoring Credibility, Washington (D.C.), U.S. Government Printing Office, 1994. [ Links ]
Valdez, R. Burciaga, Hal Morganstern, E. Richard Brown, Roberta Wyn, Chao Wang, and William Cumberland, "Insuring Latinos Against the Costs of Illness", Journal of the American Medical Association, 269, 1993, pp. 889-894. [ Links ]
Wallace, Steven, Hongjian Yu, Carolyn Méndez, and E. Richard Brown, Adjusted Estimates of Uninsured Children and Program Eligibility, California 1996, Los Angeles, UCLA Center for Health Policy Research, 1998. [ Links ]
Warren, R., Estimates of the Unauthorized Immigrant Population Residing in the United States: 1990 to 2000, Washington (D.C.), U.S. Immigration and Naturalization Service, 2003. [ Links ]
*Support for this research was provided by the UC Institute for Labor and Employment (ILE), the UC California Program on Access to Care (CPAC), and the Robert Wood Johnson Foundation. I would also like to thank Shannon McConville for valuable research assistance, as well as Victoria Ojeda, Leighton Ku, Rick Brown, Susan Carter, Abel Valenzuela, Kevin Deardorff and two anonymous referees for valuable suggestions on earlier drafts presented at the Social Science Research Council Minority Student Workshop, Los Angeles, CA: UCLA Center for Urban Poverty Studies (8-2-02); the Expanding Access to Care Conference, Jointly Sponsored by the UC California Program on Access to Care, California Policy Research Center, University of California Office of the President and the California State Senate Office of Research: Sacramento, CA (8-15-02); the Effects of Immigrant Legalization Program on the United States conference, National Institutes of Health (9-25-02), the U.S. Bureau of the Census Migration Speaker Series, Suitland, MD (10-7-03); and the Association for Public Policy Analysis and Management Immigrant Health and Well-Being in Policy Perspective session, Washington, D.C. (11-7-03). The Los Angeles County Mexican Immigrant Residency Status Survey (LAC-MIRSS) was implemented through the UCLA Lewis Center for Regional Policy Studies with the assistance of David Heer of UCSD, Polly Vigil, Jesús Montenegro and Jorge Santibáñez Romellón of El Colegio de la Frontera Norte, and Susan Alva, formerly of the Coalition for Humane Immigrant Rights of Los Angeles (CHIRLA).
1 I use the term unauthorized rather than undocumented because being documented may not be synonymous with residing in the United States legally, and it is the effect of residency status on health insurance coverage and use of medical care that is of concern in this study. For instance, one may have documents (albeit false), and thereby be residing illegally in the United States (Marcelli, 1999). Alternatively, it is possible for someone to be documented and a legal resident while a decision regarding their longer-term status is pending (Loue and Foerstel, 1996).
2 Subsequently, the Commission made two other main recommendations: to stabilize legal "immigration policy" and invest in "immigrant policy" to assist with immigrant incorporation in the United States.
3 See also California Immigrant Welfare Collaborative, "Major Benefit Programs Available to Immigrants in California." Available at http://www.nilc.org/ciwc/. Accessed on November 5, 2004.
4 The "Healthy Families" program was created in California in 1997 as part of the federal State Children's Health Insurance Program (SCHIP) and federal income eligibility changes to Medi-Cal for child access (Brown et al., 2002).
5 Employing random household data, another team of researchers (Halfon et al., 1997) found that the residency status of immigrant parents in two Los Angeles urban areas (East Los Angeles and South Central Los Angeles) did not affect whether their children were covered by Medi-Cal, California's Medicaid program, in 1992. Approximately 40% had been covered by the program since birth. These results are generally consistent with earlier studies in Los Angeles (Hayes-Bautista, Schink, and Rodríguez, 1995; National Health Foundation and UCLA Center for the Study of Latino Health, 1994), but the authors suggest that parental residency status may have become a barrier to child Medi-Cal access after voter approval of California's Proposition 187, which, had it been implemented, would have denied the children of unauthorized parents access public health services. Because the focus of this article is on how unauthorized residency status influences insurance coverage and medical care of non-elderly adult Mexicans, the 60% uninsured rate of children with unauthorized parents is only of tangential interest. Others (Wallace et al., 1998) have estimated the number of uninsured unauthorized children eligible for Healthy Families and Medi-Cal in California.
6 This is similar to Marcelli and Heer's (1998) estimate for unauthorized Mexicans in Los Angeles County.
7 Other studies confirm that unauthorized immigrants are much less likely to have health insurance and use medical care, but these have been limited to a single institution, such as an emergency room (Chan et al., 1996) or locality (Chavez, Cornelius, and Jones, 1985), and do not systematically control for competing factors.
8 The most recent estimates of the number of unauthorized immigrants residing in the United States by the former Immigration and Naturalization Service (INS) rely on the 2001 LAC-MIRSS estimates of the census undercount of unauthorized Mexican immigrants in Los Angeles County (Warren, 2003).
9 Residency-status predictors are available upon request from the author. For the current analysis, we applied the predictors from the 1994 LAC-MIRSS to the 1995-1997 March CPS and those from the 2001 LAC-MIRSS to the 1998-2002 March CPS.
10 The five major categories of health insurance are (1) Medicare, (2) Medicaid, (3) Employer-sponsored, (4) Other private, and (5) Military.
11 A focus on the social causes of illness is not new. In medieval Europe, Paracelsus highlighted unusually high rates of disease in miners; John Graunt counted deaths in country parishes in seventeenth-century England and reported social variations in morbidity and mortality; during the mid-nineteenth century, various physicians and social scientists (e.g., Villerme, Virchow, Engels) noted that poor living and working conditions impinged upon health; and in the late 1800s, Durkheim argued that one of the most intimate and personal acts (suicide) is a function of group social integration rather than individual characteristics (Berkman and Kawachi, 2000; Lynch and Kaplan, 2000).
12 I also investigated several other possible geographic determinants of medical care use (availability of public transportation, its quality, and cost) measured at the individuallevel, which turned out not to be as useful as FINDCARE.
13 The authorized Latino immigrant population rose by 60% (from 1.6 million to 2.9 million), and the total foreign-born Latino population grew from 2.8 million (or 9.3% of California's population) to 5.2 million (or 14.6% of California's population).
14 The total Mexican-born population is estimated to have been 1,831,845 (2001 LAC-MIRSS) and 1,653,208 (March 2002 CPS).
15 Statistically significant parameters (βi) associated with dichotomous or "dummy" variables, such as UNAUTHORIZED, MALE, MARRIED, UNION, and FINDCARE, are converted into probabilities using the following formula: 1/(1+e–[ln(μ/(1–μ)+βi])–μ, where μ is the mean of the dependent variable (INSURED, PUBLIC, or CARE) and e=2.7182818. Any coefficient associated with a statistically significant continuous variable, such as INC2000, PCTMIN, PCTOWN, and CIVIC, is converted to a probability more simply by multiplying the coefficient by μ, 1–μ, and a one-standard-deviation increase in the value of the independent variable.
16 This is arguably an inefficient policy for increasing health insurance coverage, but it is reasonable that a lower monthly mortgage may result in the decision to purchase health insurance.














