Introduction
Epilepsia partialis continua (EPC) is part of the focal status epilepticus spectrum. Standardized management for this condition remains unknown. Stroke-induced EPC (SIEPC) is a rare disorder with unknown frequency. We aim to describe a single-center case series regarding this uncommon condition, emphasizing clinical outcomes.
Methods
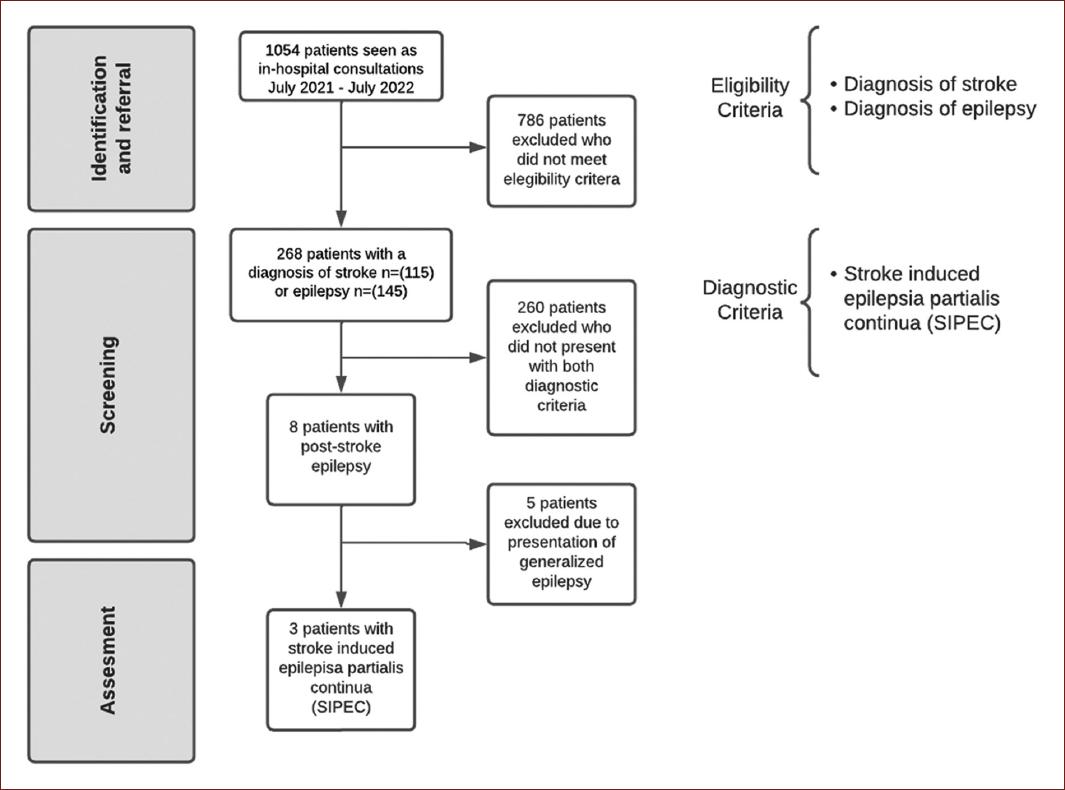
We considered consecutive adult patients (≥ 18 years) with a history of stroke or epilepsy admitted to the Hospital Civil Fray Antonio Alcalde (Guadalajara, Mexico) from July 1, 2021, to July 1, 2022. Inclusion criteria were: ≥ 18 years, with an admission diagnosis of previous or acute stroke, history of post-stroke epilepsy, and SIEPC. Exclusion criteria were generalized status epilepticus and epilepsy before stroke. We identified 1052 patients seen in-hospital consultation using the electronic health record. During this period, 268 patients presented with the diagnosis of stroke or epilepsy. We identified eight patients with post-stroke epilepsy and excluded five due to generalized epilepsy diagnosis. We finally included three patients with a diagnosis of SIEPC (Fig. 1).
Patients received standard diagnostic (including electroencephalographic assessment) and treatment protocols. A board-certified neurologist made the diagnosis on clinical grounds and supported by brain imaging and electroencephalogram (EEG). We defined EPC as continuously repeated motor seizures with preserved consciousness lasting at least 1 h, confirmed with an electroencephalogram. We analyzed the following sociodemographic variables: age, gender, stroke risk factors (dyslipidemia, hypertension, diabetes, and atrial fibrillation), clinical symptoms, EEG findings, radiological findings in computerized tomography (CT) or magnetic resonance imaging (MRI), stroke localization, pharmacological treatment, the use of mechanical ventilation, clinical outcome, and follow-up.
Results
After a systematic search, we identified eight patients with post-stroke epilepsy. Three of these presented with SIEPC (< 1% frequency [0.28%]) (Table 1). All three patients had clinical, radiological, and electrophysiological findings consistent with SIEPC.
Table 1 Demographic and clinical information of patients with stroke-induced epilepsia partialis continua
| Case | Sex | Age | Medical history | Clinical presentation | Imaging | Radiologic diagnosis | Abnormal EEG | Treatment | Pharmaco resistant epilepsy | Death |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 49 | Type 2 diabetes and hypothyroidism | Hemifacial seizures with accompanying aphasia | MRI | IS | + | Levetiracetam (2 g every 12 h), Valproate (600 mg every 8 h), Carbamazepine (200 mg every 6 h), Lacosamide (200 mg every 12 h) | + | - |
| 2 | F | 49 | Hypertension, obesity, dyslipidemia | Lingual seizures with accompanying motor faciobrachial progression | MRI | ICH | + | Levetiracetam (1 g every 12 h), Oxcarbazepine (600 mg every 12 h) | - | - |
| 3 | M | 72 | Type 2 diabetes, hypertension, and chronic kidney disease | Hemiparesis with accompanying rhythmic clonic movements (synchronic, face-arm-leg) | CT | IS | + | Levetiracetam (1 g every 12 h), Phenytoin (100 mg every 8 h), Clonazepam (0.25 mg every 8 h), Valproate (1 g every 8 h) | + | - |
MRI: magnetic resonance imaging; CT: computed tomography; EEG: electroencephalogram; IS: ischemic stroke; ICH: intracerebral hemorrhage.
Patient 1
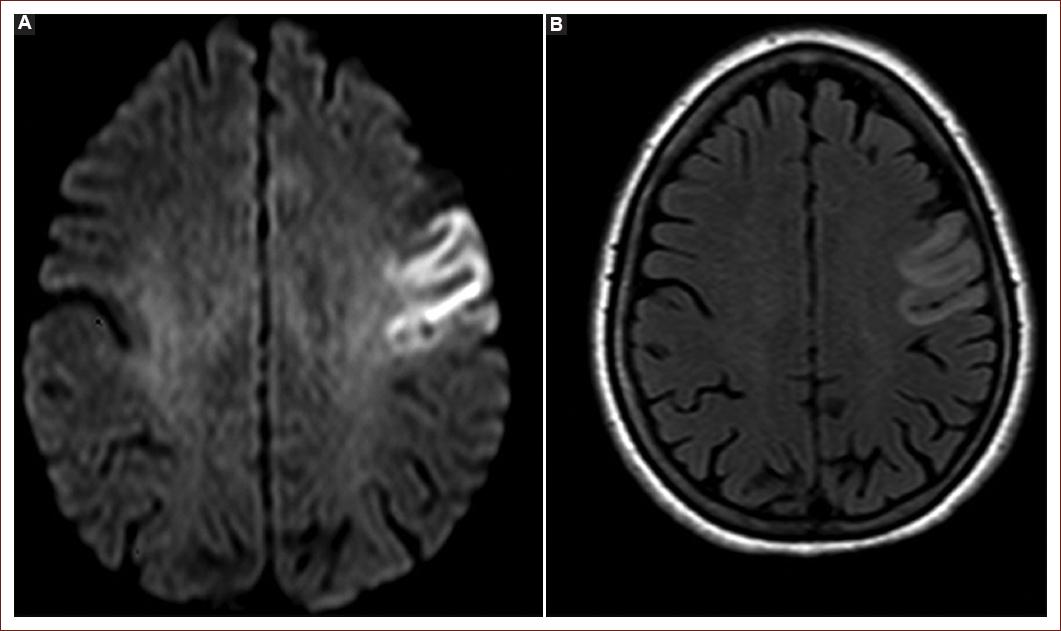
A 49-year-old right-handed female experienced right hemifacial weakness. After 26 days of this event, she presented to the emergency room with repeated right hemifacial seizures, aphasia, and preserved awareness. Her medical history was relevant for Type 2 diabetes mellitus and hypothyroidism. Unenhanced brain computed tomography (CT) was unremarkable. MRI showed subacute infarction involving the left frontocortical and superior frontal gyrus (Fig. 2). The ictal standard scalp EEG reported the presence of continuous focal epileptiform discharges in the left centroparietal region and no secondary generalization. We treated her with levetiracetam, valproate, lacosamide, and carbamazepine (doses shown in Table 1). On 8-month follow-up, she remained seizure-free with levetiracetam and valproate. After extended workup, the stroke was classified as an embolic stroke of unknown source.
Patient 2
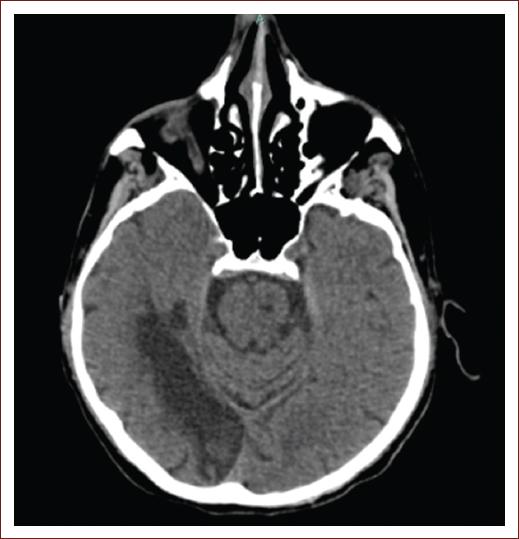
A 49-year-old right-handed female presented to the emergency room after experiencing lingual motor seizures with motor left faciobrachial progression. She had a history of hypertension, obesity, and dyslipidemia. CT scan revealed an intracerebral hemorrhage (ICH) in the right frontal lobe at the level of the precentral gyrus. Brain MRI showed a lesion at the same level (T2 hypointensity with isointense center and a "popcorn" appearance with associated perilesional edema) consistent with a cerebral cavernous venous malformation (cavernoma) (Fig. 3). The ictal standard scalp EEG showed right frontocentral discharges (F4-C4) with propagation to the contralateral hemisphere. At admission, we treated her with oxcarbazepine and levetiracetam (doses shown in Table 1). The patient responded well to pharmacotherapy.
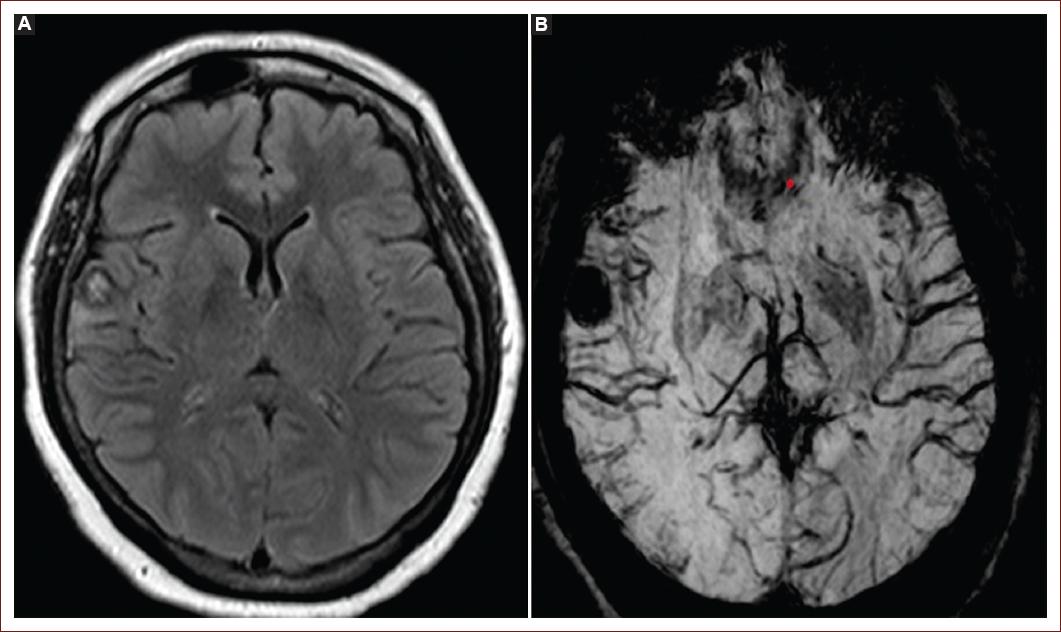
Figure 3 Fluid-attenuated inversion recovery magnetic resonance imaging (MRI) (A) shows a hypointense lesion with an isointense center (popcorn appearance) and perilesional edema in the right parietal operculum. Susceptibility-weighted angiography MRI (B) reveals a hypointense lesion in the right parietal operculum.
The lesion was surgically removed, and the patient remained seizure-free on 2-month follow-up.
Patient 3
A 72-year-old right-handed male presented to the emergency department with left hemiparesis and rhythmic, ipsilateral, and clonic movements (synchronic, face-arm-leg). He had a history of type 2 diabetes, hypertension, and chronic kidney disease. A brain CT scan showed a right temporal-occipital gyrus infarction consistent with a posterior cerebral artery territory stroke (Fig. 4). The ictal standard scalp EEG showed irregular rhythm, right hemispheric slowing, and lateralized periodic discharges (LPDs). The abnormal left-sided movements stopped abruptly after a benzodiazepine challenge but reinitiated acutely after a few minutes. The patient remained awake throughout the hospital admission and was treated with a combination of levetiracetam, phenytoin, clonazepam, and valproic acid with marked improvement (doses shown in Table 1). The patient was discharged against medical advice and was lost to follow-up. This patient's stroke was classified as cryptogenic due to an incomplete workup.
Discussion
EPC was first described by Yakovlevich Kozhevnikov in 1894 but lacks a universally accepted definition1. It is a subtype of focal status epilepticus defined as continuous regular or irregular muscular clonic twitching affecting a limited body part for at least an hour2. Consciousness is typically preserved, and the twitching most commonly involves the face, arms, or both3. The diagnosis is usually supported with an EEG; however, it may be normal4. EPC is uncommon, but when identified, a common underlying cause is stroke4-6.
Stroke is the most common cause of epilepsy in older adults, accounting for approximately 20% of the cases7,8. The incidence of post-stroke status epilepticus is 0.1-0.9%9. Stroke is also the most common cause of status epilepticus in people over 60 years10. The risk of seizures is highest in the first week after stroke11. Early seizures (< 14 days after stroke) have a 35% increased risk of later epilepsy, but the risk of epilepsy after late seizures (> 14 days after stroke) increases to 90%12. The stroke subtype is also a significant predictor of seizures and epilepsy. Hemorrhagic stroke patients have a higher incidence of seizures compared to ischemic stroke. A symptomatic post-stroke seizure has a > 60% probability of seizure recurrence13. Large infarcts with cortical involvement increase the risk of epilepsy, and the localization of the lesion determines seizure type14.
SIEPC is rare, the frequency of this condition is unknown, and few studies have focused on determining its incidence. A prospective study conducted by Bentes et al. showed an incidence of 1.7% among 151 patients with stroke. However, the study sample was small, with no similar studies15.
The differential diagnosis for this rare condition includes cluster seizures (> 3 seizures in 24 h) and other abnormal movement disorders such as hemiballismus and hemichorea16. A benzodiazepine challenge (clonic movement cessation after IV administration of short-acting benzodiazepine) may help distinguish these entities.
Management of EPC remains to be seen. Studies are highly heterogeneous, with variable clinical responses to antiseizure drugs15. However, anti-seizure medications (ASMs) such as levetiracetam, carbamazepine, and lacosamide have shown promising responses with seizure resolution. These results, although showing adequate responses, should be taken with caution, since only one patient was included for each study17-19. Other approaches such as vagus nerve stimulation, transcranial brain stimulation, and alcohol; performed in four, one, and one patient, respectively; have also been used in EPC unresponsive to medical therapy20-22.
SIEPC response to ASMs is varied and presents a worse clinical response than EPC due to other etiologies. In a study conducted by Phabphal et al., all patients with EPC due to metabolic etiologies responded well to ASMs, but only 81% of the patients with SIEPC responded well to ASMs3. In our case series, all patients required two or more ASMs to archive clinical response. Levetiracetam was administered to all patients, with favorable outcomes; only one patient (Case 3) could not be evaluated in the follow-up but showed partial resolution within hospitalization. Previous studies have shown adequate clinical responses with the use of levetiracetam in SIEPC secondary to traumatic hemorrhagic intracerebral hemorrhage23, venous sinus thrombosis24, and ischemic stroke25,26. One of the limitations of these studies is that all were one patient-case reports; therefore, further studies should be conducted to confirm these findings. Other therapies used for SIEPC include fosphenytoin and clobazam27. The dose of ASMs could also impact the patient's outcome; in our series, we used either a dose of 1 g of levetiracetam every 12 h or 2 g every 12 h, similar to the doses used by Brigo et al26. and Haase et al23. Unfortunately, other case reports of SIEPC do not specify dosing.
In our case series, SIEPC secondary to ischemic stroke required more than two ASMs to archive clinical response, contrary, SIEPC secondary to ICH only required two ASMs to archive seizure resolution. Previously, Haase et al. showed similar results of seizure resolution of SIEPC secondary to ICH with the use of levetiracetam23.
Timing between seizure onset and treatment administration could also impact the clinical response of the patients since previous studies have shown that delayed treatment is related to longer duration of the episodes28. This could be explained by the greater momentum gained with the longer duration of the episodes6. Hyperglycemia may also contribute to worse clinical outcomes28,29. However, more studies should be conducted to confirm this hypothesis.
Our study has strengths and limitations. We acknowledge that it was a single-center retrospective design, and the small sample size may be a substantial limitation of our study. As an in-hospital consultation department, most patients are admitted to the geriatric or internal medicine ward. Patients with subtle clinical manifestations in other departments may be unrecognized.
Stroke is a prevalent neurological disorder in in-hospital admissions, and this complication must be correctly identified. Our study includes many screened patients with epilepsy or stroke. All patients were treated directly by us, and we were directly involved in the diagnosis and treatment. In this study, the frequency of SIEPC was low. However, cerebrovascular disease is a common cause of hospital admission, making this disorder clinically relevant. The lack of diagnostic criteria and treatment protocols for SIEPC is striking.
Conclusion
Stroke-induced epilepsia partialis continua is rare. However, given the high prevalence of stroke as a common cause for hospital admissions, it is essential for practicing physicians to be aware of this condition. This study draws attention to this distinct clinical entity with variable presentation, diagnosis, treatment, and prognostic issues. We need a precise diagnostic strategy for this patient population, and more studies are required to guide adequate management.











 nueva página del texto (beta)
nueva página del texto (beta)