Introduction
Acute Ischemic Stroke (AIS) is the leading cause of death and disability worldwide1, and reperfusion therapies are very effective in reducing the number of patients who suffer a deterioration in their functional status due to AIS2,3. There is relative consensus on the tendency to simplify imaging tests to select patients diagnosed with large vessel occlusion (LVO) in the early window and to dispense with multimodal neuroimaging4. However, the potential benefit of mechanical thrombectomy (MT) in patients with ≥ 6 hours of evolution depends on proper selection of slow progressors, which is directly related to a good leptomeningeal collaterality5. Perfusion studies have proven to be useful in predicting the volume of ischemic core and critical hypoperfusion6, although they have the disadvantage of increasing exposure to higher doses of contrast and radiation, in addition to requiring post-processing, which, even with automated software, prolongs the time required to decide on the therapeutic approach7.
Perfusion studies are not widely available in primary stroke centers, which is a major limitation when it comes to being able to increase the time criteria for selection of patients susceptible to endovascular therapy that could be taken to comprehensive stroke centers. For this reason, selection methods based only on computed tomography (CT) in late-window patients are being explored8.
The usual neuroimaging protocol for the study of AIS includes CT angiography (CTA) from the aortic arch to the vertex, which is usually performed in the arterial phase9.
Hypoattenuation in CT angiography source images (CTA-SI) in early arterial phase has been shown to be more sensitive than Alberta Stroke Program Early CT Score (ASPECTS) of brain parenchyma to determine tissue at risk of ischemia, so it could be a good tool to determine viable salvageable tissue in an extended window10,11
Our hypothesis is that the addition of a second acquisition at 35-50 seconds could complement the assessment of hypoperfused tissue that fails to receive flow through pial vessels.
Methodology
Our study is a retrospective analysis of a prospective cohort named Registro de Enfermedades Cerebrovasculares de Clínica Alemana de Santiago (RECCA), which registered consecutive adults patients under informed consent approved by the Institutional Ethics Committee. The initial registry included all adult patients with AIS admitted to Clínica Alemana de Santiago from August 2019 to July 2023.
Study inclusion criteria were: 1) patient with AIS between 6-24 hours from symptom onset, 2) NIHSS ≥ 6, 3) LVO of anterior circulation, 4) admission CT-Perfusion and CTA in arterial/delayed phase. Exclusion criteria: 1) incomplete data.
Image and interpretation protocol
The post-processing of CT-Perfusion images was performed in an automated way through RAPID© software, which considers a candidate for extended window endovascular therapy those patients whose ischemic core determined by CBF < 30% was not greater than 50 ml and the mismatch between Tmax > 6 sec/CBF < 30% volume ≥ 1.8.
CTA from supra-aortic trunks to vertex was performed in arterial and delayed phase at 35-50 seconds.
A vascular neurologist performed the estimation of CTA-SI ASPECTS in both phases at the time of data entry into the RECCA registry, which was done blind to the results of the perfusion study. A parallel evaluation of the CTA-SI was done by a neuroradiologist who was blind to both the clinical history and the results of the multimodal neuroimaging with automated processing. In case of a discrepancy, consensus could be reached by considering a third evaluation carried out by an external neuroradiologist.
Mismatch was considered when the difference between arterial arterial phase CTA (CTA-AP) ASPECTS and delayed phase CTA (CTA-DP) ASPECTS was ≥ |2| points (Figures 1 and 2).

Figure 1 Occlusion in M1 segment of the left middle cerebral artery. A and B correspond to the arterial phase. C and D correspond to the delayed phase with filling by leptomeningeal vessels in the M1-M2-M4 and M5 region of ASPECTS. Considering a significant mismatch, the patient underwent mechanical thrombectomy.
Statistical analysis
The normality of quantitative variables was evaluated through the Shapiro-Wilk test, using descriptive statistics to calculate the mean, standard deviation, median and interquartile range. Strength of association between continuous variables of the automated perfusion study and the CTA evaluation was assessed through Pearson’s correlation coefficient. In addition, the association between categorical variables of the automated study and visual assessment was assessed using Fisher’s exact test. To predict the outcome of a categorical variable of the perfusion study by logistic regression, all clinical and demographic characteristics at admission were used as independent variables, as well as the results of the CTA study. The data were processed with STATA version 17.0.
Results
During the study period, 22 patients met the inclusion criteria. The mean age was 77.8 years (range 48-94 years), the median NIHSS score was 15 (IQR 10-21) and the median time from symptom onset to CT was 11 hours (Tables 1 and 2). CTA-AP ASPECTS—CTA-DP ASPECTS mismatch was present in 14 of the 22 patients, with no discrepancy between vascular neurologist and neuroradiologist.
Table 1 Patients with CTA-AP ASPECTS—CTA-DP ASPECTS-mismatch. Baseline clinical and imaging characteristics (n = 14)
| Variable | Mean | Median | Interquartile range |
|---|---|---|---|
| Age | 78 | 78.5 | (70-86) |
| NIHSS admission | 15 | 14 | (6-22) |
| Time onset-CT | 12 | 11 | (6,5-19) |
| Core volume (CBF < 30%) | 25 | 17 | (7-31) |
| Critical Hypoperfusion (Tmax > 6 sec) | 125 | 112 | (51-174) |
| CTA-AP ASPECTS | 6 | 6 | (5-7) |
| CTA-DP ASPECTS | 8 | 9 | (7-10) |
NIHSS: National Institutes of Health Stroke Scale; ASPECTS: Alberta Stroke Program Early CT Score; CBF: cerebral blood flow; Tmax: time-to-maximum.
Table 2 Patients without CTA-AP ASPECTS—CTA-DP ASPECTS- mismatch. Baseline clinical and imaging characteristics (n = 8)
| Variable | Mean | Median | Interquartile range |
|---|---|---|---|
| Age | 78 | 82 | (71-89) |
| NIHSS admission | 17 | 19 | (10-24) |
| Time onset-CT | 11 | 11 | (7-16) |
| Core volume (CBF < 30%) | 118 | 117 | (47-187) |
| Critical Hypoperfusion (Tmax > 6 sec) | 160 | 203 | (51-225) |
| CTA-AP ASPECTS | 5 | 5 | (3-7) |
| CTA-DP ASPECTS | 6 | 6 | (4-8) |
NIHSS: National Institutes of Health Stroke Scale; ASPECTS: Alberta Stroke Program Early CT Score; CBF: cerebral blood flow; Tmax: time-to-maximum.
Pearson’s coefficient demonstrated a high correlation between ischemic core volume and CTA-DP ASPECTS with an inverse association of -0.93 p 0.0001 (Figure 3), and between Tmax ≥ 6 sec volume and CTA-AP ASPECTS with a value of -0.88 p 0.0001 (Figure 4).
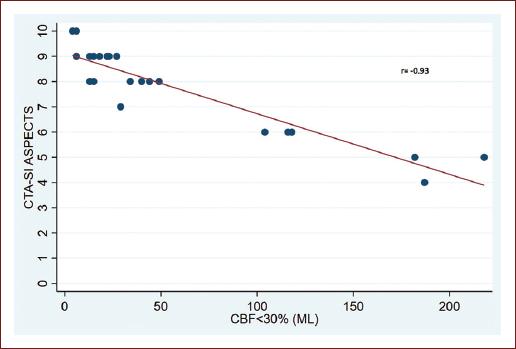
Figure 3 Scatter plot of Pearson’s correlation coefficient. A significant negative correlation between ischemic core volume (x-axis) and CTA-DP ASPECTS (y-axis).
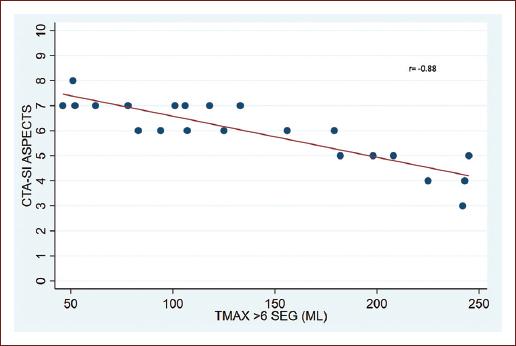
Figure 4 Scatter plot of Pearson’s correlation coefficient. A significant negative correlation between Tmax ≥ 6sec (x-axis) volume and arterial CTA-AP ASPECTS (y-axis).
There was a significant association between patient selection under DEFUSE 3 (Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke 3) criteria and the assessment of CTA-AP ASPECTS—CTA-DP ASPECTS mismatch with a p-value of 0.002. In addition, there was a direct relationship between the probability of being a candidate for MT by RAPID automated CT-Perfusion criteria and a higher CTA-SI ASPECTS value in delayed phase, with a perfect association for CTA-SI ASPECTS values ≥ 8.
Discussion
Hypoattenuation on CTA-SI has been evaluated qualitatively with CBF and CBV maps, demonstrating a higher correlation with CBF drop, suggesting a significant approximation to critically hypoperfused tissue12. Although, to date the association has only been made from CTA-SI in arterial phase and there is no data when it is compared with the volumetric values offered by the automated software. Adequate assessment of the volume of hypoperfused and infarcted tissue is essential for the selection of slow progressors13,14, who are potential beneficiaries of late-window endovascular therapy15. However, according to our results, the assessment of dual-phase CTA seems to be a semiquantitative tool comparable to the multimodal study with validated metrics.
CTA-DP ASPECTS showed a high approximation to what we consider nonviable tissue, with a 25th percentile on ASPECTS 7 appearing to be a possible lower limit for ischemic core on that quantitative score. Moreover, the CTA-SI in the arterial phase presented a high correlation with what we determined by imaging consensus as critical hypoperfusion, which includes viable tissue.
Therefore, these results provide information in the direction of the feasibility of choosing patients in extended window with imaging protocols with greater availability, shorter acquisition time and lower irradiation. In addition, it is possible that dispensing with CT-Perfusion could increase the number of patients who can benefit from TM, since there is growing evidence that advanced imaging studies lead to overselection16.
A clinical trial called MR CLEAN LATE was recently published, which aimed to evaluate the efficacy of extending the selection of patients for endovascular therapy beyond 6 hours based on the presence of collateral flow in the CTA. Although this trial demonstrated that endovascular treatment between 6 and 24 hours after symptom onset is safe and effective in patients with ischemic stroke due to occlusion of large vessels of the anterior circulation and any collateral arteries visible on CTA baseline, this study showed more benefits for patients with fewer collaterals and more clots, so stratification into degrees of collateral flow does not seem to be a useful strategy.
It seems essential to us to highlight that in the MR CLEAN LATE17, the median of NCCT ASPECTS of the endovascular group was 9 (interquartile range [IQR] = 7-10), which coincides with the median of CTA-DP ASPECTS of the group with arterial-delayed mismatch in our study.
Conclusions
In conclusion, dual-phase CTA could be used similar to CT-Perfusion and derive information on salvageable and non-salvageable tissue. It could also be used to select patients eligible for thrombectomy in the late time window, however, because of study limitations, these findings should be interpreted as preliminary and require replication.











 nova página do texto(beta)
nova página do texto(beta)



