Introduction
Attention deficit hyperactivity disorder (ADHD) is the most common neurodevelopmental disorder in the pediatric age group. This is a heterogeneous syndrome of multifactorial origin, characterized by moderate-to-severe distractibility, brief periods of attention, motor restlessness, emotional instability, and impulsivity1-4. It begins in childhood and up to 40-60% persists into adulthood, which affects psychosocial, school, and family functioning2. This has the prevalence in children of up to 41.1%, in adolescents and adults in 26.2%5. In Mexico, the prevalence is 14.6%3,6.
Executive functions are individual cognitive abilities that transform thoughts into decisions, plans, and actions. At least 4 functions are distinguished: Setting of objectives and planning, working memory, cognitive flexibility (task-switching ability), and inhibitory control. These altered functions characterize the patient with ADHD, and hinder family, school/work, and friendships social performance. It is frequently detected in the school because social interaction is evident in the group7-10.
The evaluation of executive functions is indispensable in the patient with suspicion or diagnosis of ADHD. It identifies strengths and opportunities to improve and allows to plan a psychobehavioral treatment with frequent evaluations of evolution10-13. The determining impact of ADHD on the quality of life (QOL) of children and adolescents is reflected in all areas of life and neurodevelopment13,14. This article evaluates the hypothesis about the correlation between cognition and QOL in children with ADHD.
The aim of this study was to describe the relationship between neuropsychological characteristics and QOL in children with ADHD in a second-level health care of the Mexican Social Security Institute in Puebla, Mexico.
Method
A prospective, analytical, and cross-sectional study was carried out. This work was approved by the Research Ethics Committee No. 21028 and the Local Health Research Committee No. 2102 of the Mexican Social Security Institute. All patients agreed to participate and their parents signed informed consent. They were given the possibility of not participating or leaving the study when they decided to do so. The individual results were given to the guardians and to the treating physicians. Personal data were handled with strict confidentiality.
Outpatients treated in a General Hospital of the Mexican Social Security Institute in Puebla, Mexico, were included. Patients were recruited with a diagnosis of ADHD established by neuropediatrician, (based on the criteria of the Diagnostic and Statistical Manual of Mental Disorders, fifth edition of the American Psychiatric Association DSM-5), of any gender, aged 6 to 12 years, who signed a letter of informed consent, and whose parents signed a letter of informed consent. Patients with visual or hearing impairment, severe delay in language development were excluded from this study. Those who did not complete the information and/or who requested to leave the study were eliminated from this study.
Patients who met the selection criteria received: Parental interview, and the Wechsler Intelligence Scale for Children IV (WISC-IV) and Neuropsi scales, which were applied by physicians trained for this purpose by neuropsychology.
The following instruments were applied:
− Interview with parents recording age, schooling, occupation, and behavioral disorders during childhood; about the patient: Perinatal history, time of diagnosis, sibling with ADHD, and treatment
− WISC-IV it is essential for the diagnosis of intellectual disability, learning disorders, autism spectrum, ADHD, and others, including differential diagnoses. This identifies global intellectual capacity, general abilities, and a specific profile in patients aged 6-16 years, at primary school level to the beginning of high school. It has excellent consistency (α-Cronbach = 0.93) and validity. It consists of 15 tests (10 main and 5 optional) through which a profile of scalar scores, a total intellectual quotient (IQ) and four indices (verbal comprehension, perceptual reasoning, working memory, and processing speed) are obtained. Scores in each domain can be: Very high (130 and above), superior (120-129), high average (110-119), average (90-109), low average (80-89), borderline (70-79), and extremely low (69 and below)15
− Neuropsi attention and memory third edition (Neuropsi). Evaluates the cognitive subprocesses of: Attention and executive functions, memory, and global attention and memory. It has a consistency of 0.89-1, a sensitivity of 93% and a specificity of 98%. It is standardized for the Mexican population. The values can be: High normal range (116 points and above), normal (85-115 points), mild-to-moderate disturbances (70-84 points), or severe disturbances (69 points or less)16,17
− Brief multidimensional life satisfaction scale for students (BMSLSS). Self-report consists of 6 questions exploring different environments: family, friends, residence, school, personal, and general. It is widely used in Spanish-speaking populations. It reports high consistency (α-Cronbach = 0.85) and high concordance with other life satisfaction measures and related variables. One of 3 life satisfaction scores is obtained: High, Medium, and Low. Life satisfaction was used as an indicator of QOL12,18.
Results
Of the 148 patients in control with the diagnosis, 104 accomplished inclusion criteria, representing 70%. They were 33 (31.73%) females and 71 (68.27%) males, aged 6-12 years, with a mean of 8.94 (SD = 1.83).
The most frequent values in the patients were (Table 1): Age 8-10 years; 2nd and 3rd gestation; 1st-2nd and 3rd-4th grade schooling; time since diagnosis less than 3 years; no siblings with ADHD; pharmacotherapy with methylphenidate. There were 51 (49%) patients born in the first half of the year, and 53 (51%) were born in the second half. Only 10 (9.61%) patients reported siblings with ADHD, and only 5 (5%) received psychotherapy. The main comorbidities were sleep disorders (69 patients, 66.34%), epilepsy (67, 64.42%), and gastroesophageal reflux disease (61, 58.65%).
Table 1 Patient characteristics (n = 104)
| Age (years) | |
| 6-7 | 29.80% |
| 8-10 | 50.00% |
| 11-12 | 20.19% |
| Pregnancy number | |
| 1º | 20.19% |
| 2º | 36.54% |
| 3º | 39.42% |
| 4º | 2.08% |
| 5º | 2.08% |
| Academic degree | |
| 1º-2º Elementary | 31.73% |
| 3º-4º Elementary | 34.61% |
| 5º-6º Elementary | 20.19% |
| 1º High school | 13.46% |
| Time to ADHDa Diagnosis (years) | |
| < 3 | 57.69% |
| 3-5 | 34.61% |
| > 5 | 7.69% |
| Pharmacological treatment | |
| MPDb | 77.88% |
| MPD+MVc | 14.42% |
| MPD+risperidone | 2.08% |
| MPD+sertraline | 2.08% |
| Oxybutinin | 2.08% |
| MV | 2.08% |
aADHD: attention deficit and hyperactivity disorder; bMPD: methylphenidate; cMV: magnesium valproate.
The most frequent values in mothers were (Table 2): Mean age 37 years, high school education, occupation homemakers, and behavioral disorders during childhood. For fathers: Age 38.56 years, high school, manual worker, and behavioral disorders in childhood.
Table 2 Characteristics of parents
| (n = 104) Father or tutor | (n = 104) Mother or tutor | |||
|---|---|---|---|---|
| Medium age (years) | 38.56 (±a 7.88 mínb 24, máxc 62) | 37.02 (± 7.81, mín 24, máx 69) | ||
| Academic degree | High school | 53.84% (n = 56) | High school | 44.23% (n = 46) |
| College | 22.11% (n = 23) | Secondary school | 29.80% (n = 31) | |
| Secondary school | 20.19% (n = 21) | College | 20.19% (n = 21) | |
| Does not live with the family | 3.84% (n = 4) | Elementary school | 5.76% (n = 6) | |
| Occupation | Manual worker | 60.57% (n = 63) | Housewife | 55.76% (n = 58) |
| Professional | 21.15% (n = 22) | Professional | 24.03% (n = 25) | |
| Did not answer | 14.42% (n = 15) | Manual worker | 20.19% (n = 21) | |
| No contribution to the family | 3.84% (n = 4) | |||
| Conduct disorders in childhood | 22.11% (n = 23) | 16.34% (n = 17) | ||
| Both 11.53% (n = 12) | ||||
a±: standard deviation;
bmín: minimum;
cmax: maximum
The most frequent findings in perinatal history were (Table 3) gestational risk: infections (frequently urinary), labor duration 8-10 and 12-19 h, apgar at 5 min 7-10, and in-hospital stay 0-3 days.
Table 3 Perinatal characteristics of patients (n = 104)
| History of gestational risk | |
| Infections | 54.80% |
| TA/TPTDa | 45.19% |
| Alcohol/smoking | 43.26% |
| Falls | 23.07% |
| Accidents | 3.84% |
| Other diseases | 4.80% |
| Birth care | |
| IMSSb | 48.07% |
| Particular means | 43.26% |
| Other public services | 8.65% |
| Length of labor | |
| 2-4 hc | |
| 5-7 h | 10.57% |
| 8-10 h | 29.80% |
| 12-19 h | 27.88% |
| 24-48 h | 3.84% |
| > 48 h | 8.65% |
| Pregnancy outcome | |
| Eutocic birth | 50% |
| Cesarean delivery | 50% |
| Apgar at 5 min | |
| 0-3 Bad | 27.61% |
| 4-6 Regular | 6.73% |
| 7-10 Good | 65.38% |
| In-hospital stay after birth | |
| 0-3 days | 77.88% |
| 4-10 days | 4.80% |
| 15 days or more | 17.30% |
aTA/TPTD: Threatened abortion/Threatened Preterm Delivery;
bIMSS: Mexican Social Security Institute;
ch: hours.
The WISC-IV categories with the highest percentage were (Fig. 1): in verbal comprehension: Average and very high; in perceptual reasoning: Average and high average; and in working memory, processing speed and IQ: Average and low average.
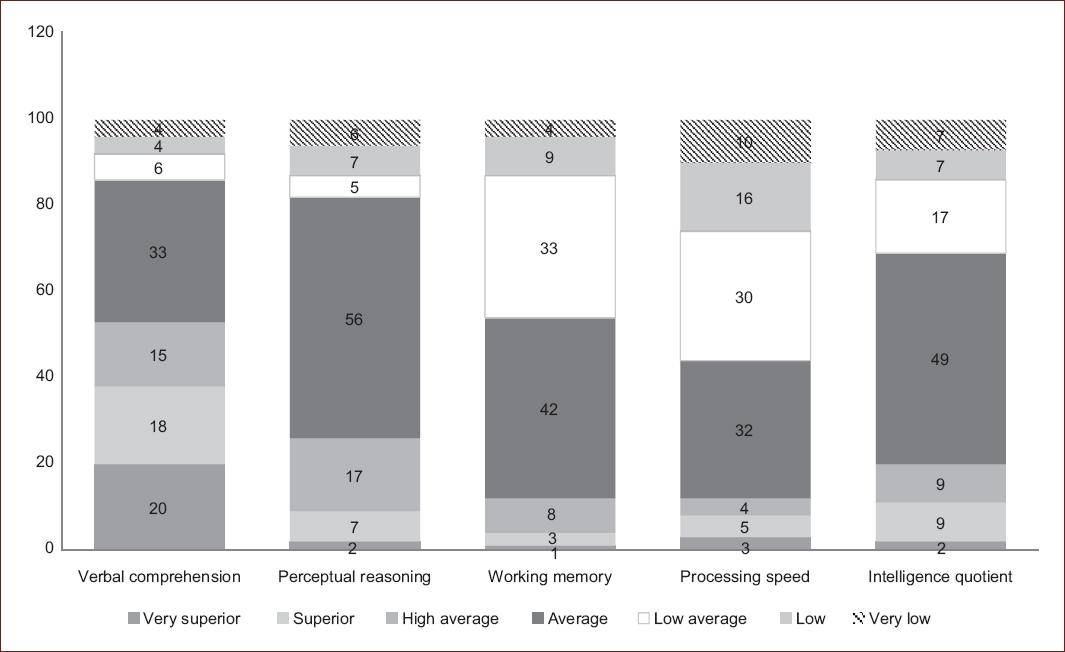
Figure 1 Cognitive characteristics (WISC-IV) in children with attention deficit hyperactivity disorder.Scores in percentages of children on the Wechsler Intelligence Scale for Children IV (WISC-IV). n = 104.
In Neuropsi, moda in the 3 domains (attention and executive functions, memory, and attention and memory) were the categories normal and mild alterations (Fig. 2).

Figure 2 Cognitive characteristics (Neuropsi) in children with attention deficit hyperactivity disorder.Results in percentages of patients in the Neuropsi Attention and Memory test 3rd ed (Neuropsi). n = 104.
The BMSLSS results are detailed in figure 3. The highest frequencies were reported in the HorribleSad responses. The most frequent life satisfaction was low (59.61%), followed by medium (31.73%), and high (8.65%).
The correlation between IQ (WISC-IV) and life satisfaction (BMSLSS) was r = 0.3962 (p < 0.001). The correlation between attention and memory (Neuropsi) and life satisfaction (BMSLSS) was r = 0.451 (p = 0.018).
Discussion
The prevalence of ADHD is high and progressive, and affects the cognitive performance of the carrier. Reports of cognitive characteristics in Mexico and Latin America with large samples are scarce13,18,19. In this study, the behavioral history of the parents, the most frequent diagnosis in 8-10 years, 3 years of evolution or less, and the management with methylphenidate are in agreement with other reports3,5,8-10,13,20,21. Some particularities differ from other reports: Less than 10% of siblings carriers of ADHD, and no differences in the demand for attention according to the semester of birth. This finding opposes to suggestions about the heritability near 75-80%, and about risks of misdiagnosis depending of the month of birth4,22. This confirms the role of the social-environmental context to develop this disorder.
Methylphenidate is the cornerstone in the treatment of ADHD, and improves QOL. Other pharmacological options are atomoxetine, lisdexamfetamine, and guanfacine. Treatment with oxybutynin, valproate, risperidone, and sertraline in this study indicates the broad spectrum of comorbidities20.
The presence of perinatal factors and childhood behavioral characteristics and disturbances in fathers and mothers in the present work represents the opportunities for prevention. The existence of more than one risk factor in several patients increases the possibility of neurological dysfunction, clinical variability, and vulnerability to ADHD. Youth, schooling, and parental occupation are conditions to be considered for comprehensive management1,3,5,12,21.
The higher prevalence of low mean and borderline scores in working memory and processing speed (WISC-IV), and attention and memory (Neuropsi) in this study is noteworthy. The ability to learn and transforming thoughts into actions starts with attention, is fixed with memory, and supports processing, including inhibition of impulsivity. These cognitive deficits are fundamental in ADHD. The importance of verbal comprehension/expression in this disorder is also established by other reports. The specific role of perceptual reasoning and other executive functions and their combinations remains to be investigated8,9,13,17,21.
In these patients, assessing the functional alteration of the individual and the results of the treatment is an essential and not only as symptomatological reduction. QOL is used for this purpose since the results in the physical, emotional, social, and cognitive dimensions are similar regardless of the instruments used to assess it23,24.
There are few studies in Mexico about QOL and cognition in patients with ADHD. In this study, life satisfaction was used as an indicator of QOL, as well as previous reports12,17. Pharmacotherapy generally improves the perception of QOL in these patients20,23,24. Despite all patients in this study receiving pharmacotherapy, 95% were not receiving psychotherapy in this study, and most reported low life satisfaction. This is alarming, and underscores the importance of combined drug and psychological treatment.
The lowest scores occurred in school, followed by friendships and housing, corresponding with reports from Latin America and Spain12,17,23-25. This is related to difficulties in the recognition of facial expressions and own and other people's emotions, which are essential skills for social relationships11,13,25,26. These deficits explain why children with ADHD perceive social rejection and poor acceptance by their peers10,27.
On the other hand, they may rate their cognitive and social competencies more positively than they actually do, which explains why the family environment and self-satisfaction received better evaluation12,27.
The IQ measured with WISC-IV is not an absolute parameter, it serves as a reference and patient labeling should be avoided. Although psychotherapy does not substantially modify it, it can optimize the evaluation score10,13. Like Neuropsi, it registered a moderate correlation with life satisfaction, both highly significant.
Only 5 patients of the sample (4.8%) received psychotherapy. Neuropsychological evaluation refines the diagnosis of the patient with ADHD, and behavioral follow-up is indispensable in comprehensive management. Psychoeducation and cognitive behavioral therapy optimize the performance of executive functions, self-esteem, and self-satisfaction. They support resilience and social performance, and decrease the probability of dissocial behaviors and future addictions10,13,17,19.
Although the present study is one of the largest samples among similar studies in this region3,9,13,17,19, it is still a limited population. Studies with more patients and multicenter studies are required to strengthen the conclusions. Another limitation is the omission of personal dimensions such as family functionality and/or parental characteristics, schools, and others.
Conclusions
Attention, memory, and processing speed are the cognitive characteristics most affected in children with ADHD. QOL is low, especially in school and friendship contexts. Psychobehavioral care strategies, together with pharmacotherapy, are essential to improve the patient's health status and prognosis.











 nueva página del texto (beta)
nueva página del texto (beta)



